Published online May 14, 2010. doi: 10.3748/wjg.v16.i18.2311
Revised: February 8, 2010
Accepted: February 15, 2010
Published online: May 14, 2010
This recipient with situs inversus totalis (SIT) was a 60-year-old female who had hepatitis B-related end-stage liver disease. Preoperative donor evaluation showed that the right posterior section satisfied graft volume and was space-fitting in the recipient hepatic fossa when it was rotated 180 degrees. The operation and postoperative course progressed satisfactorily. Three weeks after living donor liver transplantation (LDLT), the graft function was disturbed by compression of bottom-placed right hepatic vein. This was treated with a vascular stent and subsequently the graft function was normalized. The present case shows that LDLT for patients with SIT using a right posterior section graft is feasible.
- Citation: Kim BW, Bae BK, Xu W, Wang HJ, Kim MW. Living donor liver transplantation for an adult patient with situs inversus totalis. World J Gastroenterol 2010; 16(18): 2311-2313
- URL: https://www.wjgnet.com/1007-9327/full/v16/i18/2311.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i18.2311
Situs inversus totalis (SIT) is a rare congenital anomaly with complete reversal of all visceral organs. It occurs once in about 15 000 to 20 000 births and has unknown cause. Sometimes SIT is associated with other anomalies such as biliary atresia, visceral vascular anomaly, and polysplenia. In general, most people with SIT have no complications and perform normal physical activities. However, this condition could be a serious problem when he/she needs liver transplantation because the liver has asymmetrical anatomy that causes technical difficulties in graft positioning and vascular anastomoses in the SIT recipient. For this reason, it has been regarded as a contraindication to liver transplantation.
There are some technical reports of whole graft liver transplantation for adult SIT recipients[1-3]. Also, cases of living donor liver transplantation (LDLT) for the adult patient with SIT have been reported using the left or right lobe with midline positioning of the graft[4,5]. However, midline positioning in the SIT recipient may present two major concerns. Firstly, graft displacement due to redundant space of recipient’s hepatic fossa could result in vascular torsion and kinking; and secondly, the recipient’s inferior vena cava could be compressed by the graft. To overcome these problems, we performed reversed orthotopic implantation using right posterior section, Couinaud segment VI + VII, grafted into the recipient’s hepatic fossa[6].
Our recipient was a 60-year-old female with advanced liver cirrhosis caused by hepatitis B virus. Her body weight was 60 kg and the Model for End-stage Liver Disease (MELD) score was 19. The donor was her nephew, a 45-year-old male with a suitable volume of right posterior sector on preoperative computed tomography (CT) scan. Preoperative CT scan showed hilar trifurcation of portal vein and measurement of total liver volume (TLV) was 1100 mL. The right liver volume of the donor was 780 mL (71% of TLV), the left lobe volume was 320 mL, and the right posterior section volume was 510 mL (46.4% of TLV). A right posterior section graft was the only suitable type of donor hepatectomy to ensure donor safety and appropriate volume of graft to the recipient. Preoperative measurement of the right posterior section graft to recipient weight ratio (GRWR) was 0.85%. Preoperative simulation showed that the donor’s right posterior section fit well into the recipient’s left subphrenic space with 180-degree flip-over (facing backward) implantation method.
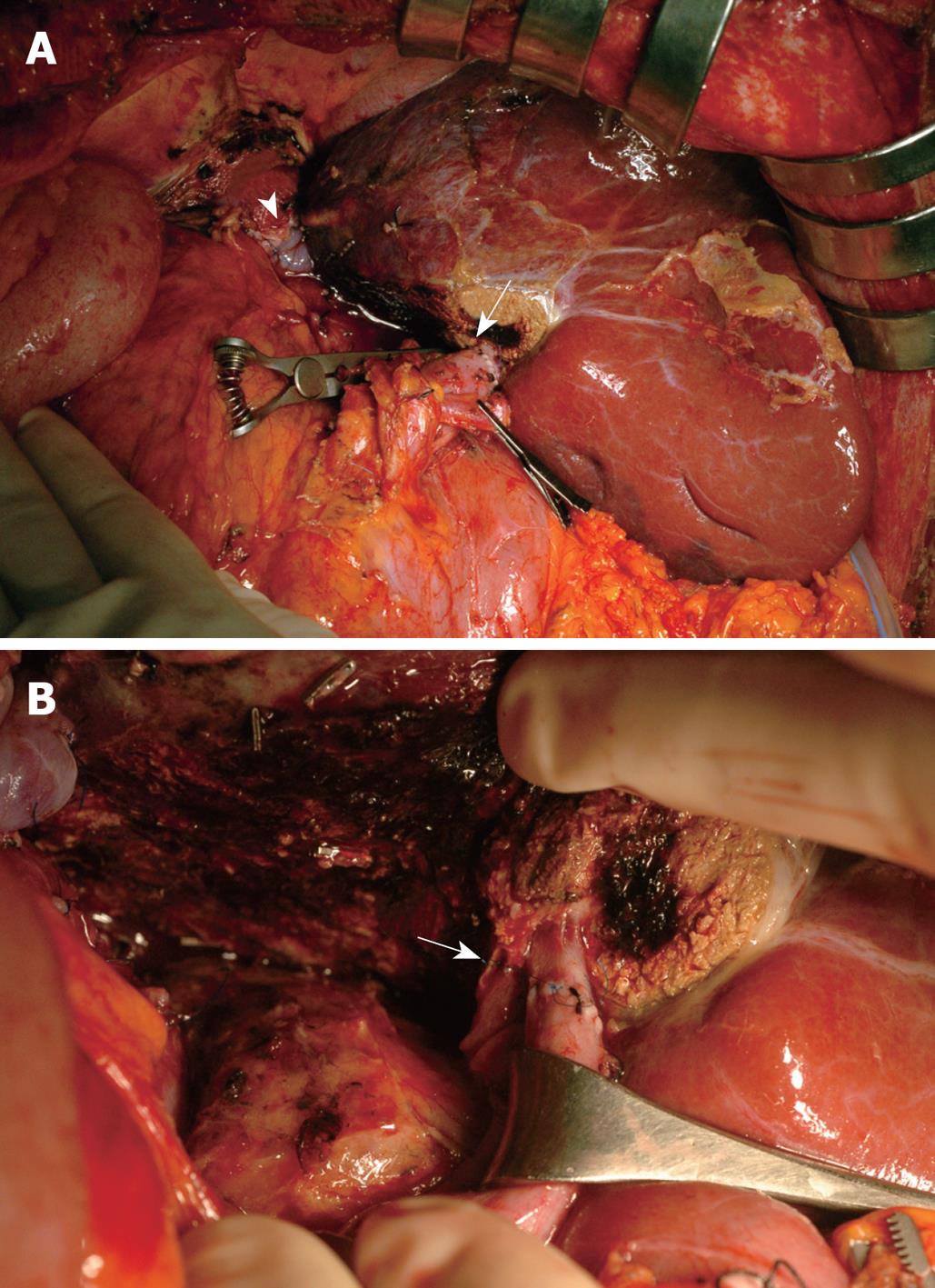
The donor operation was performed uneventfully according to the usual procedure of right posterior sectionectomy including right hepatic vein (RHV). There was no significant inferior right hepatic vein in the graft. The actual graft weight was 470 g. On the back table, protruded liver tissue behind the right posterior portal vein and RHV was cut out with an ultrasonic dissector to expose the portal and hepatic veins in reversed graft position. Under laparotomy of the recipient with inverted T-incision, complete rotation of all internal organs along the midline was observed without any vascular anomaly. Recipient hepatectomy was not complicated. The anhepatic time was 45 min. The reversed right posterior section graft was located in the recipient’s left subphrenic space. To gain sufficient graft outflow, a piece of cryopreserved vein patch was applied on the ventral portion of the graft’s RHV and a modified piggyback anastomosis was done. Vascular anastomoses of the portal vein and hepatic artery were performed as usual. The cold ischemic time was 2 h and the warm ischemic time was 45 min. In the reversed position of the right posterior section graft, the bile duct was located behind the portal vein. Thus, temporary downward traction of the portal vein was necessary for biliary anastomosis (Figure 1). Biliary anastomosis between the recipient’s common hepatic duct and the graft’s duct was performed successfully with 7-0 prolene continuous suture. Splenectomy was performed according to our indication of thrombocytopenia and splenomegaly. Total operation time was 11 h and 35 min.
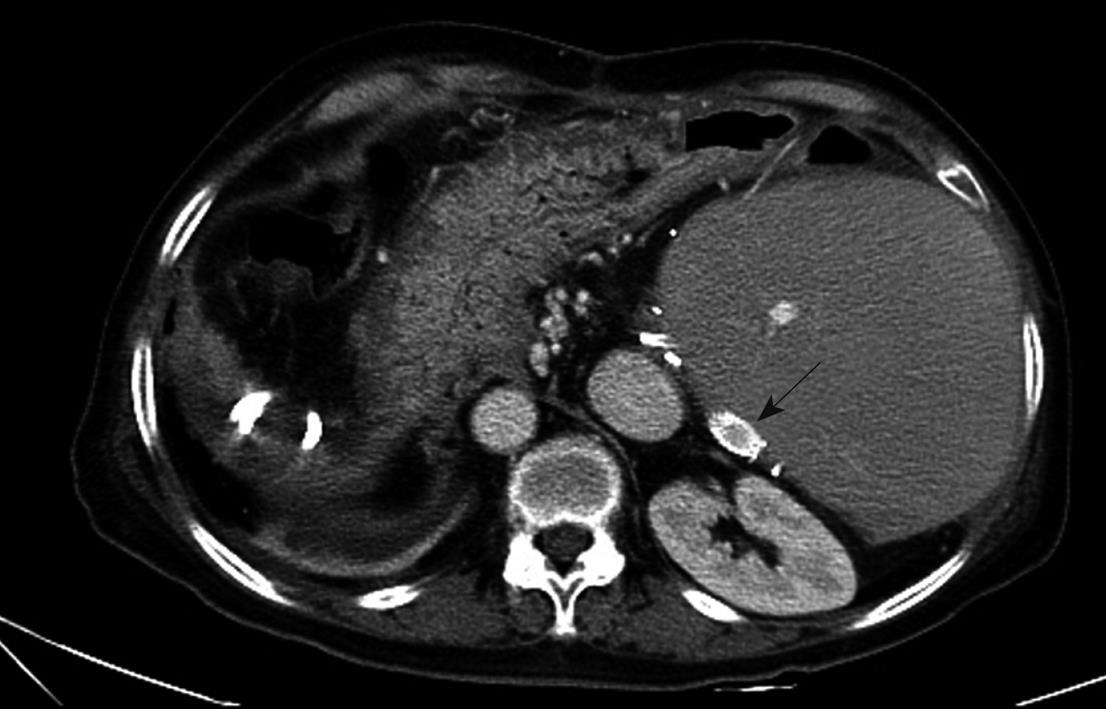
The patient’s postoperative course was excellent for 3 wk after transplantation, but the serum levels of liver enzymes subsequently started to elevate. However, there was no evidence of acute rejection on needle biopsy. Abdominal CT scan and hepatic Doppler ultrasound showed disturbance of blood flow in segment 6 RHV (V6 RHV) due to compression by the graft itself. A long endovascular stent was inserted into V6 RHV and the liver recovered quickly (Figure 2). Consequently, the patient was discharged at postoperative day 45 with good liver function. She has maintained good general condition and liver function for 8 mo postoperatively, up to the present time.
The major technical problem of liver transplantation for adult SIT is the spatial mismatch between the graft’s and recipient’s left upper quadrant space. Liver transplantation for the SIT patient has been performed at several centers, mainly using techniques of midline positioning or left shifting with/without clockwise rotation of the graft. However, these techniques have possible complications, such as graft displacement due to unfavorable position and vena cava compression by large right lobe of the graft.
Recently, Rayhill et al[7] reported a novel technique of 180-degree flip-over (facing backward) implantation of the whole liver graft into the recipient’s left subphrenic space. They reported excellent outcome without complication. Their technique provided not only orthotopic implantation of the whole graft but also good arrangement of portal vein, hepatic artery, and bile duct. We agree that orthotopic reversed graft implantation could overcome the possible complications of midline graft positioning for the SIT recipient.
Regarding LDLT, Chun et al[8] reported orthotopic implantation of a right lobe graft with 180-degree flip-over method from a living SIT donor to a recipient with normal anatomy. This technique is similar to ours in reversing the graft, but when using a reversed right lobe graft, the hilar plate is located more ventrally due to voluminous anterior sector behind the hilum. This could result in shortage of portal vein and bile duct, which leads to unavoidable tension in the anastomoses, and consequent vascular stretching or kinking. To avoid such complications, Chun et al used a special technique to achieve sufficient length of recipient’s portal vein and bile duct.
In our case, the location of the hilar plate of the right posterior sector was almost at the same level within the SIT recipient’s hepatic fossa in the reversed position. This allowed us to perform easy vascular and duct-to-duct biliary anastomoses without any of the complications mentioned above. To our knowledge, this is the first report of liver transplantation using a right posterior section graft for the adult patient with SIT. According to our experience, the only disadvantage of this technique using right posterior section graft is the possible compression of the V6 RHV, located at the bottom, by the graft itself during rapid liver regeneration after LDLT. The compression of the bottom-located RHV in reverse positioning of the right posterior section graft would be a common phenomenon, because there is little space to expand behind the RHV during rapid liver regeneration. Thus, we suggest that the surgeon should be alert to detect compression of the RHV during the early postoperative period. However, this complication could easily treated by inserting an endovascular stent.
In conclusion, reversed implantation of the right posterior section graft is one good option for liver transplantation in the adult recipient with SIT. This procedure provides not only orthotopic transplantation to the SIT recipient but also convenient vascular and duct-to-duct biliary anastomoses. In using this technique, however, we have to be alert during the postoperative course because the bottom-located RHV could be compressed by the graft.
Peer reviewers: Salvatore Gruttadauria, MD, Assistant Professor, Abdominal Transplant Surgery, ISMETT, Via E. Tricomi, 190127 Palermo, Italy; Julio Mayol, MD, PhD, Department of Digestive Surgery, Hospital Clinico San Carlos, MARTIN-LAGOS S/n, Madrid, 28040, Spain
S- Editor Tian L L- Editor Logan S E- Editor Lin YP
| 1. | Raynor SC, Wood RP, Spanta AD, Shaw BW Jr. Liver transplantation in a patient with abdominal situs inversus. Transplantation. 1988;45:661-663. |
| 2. | Tucker O, Prachalias A, Kane P, Rela M. Graft positioning at liver transplantation in situs inversus. Liver Transpl. 2006;12:1720-1722. |
| 3. | Klintmalm GB, Bell MS, Husberg BS, Holman MJ, Goldstein RM, Ramsay MA, Polter DE. Liver transplant in complete situs inversus: a case report. Surgery. 1993;114:102-106. |
| 4. | Soejima Y, Meguro M, Taketomi A, Ikegami T, Yamashita Y, Harada N, Ito S, Uchiyama H, Yoshizumi T, Maehara Y. Left lobe living donor liver transplantation in an adult patient with situs inversus: technical considerations. Transpl Int. 2008;21:384-389. |
| 5. | Heimbach JK, Menon KV, Ishitani MB, Nyberg SL, Jankowski CJ, Lindor KD, Rosen CB. Living donor liver transplantation using a right lobe graft in an adult with situs inversus. Liver Transpl. 2005;11:111-113. |
| 6. | Sugawara Y, Makuuchi M, Takayama T, Imamura H, Kaneko J. Right lateral sector graft in adult living-related liver transplantation. Transplantation. 2002;73:111-114. |
| 7. | Rayhill SC, Scott D, Orloff S, Horn JL, Schwartz J, Zaman A, Sasaki A, Naugler WS, Chang M, Gaumond J. Orthotopic, but reversed implantation of the liver allograft in situs inversus totalis-a simple new approach to a difficult problem. Am J Transplant. 2009;9:1602-1606. |
| 8. | Chun JM, Jung GO, Choi GS, Park JB, Kwon CH, Kim SJ, Joh JW, Lee SK. Living donor liver transplantation using a graft from a donor with situs inversus totalis. Liver Transpl. 2009;15:666-669. |