Published online Mar 21, 2010. doi: 10.3748/wjg.v16.i11.1402
Revised: January 17, 2010
Accepted: January 24, 2010
Published online: March 21, 2010
AIM: To determine the effect of three digestive tract reconstruction procedures on pouch function, after radical surgery undertaken because of gastric cancer, as assessed by radionuclide dynamic imaging.
METHODS: As a measure of the reservoir function, with a designed diet containing technetium-99m (99mTc), the emptying time of the gastric substitute was evaluated using a 99mTc-labeled solid test meal. Immediately after the meal, the patient was placed in front of a γ camera in a supine position and the radioactivity was measured over the whole abdomen every minute. A frame image was obtained. The emptying sequences were recorded by the microprocessor and then stored on a computer disk. According to a computer processing system, the half-emptying actual curve and the fitting curve of food containing isotope in the detected region were depicted, and the half-emptying actual curves of the three reconstruction procedures were directly compared.
RESULTS: Of the three reconstruction procedures, the half-emptying time of food containing isotope in the Dual Braun type esophagojejunal anastomosis procedure (51.86 ± 6.43 min) was far closer to normal, significantly better than that of the proximal gastrectomy orthotopic reconstruction (30.07 ± 15.77 min, P = 0.002) and P type esophagojejunal anastomosis (27.88 ± 6.07 min, P = 0.001) methods. The half-emptying actual curve and fitting curves for the Dual Braun type esophagojejunal anastomosis were fairly similar while those of the proximal gastrectomy orthotopic reconstruction and P type esophagojejunal anastomosis were obviously separated, which indicated bad food conservation in the reconstructed pouches.
CONCLUSION: Dual Braun type esophagojejunal anastomosis is the most useful of the three procedures for improving food accommodation in patients with a pouch and can retard evacuation of solid food from the reconstructed pouch.
- Citation: Li DS, Xu HM, Han CQ, Li YM. Effects on the pouch of different digestive tract reconstruction modes assessed by radionuclide scintigraphy. World J Gastroenterol 2010; 16(11): 1402-1408
- URL: https://www.wjgnet.com/1007-9327/full/v16/i11/1402.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i11.1402
Patterns and functions of digestive tract reconstruction after gastrectomy play a vital role in the quality of life of patients. As to which reconstruction after gastrectomy provides the least complications and best quality of life, much research has been carried out. Most of these studies focus on the function of the pouch built by surgery, including volume of the pouch, storage time of food in the pouch, and emptying mode of the food. In previous studies, most judgments were made from the subjective experience of the inspector, which cannot reveal the true state of the reconstructed pouch function. There is a long way to go, as regards further research, before we know which kind of reconstruction mode will provide patients with a good quality of life with the least problems after gastrectomy is performed.
Radionuclide dynamic imaging is the gold standard for measuring emptying time of the gastrointestinal tract[1,2]. It has been used to measure gastric emptying function when there is abnormal digestive function with normal anatomy. This is a simple technique and its best advantage is that there is seldom impact from the inspector or subject, and results reflect the actual empty time of the pouch based on objective facts. The method is simple and non-invasive, requiring a single oral administration of the radionuclide tracer. The meal used in the procedure does not alter the normal physiology of the gut. It is possible with this imaging to judge whether a reconstructed pouch matches normal physiological function. The aim of the present study was to quantify pouch emptying time of a solid meal in patients who had undergone gastrectomy surgery by calculating their half-emptying time (T1/2) values.
This study was conducted in patients who had undergone total and proximal gastrectomy for gastric cancer after a period of 6-36 mo, and who were surviving without cancer. Total number was 34 cases, and the average age of the patients was 28-72 years. Three operation procedures were conducted as follows: proximal gastrectomy orthotopic reconstruction, 10 cases; total gastrectomy P type esophagojejunal anastomosis, 11 cases; total gastrectomy Dual Braun type esophagojejunal anastomosis, 13 cases. Clinical data are displayed in Table 1.
| Clinical data | Reconstruction mode | ||
| Proximal gastrectomy (n = 10) | P type (n = 11) | Dual-Braun (n = 13) | |
| Gender | |||
| Male | 7 | 8 | 8 |
| Female | 3 | 3 | 5 |
| mean age (yr) | 61 | 57 | 59 |
| General type | |||
| Borrmann I | 0 | 0 | 0 |
| Borrmann II | 6 | 4 | 4 |
| Borrmann III | 4 | 7 | 9 |
| Borrmann IV | 0 | 0 | 0 |
| Staging | |||
| Early cancer | 1 | 0 | 2 |
| IB | 2 | 2 | 3 |
| II | 4 | 4 | 3 |
| IIIA | 2 | 4 | 4 |
| IIIB | 1 | 1 | 1 |
Meal preparation: The solid test meal was prepared by mixing 1 mCi non-absorbable containing technetium-99m (99mTc)-DTPA with 100 g flour, a 50 g raw egg and 80 mL clear water (thus containing protein 12.9 g, fat 15.4 g, carbohydrate 72.9 g); this was mixed to a paste. A pancake was heated in a microwave oven for 3 min. Each test meal offered 1814 kJ of calorific energy.
Scintigraphic measurements: Patients were supplemented with potassium chlorate 15 min before scanning, in order to block out hypothyroid and gastric mucosa influence and speed up the excretion of remnant 99mTc. Emission images were taken by a γ camera. All the patients ate the test meal within a 5 min period. Immediately after the meal, the patient was placed in front of a γ camera in a supine position, representing 0 min, and radioactivity was measured over the whole abdomen. The whole detection process took 90 min, and a frame image was collected approximately every minute. One frame image was consequently obtained which was stored in a computer disk, to measure the period and image of nuclide attenuation. Areas of interest corresponding to the gastric substitute were outlined, and the radioactivity was counted on each image and expressed as the percentage of ingested activity. After revising the half life of 99mTc and calculating every emission count of every image, the half-emptying actual curve and fitting curve of food containing isotopes in the detected region were depicted according to the computer analyzing processing system.
Two regions from each patient were investigated as follows: upper esophagus anastomosis, detecting reflux; food accommodation region after reconstruction, detecting half-emptying time of food containing the nuclide.
The half-emptying actual curve and fitting curve of the radionuclide were analyzed, and the actual half-emptying time of food containing the nuclide was compared among the three different reconstruction procedures using group comparison. Data analyzed among groups: differences in age and postoperative time among groups were tested by variance analysis, and there was no significance among groups; variance analysis of the actual half-emptying time compared between groups was conducted by Mann-Whitney test, and results were considered to be significant at P < 0.05.
No differences in esophagus reflux were found during the experiment between the three groups and no increment of isotope radioactivity was detected in the lower esophagus. Increments of isotope radioactivity were detected in the pouch region among some patients, which revealed that the actual curve of half-emptying descended initially and then ascended.
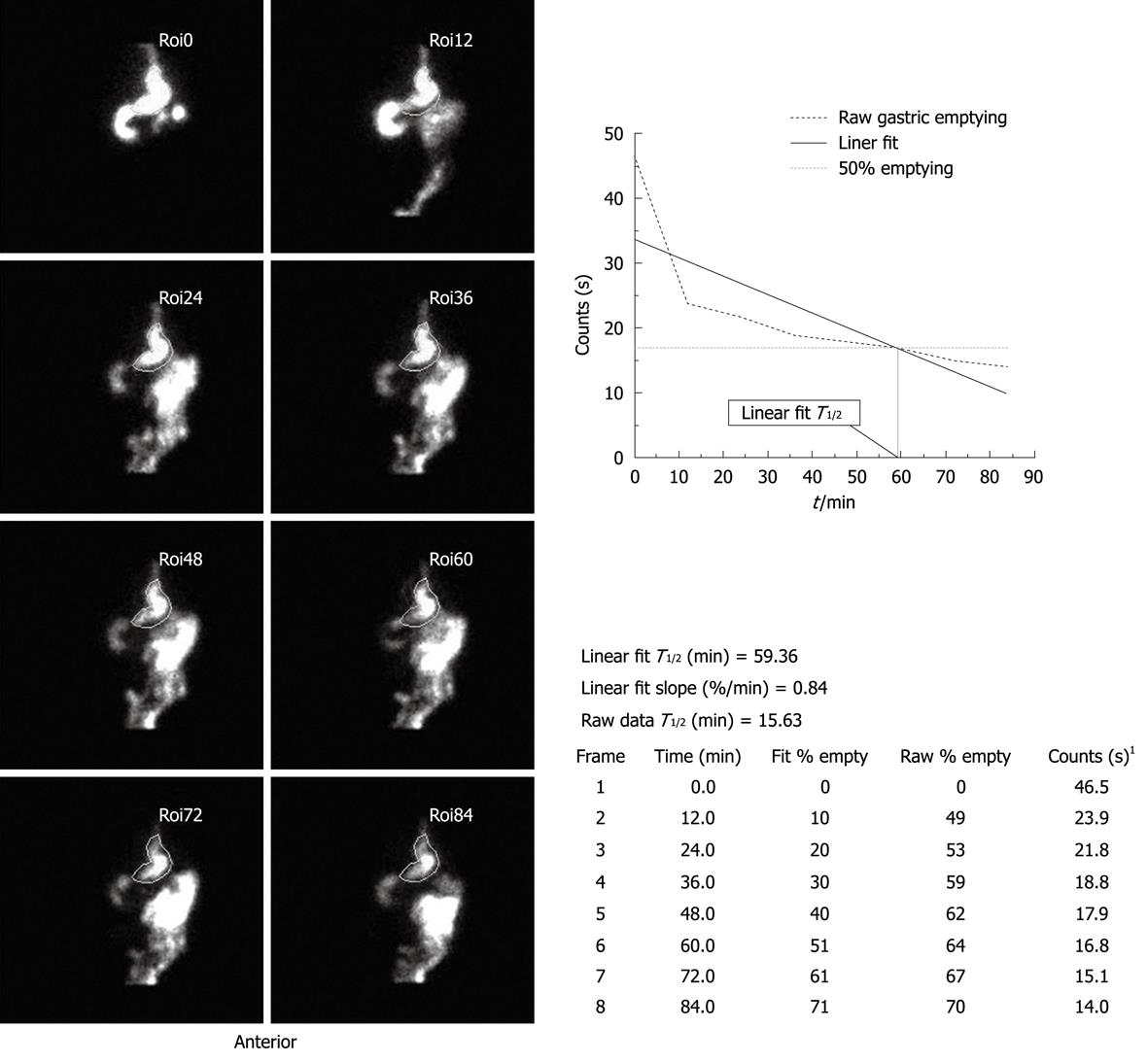
Proximal gastrectomy: The half-emptying time of the isotope markedly decreased (30.07 ± 15.77 min) with great significance compared to the Dual Braun procedure (51.86 ± 6.43 min). The actual and fitting curves were rather separated. After dietary intake for 20 min, time approached half-emptying, showing a poor food capacity in the remnant stomach (Figure 1).
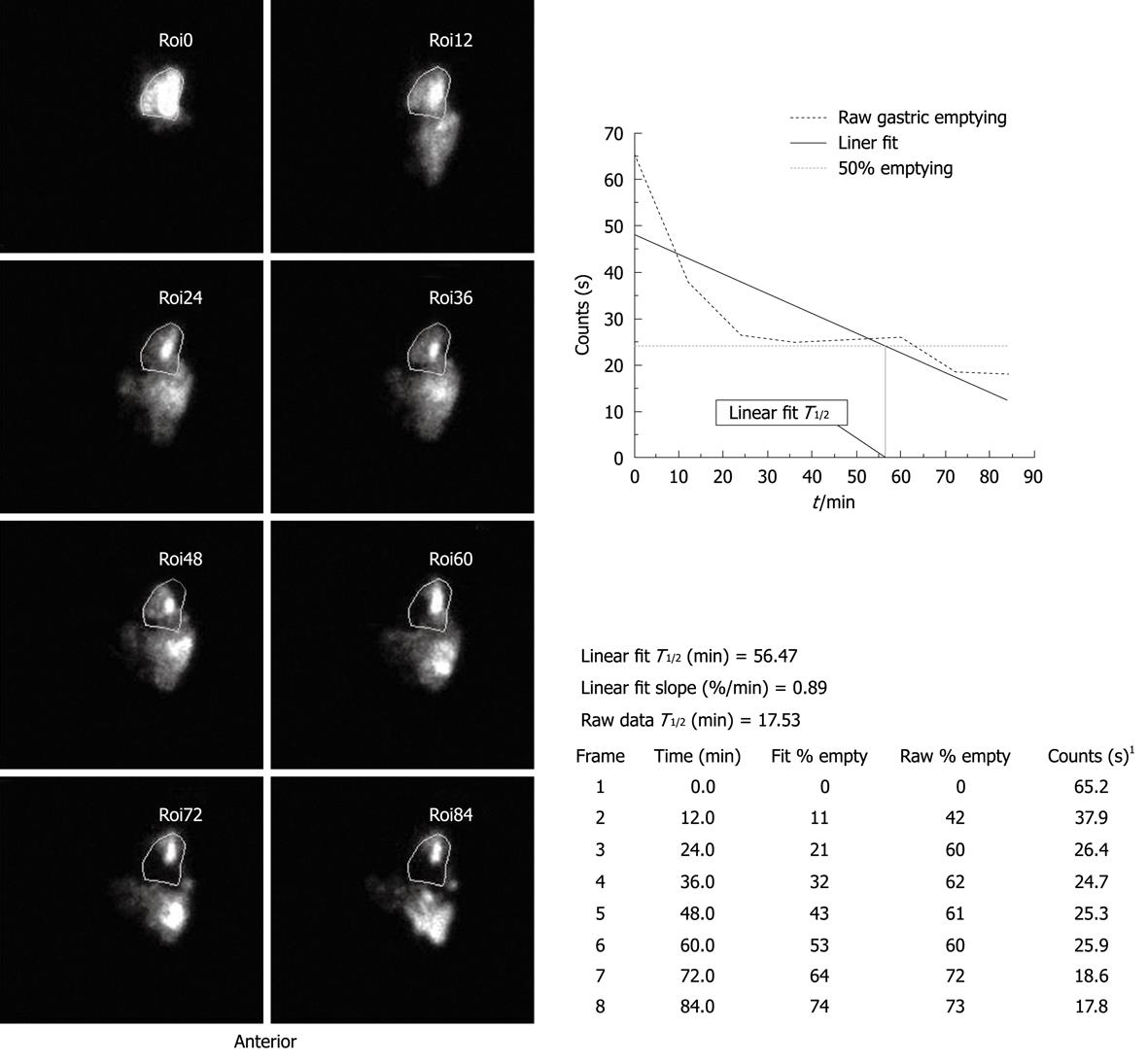
P type reconstruction: Half-emptying time (27.88 ± 6.07 min) was close to that of the proximal procedure. This reconstruction had a significantly shorter transit time compared to the Dual Braun procedure. The actual and fitting curves were rather separated, which showed a poor accommodation of food in the pouch (Figure 2).
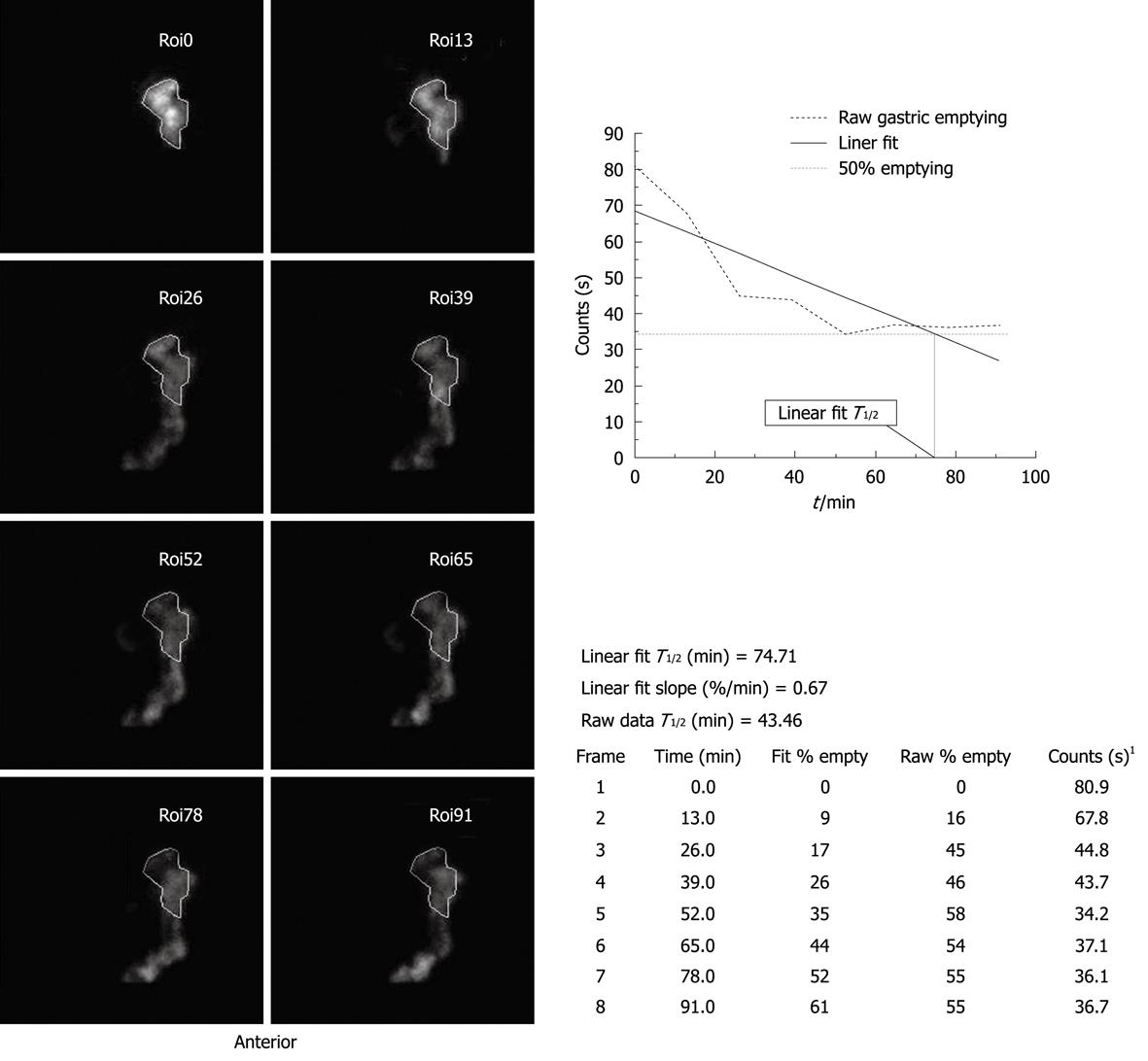
Dual Braun type esophagojejunal anastomosis: Emptying time of this procedure was 51.86 ± 6.43 min, not far from normal (60.00 ± 10.00 min), and its actual and fitting curves were fairly similar, which revealed that the reconstructed pouch could play a role in retarding the excretion of food (Figure 3).
Of the three kinds of reconstruction mode, the differences in emptying time have significant statistical relevance when compared among groups (Table 2).
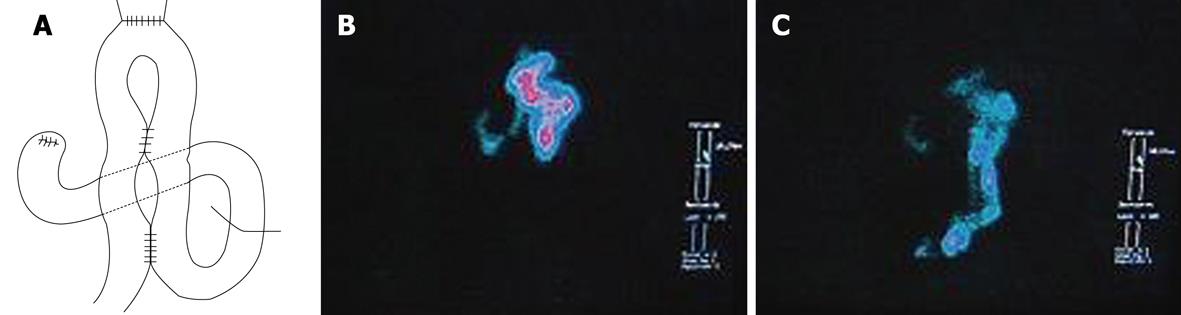
As seen from emptying images of patients having the proximal gastrectomy procedure and the total gastrectomy P type reconstruction procedure, a strong isotope development was found outside the detected region with the increasing of time, which revealed that food could not be discharged evenly from the pouch, but in an integral transferred manner. However, the double circles of the Dual Braun reconstruction procedure could retard food emptying (Figure 4).
In order to improve the quality of life of patients postoperatively, functions of digestive tract reconstructions after gastrectomy have been frequently studied by many researchers. A consensus was reached that radionuclide dynamic imaging is the most desirable method among a host of techniques used to detect effectiveness of digestive tract reconstruction. This method is simple and easy to perform; it is a non-invasive examination without any pain and is preferred by patients. Moreover, the results are not affected by subjective factors, and thus reflect pouch efficacy after digestive tract reconstruction objectively.
It has been over 100 years since Schlatter reported the first successful total gastrectomy with reconstruction. During that period, gastric carcinoma surgical techniques evolved into extended resection and ultra-extended resection. Currently, these have been converted into diminution and rational therapeutic protocols. Though many operation protocols have changed with time, they all tightly stick to the principles of radical treatment, aiming to provide security and functionality after gastric carcinoma. In recent years, studies regarding functionality of digestive tract reconstruction after gastrectomy have been progressively increasing. Different methods have their own disadvantages and advantages when viewed from different perspectives[3-12]. To determine the optimum reconstruction procedure after gastrectomy in terms of the quality of life of patients, we conducted a controlled trial to compare the pouch effectiveness of the three reconstruction procedures by radionuclide dynamic imaging.
We have previously reported a study of the same three kinds of reconstruction procedure, regarding the quality of life after operation[13]. We found Dual-Braun reconstruction provided good quality of life compared to the other two construction methods. Results showed patients put on more bodyweight and had less meal frequency. We considered that it could be the pouch that had good function with regard to digestion, so we performed this study in the same patients and confirmed that Dual Braun reconstruction can increase storage time in the pouch and empty food in a very even manner, nearly at normal levels. Therefore we proposed: (1) Proximal gastrectomy with esophagojejunal anastomosis partly preserves normal gastric tissue with easy operation, allowing a normal physiological pathway of food transit. Due to the small volume of remnant stomach and destruction of pylorus nerves, the remnant pylorus loses its routine function. As seen from the observations, food containing radionuclide was excreted fast from the remnant stomach, and thus incapable of mixing with digestive juice completely, which affects the intake of nutritional substances. The syndrome occurring when food intake of patients decreased and emptying times increased with a resultant weight loss postoperatively, was obvious clinically. The incidence of reflux was also higher postoperatively. All the results were confirmed in our subsequent review of patients; and (2) Total gastrectomy is a common resection used for gastric carcinoma, and its complications are still a cardinal factor affecting the quality of life of patients. Modification of reconstruction methods plays a positive role in avoiding postoperative complications; however, no modified protocols have received a consensus of approval. Among many modifications of pouch reconstruction and capacity, we compared P type esophagojejunal anastomosis and Dual Braun type esophagojejunal anastomosis, which has been advocated recently. In our subsequent review, we found that there was no difference in pouch capacity (food intake) between the two procedures, but from radionuclide dynamic imaging, there was an obvious difference in emptying time. One case even showed that the half-emptying time of nuclide was less than 1 min and emptying time was 3 min, as measured 24 mo after a P type procedure. The body weight of the patient decreased from 80 to 63 kg postoperatively. The patient did not undergo complete lymph node dissection and had no steatorrhea postoperatively, and had no symptoms of celiac plexus injury. Weight loss was mainly ascribed to inflexible function of the pouch in which food transited fast through the upper jejunum and nutritional substance intake was poor. The original intention of the Dual Braun procedure was to reduce reflux postoperatively and to promote functionality of the pouch. Double circles were placed after reconstruction, and the intestinal wall internal plexus was not damaged due to retention of the continuity of the jejunum, which retarded the food excretion from pouch to some extent. The half-emptying time of food containing nuclide was longer and the actual and fitting curves were similar, which showed the superiority of this reconstruction procedure.
A Dual Braun pouch provides a slower transit of food directly below the esophagus, while a double circle slows down the passage at that part of the digestive tract where the food can be mixed with bile and pancreatic juice arriving from the Y limb. This may provide a better utilization of digestive enzymes and probably leads to an improved digestion.
There was reflux noted in almost all patients after reconstruction methods of total and proximal gastrectomy, but there was no obvious reflux of food containing nuclide detected in our observations. After subsequent review, main reflux did not occur immediately after food intake, but during the period beginning from 6 min after food intake. This difference between experimental observation and clinical investigation is mainly ascribed to different detecting conditions. Our results were not in line with some other experimental reports.
Radionuclide solid gastric emptying studies have been performed clinically since 1976[14]. Many investigations published since then have confirmed the clinical utility of such studies for diagnosis of a variety of gastric motility disorders, but most of the radionuclide scintigraphy research was not in relation to reconstructed gastric tract[15-18].
The latest paper using radionuclide imaging to detect gastric emptying was published by Bernstine et al[19]; their study was to clarify whether laparoscopic sleeve gastrectomy to treat morbid obesity causes changes in gastric emptying.
Total gastrectomy is accompanied by a host of complications postoperatively, and some symptoms (i.e. malignant anemia) are unable to be avoided by operation. However, reconstruction procedures show a positive inhibitory effect on such symptoms. There are about 60 digestive tract reconstruction protocols at present; however, new prospective clinical trials should be undertaken and optimum pouch reconstruction protocols further investigated in order to ameliorate the quality of life of patients.
There are more than 60 kinds of reconstruction mode after gastrectomy. The purpose of the different modes is to diminish the complications, such as reflux and dumping syndrome, after operation and improve the quality of life. However, there is no single type of reconstruction mode commonly accepted by all researchers. Radionuclide solid gastric emptying studies have been performed clinically since 1976. Many investigations published since then have confirmed the clinical utility of such studies for diagnosis of a variety of gastric motility disorders. Nevertheless, there is a remarkable lack of standardization of this type of study and no generally applicable reference values. In particular, radionuclide studies have seldom been used in the reconstructed digestive tract.
The latest paper using radionuclide imaging to detect gastric emptying was published by Bernstine et al; their study was to clarify whether laparoscopic sleeve gastrectomy to treat morbid obesity causes changes in gastric emptying. Other research was focused on different reconstruction procedures and there has not been a study comparing emptying between different reconstruction modes.
The authors use the radiolabeled solid food to detect and compare the functions of the postoperative gastric tract, to contrast the pouch function between three kinds of reconstructed pouch. Compared with other research, the authors have used simultaneous patient follow up data to demonstrate their results.
The authors have concluded through their study that the Dual-Braun procedure was a good mode of reconstruction; it has a comparative emptying time to normal digestive tract (gastric). Radionuclide scintigraphy is a very useful method to detect the emptying time of the reconstructed pouch, is very simple and non-invasive, and can be used in other kinds of pouch.
This manuscript is original, has scientific value, is well written and has clinical value for the readers.
Peer reviewer: Raul J Rosenthal, MD, FACS, FASMBS, Affiliate Associate Professor of Surgery and Chairman, Section of Minimally Invasive Surgery, The Bariatric and Metabolic Institute; Program Director, Fellowship in Minimally Invasive Surgery, Cleveland Clinic Florida, 2950 Cleveland Clinic Blvd, Weston, FL 33331, United States
S- Editor Wang JL L- Editor Logan S E- Editor Zheng XM
| 1. | Malmud LS, Fisher RS, Knight LC, Rock E. Scintigraphic evaluation of gastric emptying. Semin Nucl Med. 1982;12:116-125. |
| 2. | Vantrappen G. Methods to study gastric emptying. Dig Dis Sci. 1994;39:91S-94S. |
| 3. | Shiraishi N, Adachi Y, Kitano S, Kakisako K, Inomata M, Yasuda K. Clinical outcome of proximal versus total gastrectomy for proximal gastric cancer. World J Surg. 2002;26:1150-1154. |
| 4. | Korenaga D, Orita H, Okuyama T, Moriguchi S, Maehara Y, Sugimachi K. Quality of life after gastrectomy in patients with carcinoma of the stomach. Br J Surg. 1992;79:248-250. |
| 5. | Thybusch-Bernhardt A, Schmidt C, Küchler T, Schmid A, Henne-Bruns D, Kremer B. Quality of life following radical surgical treatment of gastric carcinoma. World J Surg. 1999;23:503-508. |
| 6. | Wu CW, Hsieh MC, Lo SS, Lui WY, P'eng FK. Quality of life of patients with gastric adenocarcinoma after curative gastrectomy. World J Surg. 1997;21:777-782. |
| 7. | Buhl K, Lehnert T, Schlag P, Herfarth C. Reconstruction after gastrectomy and quality of life. World J Surg. 1995;19:558-564. |
| 8. | Miyoshi K, Fuchimoto S, Ohsaki T, Sakata T, Ohtsuka S, Takakura N. Long-term effects of jejunal pouch added to Roux-en-Y reconstruction after total gastrectomy. Gastric Cancer. 2001;4:156-161. |
| 9. | Tomita R, Fujisaki S, Tanjoh K, Fukuzawa M. Relationship between jejunal interdigestive migrating motor complex and quality of life after total gastrectomy with Roux-en-Y reconstruction for early gastric cancer. World J Surg. 2003;27:159-163. |
| 10. | Choi D, Yoo CH, Park H, Lee YR, Kook SH, Chung EC. Proximal gastrectomy and jejunal pouch interposition: radiographic evaluation of postoperative findings. Abdom Imaging. 2003;28:4-7. |
| 11. | Shimamoto C, Hirata I, Hiraike Y, Takeuchi N, Nomura T, Katsu K. Evaluation of gastric motor activity in the elderly by electrogastrography and the (13)C-acetate breath test. Gerontology. 2002;48:381-386. |
| 12. | Nadrowski L. Is a distal jejunojejunal pouch nutritionally ideal in total gastrectomy? Am J Surg. 2003;185:349-353. |
| 13. | Li DS, Xu HM. The quality of life of gastric cancer patients with and without duodenal passage reconstructions after total gastrectomy. Chin J Clin Oncol. 2005;2:810-814. |
| 14. | Meyer JH, MacGregor IL, Gueller R, Martin P, Cavalieri R. 99mTc-tagged chicken liver as a marker of solid food in the human stomach. Am J Dig Dis. 1976;21:296-304. |
| 15. | Ziessman HA, Fahey FH, Atkins FB, Tall J. Standardization and quantification of radionuclide solid gastric-emptying studies. J Nucl Med. 2004;45:760-764. |
| 16. | Benini L, Sembenini C, Heading RC, Giorgetti PG, Montemezzi S, Zamboni M, Di Benedetto P, Brighenti F, Vantini I. Simultaneous measurement of gastric emptying of a solid meal by ultrasound and by scintigraphy. Am J Gastroenterol. 1999;94:2861-2865. |
| 17. | Tougas G, Eaker EY, Abell TL, Abrahamsson H, Boivin M, Chen J, Hocking MP, Quigley EM, Koch KL, Tokayer AZ. Assessment of gastric emptying using a low fat meal: establishment of international control values. Am J Gastroenterol. 2000;95:1456-1462. |
| 18. | Guo JP, Maurer AH, Fisher RS, Parkman HP. Extending gastric emptying scintigraphy from two to four hours detects more patients with gastroparesis. Dig Dis Sci. 2001;46:24-29. |