Published online Apr 28, 2010. doi: 10.3748/wjg.v16.i16.2017
Revised: February 4, 2010
Accepted: February 11, 2010
Published online: April 28, 2010
AIM: To assess the risk factors and the efficacy of medications of patients with gastric and duodenal ulcers among Chinese patients in Taiwan.
METHODS: Patients with peptic ulcers, diagnosed by upper endoscopy, were retrospectively collected between January 2008 and December 2008. The differences were compared.
RESULTS: Among all 448 cases, 254 (56.6%) and 194 (43.4%) patients had gastric ulcers and duodenal ulcers respectively. Patients with gastric ulcers were younger than those with duodenal ulcers. Although more men existed, there was a female predominance in middle-aged cases. Patients with duodenal ulcers had a higher rate of Helicobacter pylori (H. pylori) infection (62.4% vs 43.3%, P = 0.001), and those with gastric ulcers owned a significantly higher amount of aspirin and nonsteroidal anti-inflammatory drug (NSAID) use (7.5% vs 1.5%, 6.7% vs 2.1%, P = 0.001). Tobacco smoking and alcohol drinking had no different impact between these two groups. Proton-pump inhibitors and H2-receptor antagonists (H2RA) were effective, but significantly less so in cases with duodenal ulcers receiving H2RAs, or in those with H. pylori infection and a history of NSAID use.
CONCLUSION: Patients with gastric ulcers had lower H. pylori infection but more aspirin or NSAID use. Antisecretory therapy was ineffective in gastric ulcers underwent H2RA treatment, and cases combined H. pylori infection and NSAID use.
- Citation: Lee SW, Chang CS, Lee TY, Yeh HZ, Tung CF, Peng YC. Risk factors and therapeutic response in Chinese patients with peptic ulcer disease. World J Gastroenterol 2010; 16(16): 2017-2022
- URL: https://www.wjgnet.com/1007-9327/full/v16/i16/2017.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i16.2017
Peptic ulcer disease develops when the protective mechanisms of the gastrointestinal mucosa, such as mucus and bicarbonate secretion, are overwhelmed by the damaging effects of gastric acid and pepsin[1]. Peptic ulcers occur mainly in the stomach (gastric ulcer) or proximal duodenum (duodenal ulcer), and they continue to be a common disease that causes a substantial socioeconomic burden and negatively impacts on quality of life.
Helicobacter pylori (H. pylori) infection was originally identified as the main cause of peptic ulcers. As the prevalence of H. pylori infection has declined in western countries, gastric ulcer has become more commonly associated with the use of nonsteroidal anti-inflammatory drugs (NSAID) and aspirin[2]. Tobacco smoking and alcohol drinking were also meaningful risk factors for peptic ulcer disease[3].
Effective pharmacologic suppression of gastric acid secretion began with the introduction of H2-receptor antagonists (H2RA) in the 1970s, which greatly improved clinical outcomes. The development of proton-pump inhibitors (PPI) further improved inhibition of gastric acid secretion, and ensured very high healing rates for duodenal and gastric ulcers[4]. The aim of this study was to compare the association of H. pylori infection, NSAID and aspirin use, tobacco smoking and alcohol drinking with gastric and duodenal ulcers, and further assess the efficacy of therapeutic medications in the patients with peptic ulcer disease.
Data from the medical records of consecutive patients with peptic ulcers, diagnosed by open-access transoral upper endoscopy in our hospital, a 1155-bed academic urban tertiary-care center, were retrospectively analyzed between January 2008 and December 2008. Exclusion criteria were as follows: (1) cirrhosis with varices or portal hypertensive gastropathy, (2) combined other structural gastrointestinal disorders, such as gastroesophageal reflux disease, esophageal or gastric malignancy, (3) prior gastric surgery, (4) use of chronic anti-acid medication, such as PPI or H2RA, for more than 2 mo prior to enrollment, and (5) combined gastroduodenal ulcers so undistinguished clearly.
Written informed consent for upper endoscopy was obtained from all patients before the procedure. Medications taken longer than 3 mo prior to the enrollment, including aspirin or other NSAID, were recorded. Aspirin and NSAID were recorded separately due to discrepant doses of these drugs. All cases underwent rapid urease test (CLO test, Delta West, Bentley, Australia) for H. pylori status from antral biopsy.
Patients were assigned to the gastric ulcer group or the duodenal ulcer group according to the locations of peptic ulcers, which were confirmed by experienced gastroenterologists. The definition of peptic ulcers was mucosal break of stomach or duodenum over 3 mm in diameter, or more than 10 gastric or duodenal erosions. The patients with H. pylori infection underwent standard eradication therapy, including oral PPI 40 mg, amoxicillin 2 g and Klaricid 1 g a day for one week. All patients enrolled in the study received PPI (omeprazole 20 mg, lansoprazole 30 mg, pantoprazole 40 mg once per day) or H2RA (ranitidine 150 mg, cimetidine 400 mg twice a day). The efficacy of therapeutic medications was defined as ulcer healing and negative rapid urease test evaluated by repeated endoscopy pulse antral biopsy at our outpatient clinic 3 mo following initial endoscopy. Patients who received aspirin were also given PPI or H2RA, and those who received NSAID were shifted to Coxibs in addition to standard PPI or H2RA use.
Data are expressed as standard derivation of mean for each of the measured parameters. Gender, H. pylori infection, and combined medication are expressed as a percentage of the total patient number. Statistical comparisons were made using Pearson’s χ2 test to compare the effects of gender, H. pylori infection, tobacco smoking, alcohol drinking, combined medications, and risk factors. t test was used to compare the mean ages of patients, and Fisher’s exact test was applied to evaluate the therapeutic efficacy of cases with aspirin or NSAID use. A P value below 0.05 was considered statistically significant.
Among all consecutive patients who received open-access upper endoscopy between January and December 2008, there were 448 cases enrolled in our study and the characteristic of them were displayed in Table 1. Among these patients, 254 patients (56.6%) had isolated gastric ulcers and 194 patients (43.4%) had isolated duodenal ulcers. Comparing the chronic medication use of patients with gastric ulcers and duodenal ulcers, more patients with gastric ulcers took aspirin and NSAID than did those with duodenal ulcers (7.5% vs 1.5%, 6.7% vs 2.1%, respectively), and the difference was significant (P = 0.001).
| Upper endoscopy finding | Total | P-value | ||
| Gastric ulcers | Duodenal ulcers | |||
| Case numbers (prevalence) | 254 (56.6) | 194 (43.4) | 448 (100) | |
| Age (yr) | 60.44 ± 15.27 | 51.99 ± 16.24 | 0.0011 | |
| Gender | ||||
| Male | 142 (55.8) | 110 (56.7) | 252 (56.2) | 0.8662 |
| Female | 112 (44.1) | 84 (43.3) | 196 (43.8) | |
| H. pylori | ||||
| Positive | 110 (43.3) | 121 (62.4) | 231 (56.7) | 0.0012 |
| Negative | 144 (56.7) | 73 (37.6) | 217 (43.3) | |
| Smoking | ||||
| Yes | 36 (14.2) | 31 (16.0) | 67 (15.8) | 0.5952 |
| No | 218 (85.8) | 163 (84.0) | 381 (86.0) | |
| Alcohol | ||||
| Yes | 21 (8.3) | 22 (11.3) | 43 (9.6) | 0.2742 |
| No | 233 (91.7) | 172 (88.7) | 405 (90.4) | |
| Co-medications | ||||
| Nil | 218 (85.8) | 187 (96.4) | 405 (90.4) | 0.0012 |
| Aspirin | 19 (7.5) | 3 (1.5) | 22 (4.9) | |
| NSAIDs | 17 (6.7) | 4 (2.1) | 21 (4.7) | |
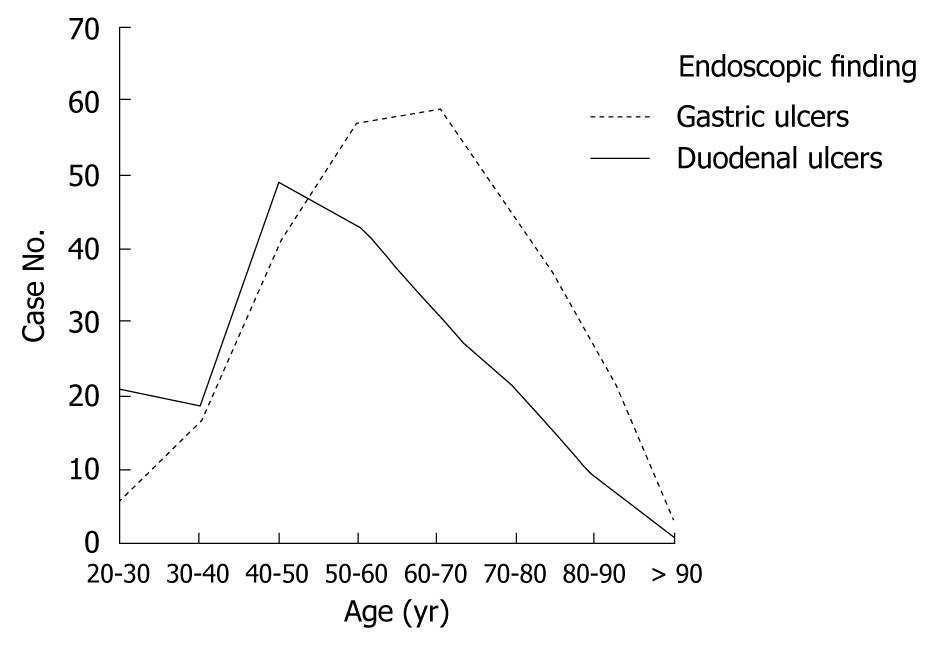
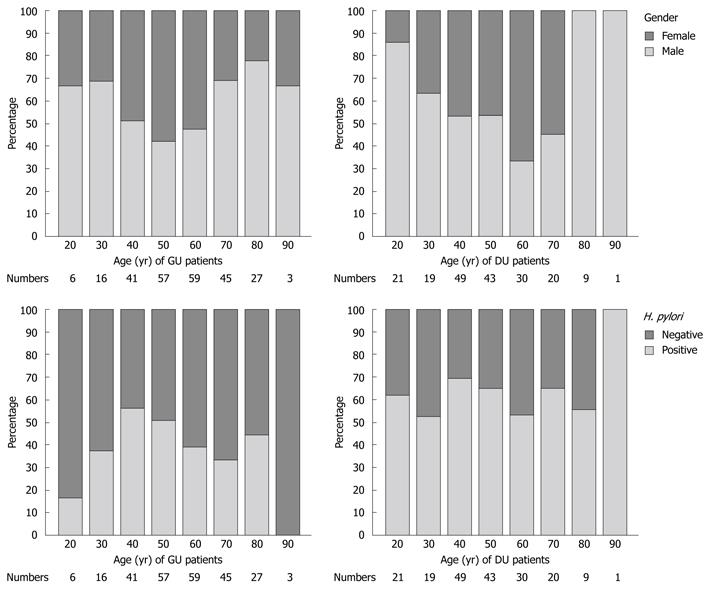
Most of the patients with gastric ulcers were in the fifth decade of life, whereas most patients with duodenal ulcers were in the sixth decade, as shown in Figure 1. There were more male patients than female patients in both groups, and a similar gender ratio existed between these two groups. The ratio of gender according to age distribution is shown in Figure 2. More female cases were noted in the 50-60-year-old patients with gastric ulcers and the 60-70-year-old patients with duodenal ulcers. Male predominance was noted in both the younger and older gastric ulcer and duodenal ulcer patients.
The rate of H. pylori infection, shown in Table 1, was significantly higher in the patients with duodenal ulcers than in those with gastric ulcers (62.4% vs 43.3%, P = 0.001). Similarly, more patients with duodenal ulcers smoked tobacco and drank alcohol than those with gastric ulcers (16% vs 14.2%, 11.3% vs 8.3%, respectively), but these differences in our study were insignificant (P = 0.595 and 0.274).
There was a similar proportion of patients in each of the two groups with positive H. pylori infection according to age distribution, as shown in Figure 2. The lowest rate was noted in gastric ulcer patients in the second and ninth decades of life, and the highest rate was found in duodenal ulcer patients in the ninth decade of life. However, the numbers in these groups were very small.
In regard to the impact of therapeutic efficacy on H. pylori infection, all had effective eradication proven by negative secondary rapid urease test. As illustrated in Table 2, the results revealed there were similar rates of peptic ulcer healing among patients with and without H. pylori infection in both groups who underwent eradication therapy. There was no significant difference between the efficacy of PPI and H2RA among patients with duodenal ulcers (78.2% vs 72.3%, P = 0.430). On the contrary, PPI was significantly more effective than H2RA in patients with gastric ulcers (79.4% vs 62.9%, P = 0.007).
| Therapeutic efficacy | Total | P-value | ||
| Ulcer healed | Ulcer unhealed | |||
| H. pylori | ||||
| GU | ||||
| Positive infections | 77 (70.6) | 32 (29.4) | 109 | 0.661 |
| Negative infections | 99 (68.3) | 46 (31.7) | 145 | |
| DU | ||||
| Positive infections | 87 (71.9) | 34 (28.1) | 121 | 0.505 |
| Negative infections | 55 (75.3) | 18 (24.7) | 73 | |
| Medications | ||||
| GU | ||||
| Treat with PPI | 131 (79.4) | 34 (20.6) | 165 | 0.007 |
| Treat with H2RA | 56 (62.9) | 33 (37.1) | 89 | |
| DU | ||||
| Treat with PPI | 115 (78.2) | 32 (21.8) | 147 | 0.430 |
| Treat with H2RA | 34 (72.3) | 13 (27.7) | 47 | |
As shown in Table 3, the therapeutic efficacy of PPI and H2RA was compared among patients who used aspirin or NSAIDs regularly or took no medicine. In regard to the combined influence of H. pylori infection and chronic aspirin or NSAID use in patients with peptic ulcer disease, there was a lower rate of response to therapeutic medicine, especially in the cases taking NSAID (60% vs 100%, P = 0.035).
| Co-medications | Therapeutic efficacy | Total | P-value | |
| Ulcer healed | Ulcer unhealed | |||
| None | ||||
| Positive H. pylori infection | 159 (75.7) | 51 (24.3) | 210 | 0.370a |
| Negative H. pylori infection | 140 (71.8) | 55 (28.2) | 195 | |
| ASP | ||||
| Positive H. pylori infection | 8 (80) | 2 (20) | 10 | 0.195b |
| Negative H. pylori infection | 12 (100) | 0 | 12 | |
| NSAID | ||||
| Positive H. pylori infection | 6 (60) | 4 (40) | 10 | 0.035b |
| Negative H. pylori infection | 11 (100) | 0 | 11 | |
Peptic ulcer disease is associated with gastric hypersecretion, a physiological imbalance between antagonistic gastric hormones, cholinergic hypersensitivity, psychological stress, tobacco smoking, alcohol consumption, or use of aspirin and NSAID. Duodenal ulcer is essentially an H. pylori-related disease and is caused mainly by an increase in acid and pepsin load[5]. Gastric ulcer in Western countries is most commonly associated with NSAID ingestion or H. pylori infection. As the prevalence of H. pylori infection has declined in western countries, gastric ulcer has become more commonly associated with the use of NSAID and aspirin[6].
The prevalence of peptic ulcers in developed countries has been declining for several decades owing to improvements in sanitation and a reduced rate of H. pylori acquisition[7]. Recently, a study in Taiwan reported incidences of gastric and duodenal ulcer diseases decreased 42%-48% and 41%-71%, respectively, in a 10-year period[8]. The birth cohorts with the highest risk of developing gastric ulcer were born 10-20 years before those with the highest risk for duodenal ulcer in all European countries, the USA, Australia and Japan[9]. Our results were similar, although our study was not population-based.
Previous studies have shown that male gender is an independent risk factor for peptic ulcer disease in populations in the USA, Japan and Norway[10-12]. Our results documented male predominance in both the patients with gastric ulcers and in those with duodenal ulcers. Interestingly, we also found there was relative female predominance in middle-aged patients, although no previous studies had similar findings. The reason may be that middle-aged women are more likely to seek medical treatment than men in the same age group.
Previous studies had documented tobacco smoking and alcohol drinking as firm risk factors for peptic ulcer disease[3,5], however, no available data focused on the different impacts of these factors in achieving gastric ulcers and duodenal ulcers. Our study found similar influences of these two groups, implying the excellent benefit of quitting tobacco smoking and alcohol drinking in patients with peptic ulcer disease, regardless of the location of the ulcers.
During the 1980s, H. pylori infection was found in more than 90% of patients with duodenal ulcers, and around 70% of patients with gastric ulcers[13]. An increased prevalence correlates with lower educational levels, income, and other socioeconomic factors[14]. A recent study reported a seroprevalence of H. pylori infection in 56.4% of patients with duodenal ulcers and a lower rate in those with gastric ulcers[3]. Similarly, our patients had a lower prevalence of H. pylori infection than previously expected, with a rate of 42.9% in cases with gastric ulcers, and 62.4% in those with duodenal ulcers. The result may be due to improvements in hygiene, and it emphasizes the fact that eradication therapy should not be initiated without prior verification of the infection.
On the contrary, aspirin and NSAID significantly increase the risk of adverse gastric or duodenal ulcers and complications, especially bleeding[3]. Gastric ulcers are strongly linked to NSAIDs, and this was confirmed by the positive relationship between aspirin or NSAID use and gastric ulcers in our study. H. pylori infection and NSAID have additive or synergistic effects on adverse gastrointestinal outcomes: H. pylori damages through direct pathogenic mechanisms, and NSAID causes disruption of mucosal defensive mechanisms indirectly[2]. Our study did not include this conclusion because there were too few cases with H. pylori infection taking aspirin or NSAID to be analyzed sufficiently.
In regard to the patients with peptic ulcer disease owing to H. pylori infection, studies indicate that eradication of infection not only heals peptic ulcers, but also reduces the ulcer recurrence rate[15]. Maintenance treatment should be continued with PPI use following H. pylori eradication in all patients to prevent ulcer recurrence or complications[16]. Standard dose PPI treatment should be prescribed for 4 wk in patients with duodenal ulcers and for 8 wk in patients with gastric ulcers[17].
The results of our study revealed an adequate ulcer healing rate in patients with gastric or duodenal ulcers who received antisecretory therapy, PPI or H2RA, whether they had H. pylori infection or not, and whether they were taking aspirin and other NSAID or not. There were two subgroups of patients with a significantly poor therapeutic response: patients with gastric ulcers who underwent H2RA treatment (62.9%), and patients with both H. pylori infection and NSAID use who accepted antisecretory therapy (60%).
One previous study noted that pantoprazole was more effective than ranitidine in the treatment of duodenal ulcers, providing not only symptom remission but also faster ulcer healing[18]. Another study reported H. pylori infection and NSAID use synergistically increase the risk of peptic ulcers and ulcer bleeding[19]. These results implied that PPI, at least in duodenal ulcers, is more effective than H2RA, and prolonged antisecretory therapy may be necessary in the treatment of peptic ulcers caused by H. pylori infection and NSAID use. One recent study among a Japanese population also mentioned that it is desirable to administer antiulcer agents to patients with risk factors, such as H. pylori infection, when taking NSAID[20].
There were some limitations in our study. Firstly, our study, a form of referral-based endoscopy, as opposed to a population-based survey, was less representative of the general population due to selection bias. Secondly, we only recorded the recent use of NSAID. There is a possibility that some patients were unaware that they were taking NSAIDs. Besides, the kinds of NSAID and PPI were heterogeneous. Thirdly, only an incomplete previous history of peptic ulcer disease or H. pylori infection was available to be analyzed. Furthermore, previous H. pylori eradication was not listed in the exclusion criteria of this study, and the H. pylori infection rate may be an underestimation. Lastly, major limitations of this study included the retrospective study design and the lack of randomization. Although the duration of this study was designed to be as long as one year, it is possible that there were unmeasured differences among these subgroups.
In the present study, Chinese patients in Taiwan with peptic ulcers had different characteristics. The patients with gastric ulcers were older, had a lower ratio of H. pylori infection and a greater association with aspirin or NSAID use, compared with those with duodenal ulcers. Antisecretory therapy was very effective in patients with peptic ulcer disease, except cases with gastric ulcers who underwent H2RA treatment, and those who had combined H. pylori infection and NSAID use and accepted antisecretory therapy.
Peptic ulcer disease is associated with Helicobacter pylori (H. pylori) infection, aspirin and nonsteroidal anti-inflammatory drug (NSAID) use, tobacco smoking and alcohol drinking. Effective pharmacological therapy includes H2-receptor antagonist (H2RA) and proton-pump inhibitor (PPI).
Although risk factors and therapeutic efficacy are well known in Western countries, the information in the Chinese population is relatively rare. The aim of this study was to assess the risk factors and the efficacy of medications of patients with gastric and duodenal ulcers among Chinese patients in Taiwan.
The authors’ result found that Chinese patients in Taiwan with gastric ulcers were older, had a lower ratio of H. pylori infection and a greater association with aspirin or NSAID use compared with those with duodenal ulcers. Antisecretory therapy was very effective against peptic ulcers, except in cases with gastric ulcers who underwent H2RA treatment, and those with combined H. pylori infection and NSAID use who accepted antisecretory therapy.
Maintenance treatment should be continued with PPI use, following H. pylori eradication, in all patients to prevent ulcer recurrence or complications, especially in cases who used NSAID.
The study compares a group of gastric ulcer patients with a group of duodenal ulcer patients in terms of demographic characteristics, certain risk factors, and response to treatment. It is of moderate importance with minimal novelty.
Peer reviewers: Reza Malekzadeh, Professor, Director, Digestive Disease Research Center, Tehran University of Medical Sciences, Shariati Hospital, Kargar Shomali Avenue, 19119 Tehran, Iran; Julio H Carri, Professor, Internal Medicine - Gastroenterology, National University of Córdoba, Av. Estrada 160-P 5-Department D, Córdoba 5000, Argentina
S- Editor Wang YR L- Editor O'Neill M E- Editor Lin YP
| 1. | Sung JJ, Kuipers EJ, El-Serag HB. Systematic review: the global incidence and prevalence of peptic ulcer disease. Aliment Pharmacol Ther. 2009;29:938-946. |
| 2. | Makola D, Peura DA, Crowe SE. Helicobacter pylori infection and related gastrointestinal diseases. J Clin Gastroenterol. 2007;41:548-558. |
| 3. | Rosenstock S, Jørgensen T, Bonnevie O, Andersen L. Risk factors for peptic ulcer disease: a population based prospective cohort study comprising 2416 Danish adults. Gut. 2003;52:186-193. |
| 4. | Yuan Y, Padol IT, Hunt RH. Peptic ulcer disease today. Nat Clin Pract Gastroenterol Hepatol. 2006;3:80-89. |
| 5. | Dore MP, Graham DY. Pathogenesis of duodenal ulcer disease: the rest of the story. Baillieres Best Pract Res Clin Gastroenterol. 2000;14:97-107. |
| 6. | Laine L. Nonsteroidal anti-inflammatory drug gastropathy. Gastrointest Endosc Clin N Am. 1996;6:489-504. |
| 7. | Pérez-Aisa MA, Del Pino D, Siles M, Lanas A. Clinical trends in ulcer diagnosis in a population with high prevalence of Helicobacter pylori infection. Aliment Pharmacol Ther. 2005;21:65-72. |
| 8. | Wu CY, Wu CH, Wu MS, Wang CB, Cheng JS, Kuo KN, Lin JT. A nationwide population-based cohort study shows reduced hospitalization for peptic ulcer disease associated with H pylori eradication and proton pump inhibitor use. Clin Gastroenterol Hepatol. 2009;7:427-431. |
| 9. | Sonnenberg A. Temporal trends and geographical variations of peptic ulcer disease. Aliment Pharmacol Ther. 1995;9 Suppl 2:3-12. |
| 10. | Harewood GC, Holub JL, Lieberman DA. Biopsy specimen acquisition in patients with newly diagnosed peptic ulcer disease as determined from a national endoscopic database. Gastrointest Endosc. 2004;59:664-669. |
| 11. | Watanabe Y, Kurata JH, Kawamoto K, Kawai K. Epidemiological study of peptic ulcer disease among Japanese and Koreans in Japan. J Clin Gastroenterol. 1992;15:68-74. |
| 12. | Bernersen B, Johnsen R, Straume B, Burhol PG, Jenssen TG, Stakkevold PA. Towards a true prevalence of peptic ulcer: the Sørreisa gastrointestinal disorder study. Gut. 1990;31:989-992. |
| 13. | Graham DY, Klein PD, Opekun AR, Boutton TW. Effect of age on the frequency of active Campylobacter pylori infection diagnosed by the [13C]urea breath test in normal subjects and patients with peptic ulcer disease. J Infect Dis. 1988;157:777-780. |
| 14. | Suerbaum S, Michetti P. Helicobacter pylori infection. N Engl J Med. 2002;347:1175-1186. |
| 15. | Arkkila PE, Seppälä K, Kosunen TU, Sipponen P, Mäkinen J, Rautelin H, Färkkilä M. Helicobacter pylori eradication as the sole treatment for gastric and duodenal ulcers. Eur J Gastroenterol Hepatol. 2005;17:93-101. |
| 16. | Lai KC, Lam SK, Chu KM, Wong BC, Hui WM, Hu WH, Lau GK, Wong WM, Yuen MF, Chan AO. Lansoprazole for the prevention of recurrences of ulcer complications from long-term low-dose aspirin use. N Engl J Med. 2002;346:2033-2038. |
| 17. | Yeomans ND. New data on healing of nonsteroidal anti-inflammatory drug-associated ulcers and erosions. Omeprazole NSAID Steering Committee. Am J Med. 1998;104:56S-61S; discussion 79S-80S. |
| 18. | Meneghelli UG, Zaterka S, de Paula Castro L, Malafaia O, Lyra LG. Pantoprazole versus ranitidine in the treatment of duodenal ulcer: a multicenter study in Brazil. Am J Gastroenterol. 2000;95:62-66. |
| 19. | Huang JQ, Sridhar S, Hunt RH. Role of Helicobacter pylori infection and non-steroidal anti-inflammatory drugs in peptic-ulcer disease: a meta-analysis. Lancet. 2002;359:14-22. |
| 20. | Murakami K, Okimoto T, Kodama M, Tanahashi J, Yasaka S, Inoue K, Uchida M, Anan J, Mizukami K, Abe T. Helicobacter pylori and NSAID-induced gastric ulcer in a Japanese population. J Gastroenterol. 2009;44 Suppl 19:40-43. |