Published online Oct 28, 2010. doi: 10.3748/wjg.v16.i40.5118
Revised: June 29, 2010
Accepted: July 6, 2010
Published online: October 28, 2010
AIM: To investigate the resistance of Helicobacter pylori (H. pylori) to 6 commonly used antibiotics from 2000 to 2009 in Shanghai.
METHODS: A total of 293 H. pylori strains were collected from 2000 to 2009 in Shanghai and tested for their susceptibility to metronidazole, clarithromycin, amoxicillin, furazolidone, levofloxacin and tetracycline using agar dilution.
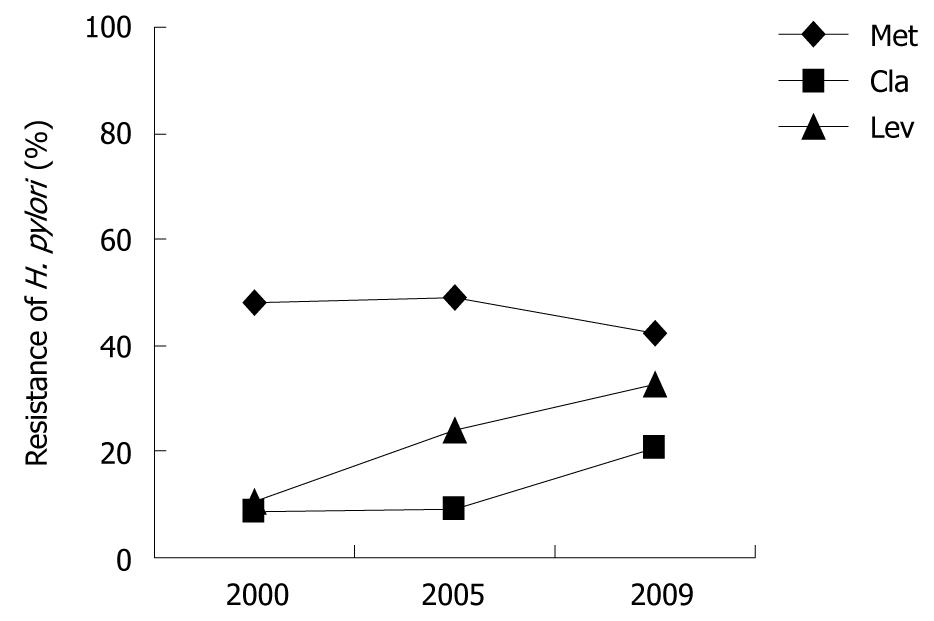
RESULTS: The resistant rates of H. pylori to clarithromycin (8.6%, 9.0% and 20.7%) and levofloxacin (10.3%, 24.0% and 32.5%) increased from 2000 to 2009 in Shanghai. The resistant rate of H. pylori to metronidazole remained stable (40%-50%). Only one strain of H. pylori isolated in 2005 was resistant to tetracycline. All strains were sensitive to amoxicillin and furazolidone. The resistant rate of H. pylori to antibiotics was not related with the sex, age and clinical outcome of patients.
CONCLUSION: Resistance of H. pylori to antibiotics plays an important role in making treatment strategies against H. pylori-associated diseases.
-
Citation: Sun QJ, Liang X, Zheng Q, Gu WQ, Liu WZ, Xiao SD, Lu H. Resistance of
Helicobacter pylori to antibiotics from 2000 to 2009 in Shanghai. World J Gastroenterol 2010; 16(40): 5118-5121 - URL: https://www.wjgnet.com/1007-9327/full/v16/i40/5118.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i40.5118
Chronic gastritis, peptic ulcer, gastric adenocarcinoma, and mucosa-associated lymphoid tissue lymphoma can be relieved or even cured after eradication of Helicobacter pylori (H. pylori)[1,2]. Although triple therapy with proton pump inhibitor (PPI), amoxicillin and clarithromycin or metronidazole is still recommended, it should only be used when the local prevalence of resistance of H. pylori to antibiotics is below a certain level[3]. Recently, levofloxacin, tetracycline and furazolidone have been recommended in primary and/or rescue therapies in some areas. Resistance of H. pylori to antibiotics is the main reason for the failure of therapies for H. pylori-associated diseases. Since the initial eradication of H. pylori can no longer be achieved due to its increasing resistance to antibiotics, it is necessary to investigate the local resistance of H. pylori to antibiotics for choosing the effective therapy for H. pylori-associated diseases.
Clinical H. pylori strains were isolated from 293 patients who visited Renji Hospital (Shanghai, China) for dyspeptic symptoms in 2000, 2005 and 2009. Their dyspeptic symptoms included abdominal pain, abdominal distention, eructation, nausea, sour regurgitation and disgorging. Patients who used antibiotics, bismuth, H2-receptor antagonist (H2RA) or PPI for H. pylori in the past month, or administered non-steroidal anti-inflammatory drugs and alcohol, were excluded from the study. A total of 293 patients (male: 182, female: 111), enrolled in this study, were diagnosed as gastritis, peptic ulcer and gastric cancer, respectively, by endoscopy. All patients gave their written informed consent for participation in the study.
One biopsy was taken from the antrum of each patient for H. pylori culture. The biopsy specimens were cultured with a brain heart infusion (BHI) agar medium (OXOID, Basingstoke, UK) containing 5% defibrinated sheep blood under microaerophilic conditions (85% N2, 10% CO2 and 5% O2) at 37°C. All stocks were kept in BHI broth (Difco Laboratory, Detroit, MI, USA) supplemented with 30% glycerol at -80°C. Clinical H. pylori strains were identified when the tests and Gram staining were positive for urease, oxidase, and catalase.
Minimal inhibitory concentration (MIC) of metronidazole (Met), clarithromycin (Cla), amoxicillin (Amo), levofloxacin (Lev), tetracycline (Tet) and furazolidone (Fur), was measured with the two-fold agar dilution method. H. pylori strains were suspended in saline and detected with a spectrophotometer. The bacterial suspensions (108 colonies per milliliter) were then plated onto agar plates containing various concentrations of the above antibiotics with an inoculator (Sakuma Seisaku, Tokyo, Japan). Three days after microaerophilic incubation, MIC was defined as the lowest drug concentration that prevented visible growth of the bacteria. ATCC43504 was used as a quality control. Met > 8 μg/mL, Cla > 2 μg/mL, Lev > 2 μg/mL, Amo > 8 μg/mL, Tet > 2 μg/mL and Fur > 2 μg/mL were determined as resistance breakpoints as previously described[4,5]. Antibiotics and their solvents used in this study are shown in Table 1.
| Antibiotic | Manufacturer | Solvent |
| Metronidazole, Met | Wuhan Pharmaceutical Ltd. | Distilled water |
| Clarithromycin, Cla | Livzon Syntpharm Co., Ltd. | Acetone |
| Levofloxacin, Lev | Livzon Syntpharm Co., Ltd. | Distilled water |
| Tetracycline, Tet | SIGMA-ALDRICH Co., Ltd. | 0.1 mol/L phosphate buffer saline (pH 6.0) |
| Amoxicillin, Amo | Kunming Baker Norton Pharmaceutical Ltd. | 0.1 mol/L phosphate buffer saline (pH 6.0) |
| Furazolidone, Fur | Shenzhen Jiangmen Pharmaceutical Ltd. | N,N-dimethylformamid (DMF) |
Data were analyzed by chi square test using SPSS13.0. P < 0.05 was considered statistically significant.
The demographic data about the patients are shown in Table 2. No significant difference was observed in background of the patients.
| 2000 | 2005 | 2009 | |
| No. of strain | 58 | 100 | 135 |
| Male/Female | 46/12 | 61/39 | 75/60 |
| Age (average, range) | 44.3 (20-78) | 45.2 (18-81) | 42.5 (20-74) |
| Gastritis/Ulcer/Gastric cancer | 36/20/2 | 46/44/10 | 81/53/1 |
No significant difference was observed in the resistance rate of H. pylori to metronidazole during the past 10 years (28/58 in 2000, 49/100 in 2005 and 57/135 in 2009). The resistance rate of H. pylori strains isolated in 2009 to clarithromycin was 20.7% (28/135), which was significantly higher than that of H. pylori strains isolated in 2000 (8.6%, 5/58) and 2005 (9.0%, 9/100) (P < 0.05). The resistance rate of H. pylori strains to levofloxacin was higher in 2009 (32.6%, 44/135) than in 2005 (24.0%, 24/100) (P < 0.05), and the resistant rate of H. pylori strains to levofloxacin was significantly higher in 2005 (24.0%, 24/100) than in 2000 (10.3%, 6/58) (P < 0.05). No H. pylori strain was resistant to amoxicillin and furazolidone and only one H. pylori strain isolated in 2005 was resistant to tetracycline. No significant difference was observed in gender and age of the patients and in antibiotic resistance-associated diseases (Figure 1).
Multidrug resistance means that one strain is resistant to two or more antibiotics. In this study, the multidrug resistance of H. pylori was 27.9% (36/129) in 2009, which was significantly higher than that (10.3%, 6/58) of H. pylori in 2000 (P < 0.05). The multidrug resistance of H. pylori to metronidazole and levofloxacin was the highest (43.1%, 25/58), followed by the combination of metronidazole/levofloxacin and metronidazole/clarithromycin with a resistance rate of 24.1% (14/58).
The resistance of H. pylori to metronidazole has been increasing in Shanghai since 1990s. The resistant rate of H. pylori has increased from 42% in 1995 to 70% in 1999[6,7]. In this study, agar dilution showed that the resistance of H. pylori to metronidazole was slightly decreased in recent years[8], but was still higher than 40%. According to the Maastricht III Consensus Conference report, in an area with a resistance rate of H. pylori to metronidazole of over 40%, the efficacy of triple therapy with metronidazole may decrease. However, the eradication rate of H. pylori for metronidazole-containing therapy can be improved by increasing its dosage, prolonging its duration or adding bismuth salts[9-11].
It has been shown that triple therapy with clarithromycin is the first choice of treatment for eradication of H. pylori with an ITT rate of over 90%[12]. However, the resistance of H. pylori to clarithromycin has been increasing all over our country[13]. For example, the resistance of H. pylori to clarithromycin was 10% in 1999 and 36% in 2005 in Beijing[14], and 0% in 1995 and 10% in 1999 in Shanghai[6]. In this study, the resistance of H. pylori to clarithromycin was 8.6% in 2000, 9.0% in 2005 and 20.7% in 2009, respectively. The guidelines recommend that if the resistance of H. pylori to clarithromycin is over 15%-20%, therapies with clarithromycin should not be used as an empirical treatment. However, therapies with combined clarithromycin and bismuth can improve the bactericidal activity of clarithromycin[10].
Levofloxacin, a new broad-spectrum antibiotic with a strong antimicrobial activity, has been used in eradicating H. pylori in recent years. The guidelines suggest that levofloxacin-containing therapies as the first-line therapy and rescue therapy have good efficacy. However, it was reported that the resistance of H. pylori to levofloxacin is high in many areas (29.1% in Beijing and 21.7% in Xi’an)[15]. In the present study, the resistance rate of H. pylori to levofloxacin in Shanghai was 10.3% in 2000, 24.0% in 2005 and 32.6% in 2009, respectively, indicating that eradication of H. pylori may fail when its resistance to levofloxacin is over 20% and that levofloxacin should not be used in treatment of H. pylori when susceptibility test is not performed[16,17].
Antimicrobial susceptibility testing is an effective method that tests if H. pylori strains are resistant to some antibiotics. Romano et al[18] showed that antimicrobial susceptibility testing before treatment improves the rate of response to therapy and is cost-saving. However, this testing cannot be done in large areas because the culture of H. pylori is very costly.
In this study, the resistance of H. pylori to metronidazole in Shanghai was over 40%, which showed a decreasing trend. The resistance rate of H. pylori to clarithromycin was 20.7% in 2009 which was on the warning level. The resistance of H. pylori to levofloxacin has increased rapidly in the past 10 years with a resistant rate of 30.7% in 2009. Almost all H. pylori strains were not resistant to amoxicillin, furazolidone and tetracycline, indicating that these antibiotics may become good candidates against H. pylori. Treatment strategies should be made and changed according to the resistance of H. pylori to antibiotics. Further study is needed in more centers.
Many alimentary diseases are associated with Helicobacter pylori (H. pylori) infection. The resistance of H. pylori to antibiotics is increasing as the spreading of eradication treatment and is the main reason for the failure of H. pylori eradication. The authors need to know the local area resistance rate of H. pylori to antibiotics in different places and treatment strategies should be made according to antimicrobial susceptibility testing.
The resistance of H. pylori to 6 antibiotics from 2000 to 2009 in Shanghai was studied, which may help us chose antibiotics for eradication of H. pylori.
This study showed the resistance rates of H. pylori to 6 antibiotics from 2000 to 2009 in Shanghai and highlighted the importance of the resistance of H. pylori to antibiotics in making treatment strategies against H. pylori.
The resistance rate of H. pylori to metronidazole, clarithromycin, amoxicillin, furazolidone, levofloxacin and tetracycline from 2000 to 2009, shown in the present study, may help the clinicians carry out experiential therapies.
In this manuscript, the authors reported the resistance pattern of H. Pylori to six antibiotics from 2000 to 2009 in Shanghai and highlighted the importance of the resistance of H. pylori to antibiotics in making treatment strategies against H. pylori, which may help the clinicians carry out experiential therapies for H. pylori-associated diseases.
Peer reviewers: Dr. Fritz Francois, Assistant Dean for Academic Affairs and Diversity, Assistant Professor of Medicine, New York University School of Medicine, 423 E. 23rd St. Room 1132N, New York, NY 10010, United States; Marco Romano, MD, Professor, Dipartimento di Internistica Clinica e Sperimentale-Gastroenterologia, II Policlinico, Edificio 3, II piano, Via Pansini 5, 80131 Napoli, Italy
S- Editor Wang YR L- Editor Wang XL E- Editor Ma WH
| 1. | Huang JQ, Hunt RH. Review article: Helicobacter pylori and gastric cancer--the clinicians’point of view. Aliment Pharmacol Ther. 2000;14 Suppl 3:48-54. |
| 2. | Sipponen P, Kosunen TU, Valle J, Riihelä M, Seppälä K. Helicobacter pylori infection and chronic gastritis in gastric cancer. J Clin Pathol. 1992;45:319-323. |
| 3. | Malfertheiner P, Megraud F, O’Morain C, Bazzoli F, El-Omar E, Graham D, Hunt R, Rokkas T, Vakil N, Kuipers EJ. Current concepts in the management of Helicobacter pylori infection: the Maastricht III Consensus Report. Gut. 2007;56:772-781. |
| 4. | Godoy AP, Ribeiro ML, Benvengo YH, Vitiello L, Miranda Mde C, Mendonça S, Pedrazzoli J Jr. Analysis of antimicrobial susceptibility and virulence factors in Helicobacter pylori clinical isolates. BMC Gastroenterol. 2003;3:20. |
| 5. | Liang X, Liu W, Xu WW, Xiao SD. Study on the resistance of Levofloxacin to Helicobacter pylori. Weichangbinxue. 2007;12:589-592. |
| 6. | Shi T, Liu WB, Xiao SD, Xu WW. Antibiotic resistance in Shanghai. Zhonghua Neike Zazhi. 2000;39:576. |
| 7. | Osato MS, Reddy R, Reddy SG, Penland RL, Graham DY. Comparison of the Etest and the NCCLS-approved agar dilution method to detect metronidazole and clarithromycin resistant Helicobacter pylori. Int J Antimicrob Agents. 2001;17:39-44. |
| 8. | Liang X, Liu WB, Lu H, Xu WW, Xiao SD. Helicobacter pylori: in vitro induction of resistance to antibiotics and surveillance of its resistant prevalence. Zhonghua Xiaohua Zazhi. 2003;23:146-149. |
| 9. | Zheng Q, Dai J, Li XB, Lu H, Xiao SD. Comparison of the Efficacy of Pantoprazole· based Triple Therapy Versus Quadruple Therapy in the Treatment of Helicobacter pylori Infection: A Single-center, Randomized, Open and Parallel-controlled Study. Weichangbingxue. 2009;14:8-11. |
| 10. | Wolle K, Malfertheiner P. Treatment of Helicobacter pylori. Best Pract Res Clin Gastroenterol. 2007;21:315-324. |
| 11. | Marshall BJ, Warren JR. Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet. 1984;1:1311-1315. |
| 12. | Xuan SH, Zhou YG, Wang HM. Advance in Helicobacter pylori resistance to clarithromycin. Shijie Huaren Xiaohua Zazhi. 2008;16:3060-3064. |
| 13. | Hao Q, Li Y, Zhang ZJ, Liu Y, Gao H. New mutation points in 23S rRNA gene associated with Helicobacter pylori resistance to clarithromycin in northeast China. World J Gastroenterol. 2004;10:1075-1077. |
| 14. | Hu F. Antibiotic resistance status of H. pylori in China. In 7th China-Korea-Japan Joint Conference on Helicobacter infection. Febury21-22, 2008, The Westin Miyako Hotel, Kyoto, Japan 31. . |
| 15. | Hu FL. Antibiotic resistance status of H. pylori in China. Weichangbingxue He Ganbingxue Zazhi. 2008;17:517-518. |
| 16. | Bilardi C, Dulbecco P, Zentilin P, Reglioni S, Iiritano E, Parodi A, Accornero L, Savarino E, Mansi C, Mamone M. A 10-day levofloxacin-based therapy in patients with resistant Helicobacter pylori infection: a controlled trial. Clin Gastroenterol Hepatol. 2004;2:997-1002. |
| 17. | Branca G, Spanu T, Cammarota G, Schito AM, Gasbarrini A, Gasbarrini GB, Fadda G. High levels of dual resistance to clarithromycin and metronidazole and in vitro activity of levofloxacin against Helicobacter pylori isolates from patients after failure of therapy. Int J Antimicrob Agents. 2004;24:433-438. |
| 18. | Romano M, Marmo R, Cuomo A, De Simone T, Mucherino C, Iovene MR, Montella F, Tufano MA, Del Vecchio Blanco C, Nardone G. Pretreatment antimicrobial susceptibility testing is cost saving in the eradication of Helicobacter pylori. Clin Gastroenterol Hepatol. 2003;1:273-278. |