CASE REPORT
A 38-year-old woman was referred to our outpatient clinic for biopsy-proven adenocarcinoma of the stomach. The patient had no significant medical history. On gastroduodenoscopic examination, type IIc early gastric cancer was found at the lesser curvature of the body. Moderately differentiated adenocarcinoma was confirmed by performing a biopsy of the lesion. Staging work-up including abdominal computed tomography (CT) revealed no metastasis.
Radical subtotal gastrectomy with Billroth II reconstruction, including complete dissection of the perigastric nodes plus the lymph node along the left gastric and hepatic arteries, was performed. The lesser curvature of the stomach and the duodenal stump were closed with staples. Antecolic, isoperistatic gastrojejunostomy was performed using Albert-Lembert sutures. A nasogastric tube was placed in the remnant stomach.
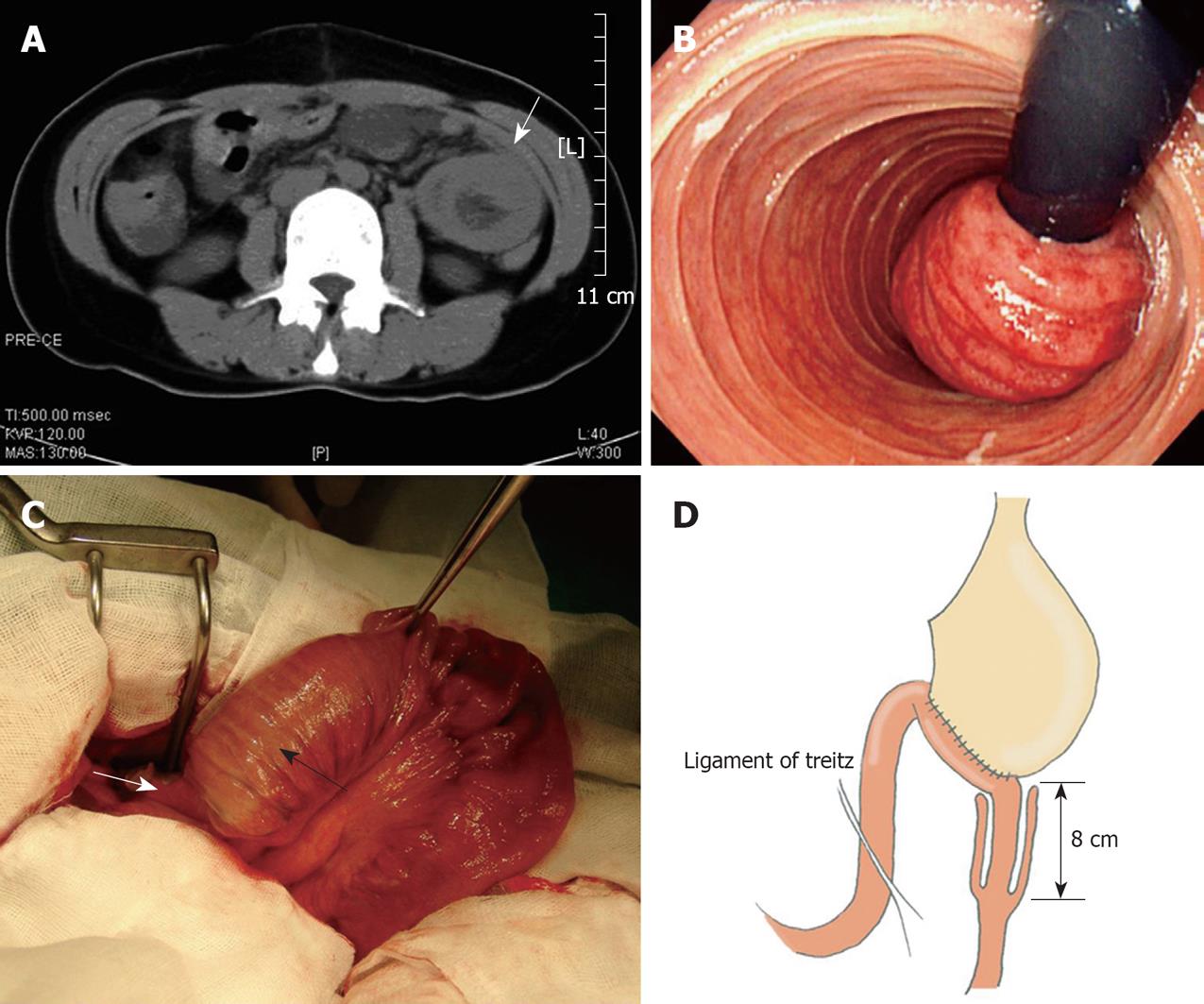
On the first postoperative day (POD), the patient did not complain of abnormal symptoms. However, on POD 2, she started to complain of recurrent episodes of abdominal colicky pain, which did not subside for over 5 d, without a definite cause. During that time, 500-900 mL bile-containing gastric juice was drained via the nasogastric tube daily. Serial plain abdominal radiography and laboratory tests showed no remarkable findings. The blood tests were unremarkable except for elevated white blood cell count up to 16 000/μL. On POD 6, the patient complained of intermittent abdominal cramping, and abdominal tenderness in the left upper quadrant of the abdomen on physical examination. Non-enhanced CT was carried out and revealed a non-homogeneous jejunal mass below the anastomosis site (Figure 1A). Gastrofibroscopic examination was performed subsequently. The entrance of the efferent loop was narrow and edematous, but the gastro-fibroscope was able to pass through the efferent loop. A congested jejunal mass was observed on the J-turn image (Figure 1B). Emergency laparotomy was performed, on suspicion of a jejunojejunal intussusception.
Figure 1 Radiologic, endoscopic and intraoperative findings of anterograde jejunojejunal intussusception.
A: Abdominal computed tomography showed a non-homogeneous mass (arrow) in the left upper quadrant of the abdomen; B: A J-turn view of gastrofibroscopic examination demonstrated a congested jejunal mass (intussusceptum); C: Intraoperative findings revealed that the intussusception started just below the gastrojejunostomy anastomosis. The black arrow indicates the intussuscipiens, and the white arrow indicates the intussusceptum; D: Schematic diagram of the intussusception at the efferent-loop.
On exploration, an anterograde jejunojejunal intussusception was found at about 5 cm distal to the gastrojejunostomy anastomosis line (Figure 1C and D). Manual reduction was performed carefully and the intussusception came loose subsequently. The proximal jejununal segment (intussusceptum), about 8 cm in length, did not recover from ischemia. The primary gastrojejunostomy anastomosis, which was non-viable, was removed, and a Roux-en-Y gastrojejunostomy was formed. On pathological examination, no identifiable leading point for the intussusception was present. She was discharged without further complications or abnormal symptoms on POD 11 after the second operation.
DISCUSSION
Intussusception is primarily a disease of infancy and childhood, and only about 5% of cases occur in adults[3]. Although childhood intussusception is idiopathic in 90% of cases, adult intussusception has an organic lesion as a leading cause in 70%-90% of cases, and > 50% of the lesions have been reported to be malignant[4,5].
Although postoperative intussusception is a rare clinical entity in both age groups, it is also more common in the pediatric population than in adults. It accounts for 5%-10% of cases of postoperative ileus in infancy and childhood[6], and only 1% of cases in adults[7].
Intussusception is an extremely rare complication after gastric surgery; the incidence is reported to be < 0.1%[1]. Since the first case of jejunogastric intussusception after gastrojejunostomy was reported by Bozzi[8] in 1914, a large number of isolated cases have been reported, and fewer than 200 cases of postoperative intussusception after gastric surgery have been reported in the English-language literature[2]. Retrograde jejunogastric intussusception is the most common type after gastric surgery[9]. Rarer cases of jejunojejunal[10-14], jejunoduodenal[15] or duodenogastric intussusception[16], or intussusception through a Braun anastomosis[17] also have been reported after gastric surgery.
All cases of jejunojejunal intussusception have been observed after Roux-en-Y gastro- or esophagojejunostomy. To the best of our knowledge, this is the first case report of jejunojejunal intussusception after partial gastrectomy with Billroth II type gastrojejunostomy. However, it should be pointed out that jejunojejunal intussusception might not be such a rare problem after Roux-en-Y gastric bypass for morbidly obese patients[18]. Simper et al[18] recently have reported 22 cases (0.15%) of postoperative jejunojejunal intussusception after more than 15 000 Roux-en-Y gastric bypasses.
In the present case, neither functional nor mechanical causes were identified as leading causes of intussusception. Although most adult intussusceptions are caused by a definable structural lesion[5], definite anatomical or pathological causes are rarely found in cases following gastric surgery[2]. A variety of postoperative conditions, such as adhesions around the suture lines[3,19], a long intestinal tube[20], increased intra-abdominal pressure[1], shortening of the jejunal mesentery[21], and reverse peristalsis[19,22], have been proposed as possible mechanisms of intussusception after gastric surgery, but none has been confirmed. Functional causes include reverse peristalsis, which is triggered by an anastomosed jejunal loop being irritated by hydrochloric acid, and atonic stomach, which is caused by vagotomy[2].
Diagnosis of postoperative intussusception is difficult in adults. The classic symptom triad of intussusception (pain, palpable mass, and currant-jelly stool) rarely occurs in adults[3]. Furthermore, usual symptoms encountered in acute postoperative intussusception are easily confused with postoperative ileus or adhesion[23,24]. For these reasons, diagnosis was delayed in our case, which rapidly progressed to incarceration and strangulation of the involved efferent limb. Thus, a high index of clinical suspicion is necessary for early diagnosis of this potentially lethal complication. Upper gastrointestinal endoscopy and abdominal CT are highly diagnostic in the setting of urgent, high-level intestinal obstruction[25].
Endoscopic reduction of jejunogastric intussusception has been suggested in a few selected cases[26]; however, this is associated with a significant risk of recurrence[27]. Surgery is the mainstay of treatment in jejunojejunal intussusception, and should be individualized for each patient. Surgical procedures include reduction, resection, and revision of the intussusception and takedown of the previous anastomosis with construction of a new anastomosis, depending on the operative findings. If the affected segment loses viability, resection of the non-viable segment is inevitable. Ozdogan et al[13] have suggested that the operation should be conservative, provided that the bowel is viable; manual reduction is the only required treatment, and other preventive measures are not necessary.
We report a case of anterograde jejunojejunal intussusception that caused acute efferent loop syndrome after partial gastrectomy. Acute jejunojejunal intussusception after gastric surgery is an extremely rare clinical entity that requires a high index of clinical suspicion for early diagnosis and prompt surgical management. Thus, intussusception should be considered as one of the possible causes of high-level intestinal obstruction in the immediate postoperative period after partial gastrectomy.