Published online Mar 28, 2010. doi: 10.3748/wjg.v16.i12.1541
Revised: January 12, 2010
Accepted: January 19, 2010
Published online: March 28, 2010
Endoscopic therapy of pancreatic duct (PD) strictures using balloon dilation and pancreatic duct stent (PS) placement has been reported to improve the severity of abdominal pain in selected patients with chronic pancreatitis (CP). However, some strictures are refractory and require frequent PS exchange to control symptoms. We describe two cases of successful endoscopic PD incision for difficult PD stricture using a wire-guided snare. The snare is partially opened within the strictured pancreatic duct while applying current, thus incising the duct. Although both cases were successful without complications we do not advocate that this method be used routinely because of the potential for severe complications, e.g. bleeding, ductal perforation or pancreatic parenchymal damage. In order to prevent these complications, we developed a wire-guided technique under fluoroscopic control. We think this procedure may be useful in patients with short, straight PD strictures. Although further study is required, this approach may have potential for selected patients with refractory PD strictures due to CP.
- Citation: Itoi T, Sofuni A, Itokawa F, Kurihara T, Tsuchiya T, Ishii K, Tsuji S, Ikeuchi N, Moriyasu F. Transpapillary incision of refractory circumscript pancreatic duct stricture using wire-guided snare forceps. World J Gastroenterol 2010; 16(12): 1541-1544
- URL: https://www.wjgnet.com/1007-9327/full/v16/i12/1541.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i12.1541
Endoscopic therapy of pancreatic duct (PD) strictures using balloon dilation and pancreatic duct stent placement has been reported to improve the severity of abdominal pain in selected patients with chronic pancreatitis (CP)[1-6]. However, some strictures are refractory and require frequent stent exchange to control symptoms. We describe two cases of successful endoscopic PD incisions for difficult PD strictures using a wire-guided snare. The snare is partially opened within the strictured pancreatic duct while applying electrical current, to incise the duct.
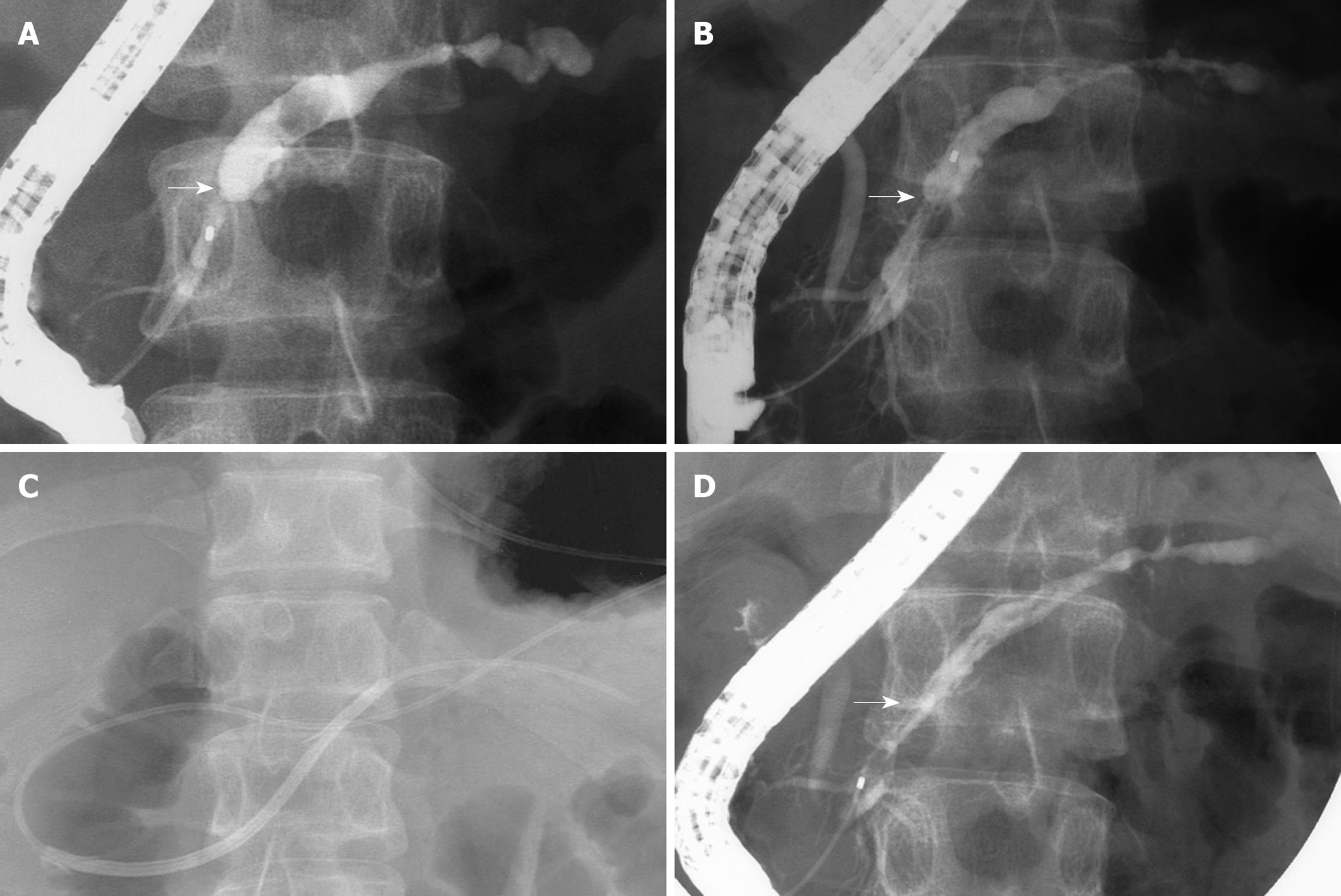
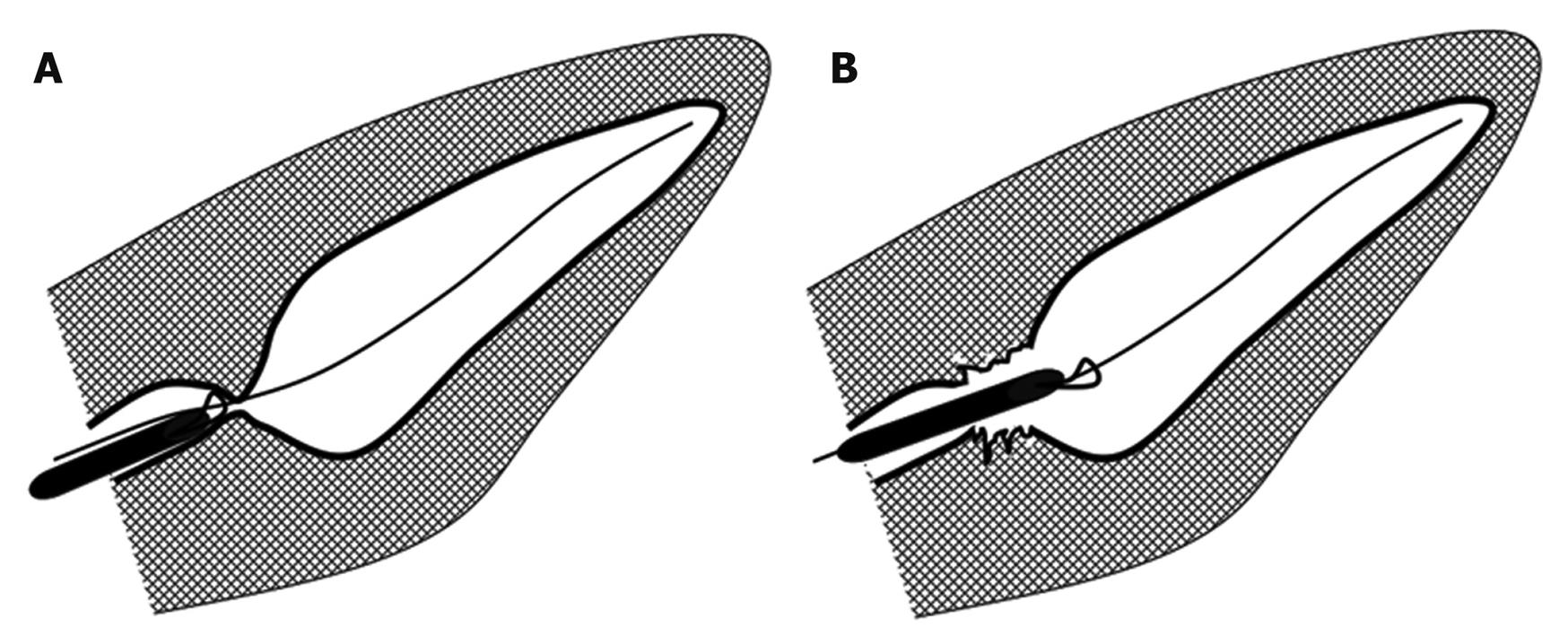
A 35-year-old man with a 2-year history of acute chronic pancreatitis required repeated initial placement of a 7-Fr stent, followed by 10-Fr pancreatic duct stent exchange after a major papillotomy for management of a tight, short PD stricture (Figure 1A). Pancreatography after removal of the 10-Fr stent still showed a PD stricture (Figure 1B); the PD stent removal had been performed 6 mo previously at the patient’s request. He was subsequently admitted with severe epigastric pain and recurrent pancreatitis. Pancreatography revealed obstruction of the PD and a 7-Fr stent was placed. We again recommended regular stent exchange or surgical therapy, but he refused. One month later, a transpapillary PD incision was performed in an attempt to produce stricture resolution without a stent. A guidewire was inserted across the stricture, and a standard snare (SD-5U-1, 6U-1, Olympus Medical Systems, Tokyo, Japan) was advanced over the wire to the level of the stricture (Figure 1C). A PD incision was performed using an electrosurgical generator (ICC200; ERBE Elektromedizin GmbH, Tubingen, Germany) (Figure 2A and B). The patient experienced pain during the incision. A 10-Fr stent was placed without any serious complications such as bleeding or pancreatitis. Two weeks later the stent was removed (Figure 1D). The patient remains asymptomatic 3 years later.
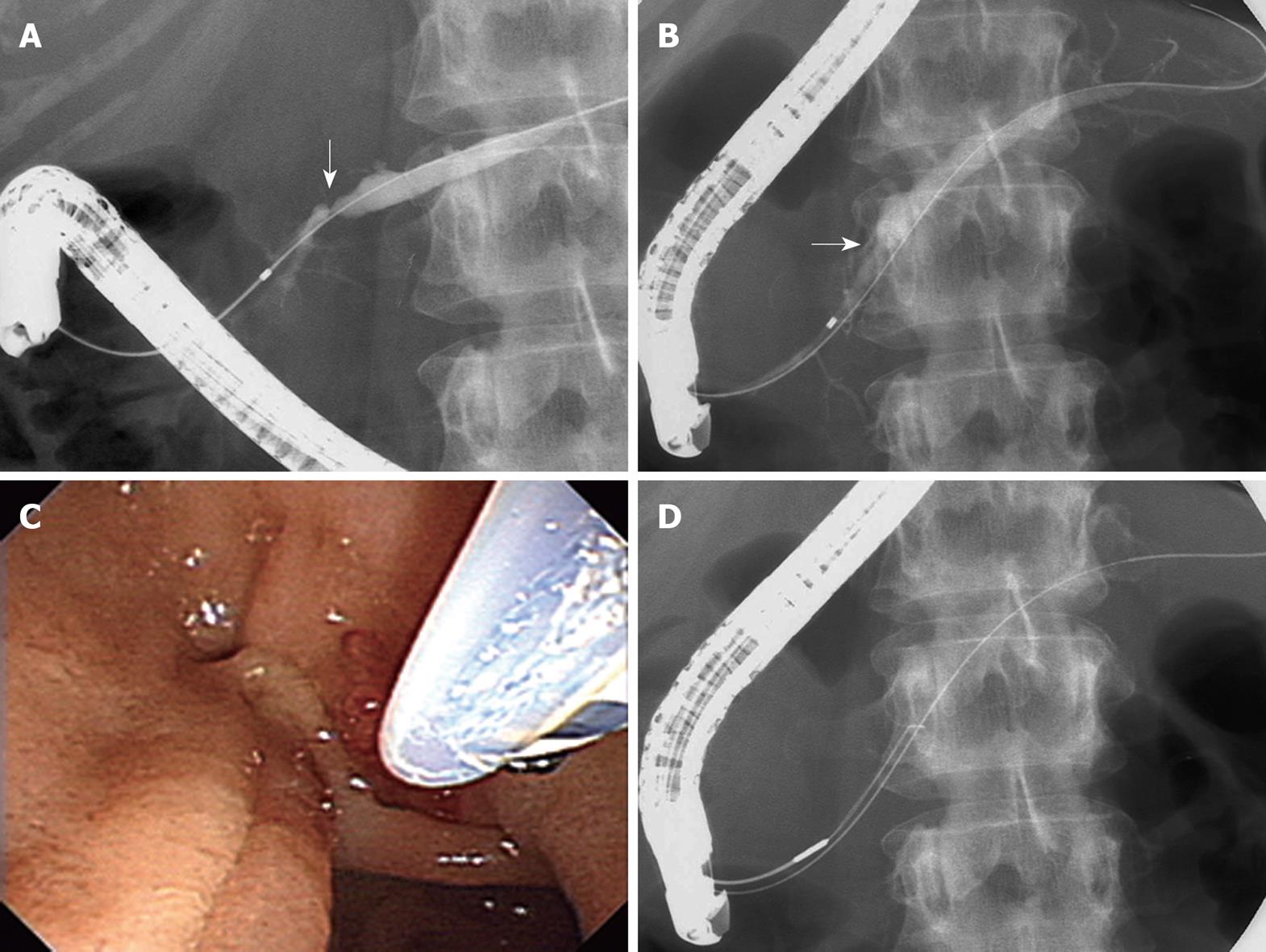
A 37-year-old woman had undergone regular replacement of 7-Fr and 10-Fr stents with a minor papillotomy across the minor papilla for management of a PD stricture (Figure 3A) due to pancreas divism for the past 3 years. Although pancreatography after removal of the 10-Fr stent still showed a PD stricture (Figure 3B), the stent was removed at the patient’s request. However, 8 mo later, she developed severe epigastric pain due to recurrent pancreatitis. Since she refused regular stent exchange and surgical therapy, a PD incision was performed as described in the previous case. A 10-Fr stent was placed (Figure 3C and D). No complications occurred. The stent was removed one month later. She remains asymptomatic 18 mo later.
Placement of a pancreatic duct stent can often result in symptomatic improvement in patients with PD strictures caused by CP. However, long-term outcomes are not necessarily satisfactory. In patients with refractory PD strictures, regular, single or multiple stent replacements may be required for sustained symptom improvement[4-6]. Such refractory strictures can be dilated using a Soehendra stent extractor[7] or by self-expandable metal stent placement[8]. Interestingly, Kawamoto et al[9] reported the dissection of a difficult PD stricture using a needle-knife. Although the aim of their technique was recanalization of the pancreatic duct showing disconnection using a needle, our aim was persistent canalization without any stent.
Until now, endoscopic therapy using stents has been a well-established procedure. Nevertheless, several investigators have advocated that the technique of regular stent replacement is not recommended for CP with circumscript PD stenosis because outcomes of a surgical approach in these cases were superior to those of an endoscopic approach[10-12].
In the present cases, the patients strongly refused surgical therapy. We therefore performed PD incision in anticipation that mechanical manipulation around the stricture might allow stricture resolution. We hypothesized that the snare could obtain a wider aperture compared to a sharp dissection using a needle knife. Although both cases were successful without complications we do not advocate that this method should be used routinely because of the potential for severe complications, e.g. bleeding, ductal perforation, or pancreatic parenchymal damage. In order to prevent these complications, we developed a wire-guided technique under fluoroscopic control. Furthermore, we advocate that the technique described here is rather experimental and should only be used in experienced hands due to the possibility of severe complications.
With regard to necessity and duration of a temporary stent placement after PD incision, this is a controversial issue because a relatively large PD incision can be expected. However, we used a stent to avoid acute obstructive pancreatitis due to edematous change for a period of 1 mo. We think this procedure may be useful in patients with circumscript, straight PD strictures.
Limitations of this study include a small sample size, lack of a control group and no long-term outcomes.
In conclusion, although we do not think that this procedure can replace conventional endoscopic therapy as the first-line treatment, this approach may have potential for selected patients with refractory circumscript PD strictures due to CP.
Peer reviewers: Yoshiaki Murakami, MD, Department of Surgery, Division of Clinical Medical Science, Graduate School of Biomedical Science, Hiroshima University, 1-2-3 Kasumi, Minami-ku, Hiroshima 734-8551, Japan; Thilo Hackert, MD, Department of Surgery, University of Heidelberg, Im Neuenheimer Feld 110, 69120 Heidelberg, Germany
S- Editor Wang JL L- Editor Logan S E- Editor Lin YP
| 1. | Grimm H, Meyer WH, Nam VC, Soehendra N. New modalities for treating chronic pancreatitis. Endoscopy. 1989;21:70-74. |
| 2. | Morgan DE, Smith JK, Hawkins K, Wilcox CM. Endoscopic stent therapy in advanced chronic pancreatitis: relationships between ductal changes, clinical response, and stent patency. Am J Gastroenterol. 2003;98:821-826. |
| 3. | Binmoeller KF, Jue P, Seifert H, Nam WC, Izbicki J, Soehendra N. Endoscopic pancreatic stent drainage in chronic pancreatitis and a dominant stricture: long-term results. Endoscopy. 1995;27:638-644. |
| 4. | Rösch T, Daniel S, Scholz M, Huibregtse K, Smits M, Schneider T, Ell C, Haber G, Riemann JF, Jakobs R. Endoscopic treatment of chronic pancreatitis: a multicenter study of 1000 patients with long-term follow-up. Endoscopy. 2002;34:765-771. |
| 5. | Eleftherladis N, Dinu F, Delhaye M, Le Moine O, Baize M, Vandermeeren A, Hookey L, Devière J. Long-term outcome after pancreatic stenting in severe chronic pancreatitis. Endoscopy. 2005;37:223-230. |
| 6. | Costamagna G, Bulajic M, Tringali A, Pandolfi M, Gabbrielli A, Spada C, Petruzziello L, Familiari P, Mutignani M. Multiple stenting of refractory pancreatic duct strictures in severe chronic pancreatitis: long-term results. Endoscopy. 2006;38:254-259. |
| 7. | Baron TH, Morgan DE. Dilation of a difficult benign pancreatic duct stricture using the Soehendra stent extractor. Gastrointest Endosc. 1997;46:178-180. |
| 8. | Park do H, Kim MH, Moon SH, Lee SS, Seo DW, Lee SK. Feasibility and safety of placement of a newly designed, fully covered self-expandable metal stent for refractory benign pancreatic ductal strictures: a pilot study (with video). Gastrointest Endosc. 2008;68:1182-1189. |
| 9. | Kawamoto H, Ishida E, Ogawa T, Okamoto Y, Mizuno O, Nakanishi T, Fukatsu H, Kato J, Okada H, Shiratori Y. Dissection of a refractory pancreatic-duct stricture by using a pre-cutting needle-knife. Gastrointest Endosc. 2006;63:190-192. |
| 10. | Kahl S, Zimmermann S, Genz I, Glasbrenner B, Pross M, Schulz HU, Mc Namara D, Schmidt U, Malfertheiner P. Risk factors for failure of endoscopic stenting of biliary strictures in chronic pancreatitis: a prospective follow-up study. Am J Gastroenterol. 2003;98:2448-2453. |