Published online Nov 7, 2009. doi: 10.3748/wjg.15.5224
Revised: September 18, 2009
Accepted: September 25, 2009
Published online: November 7, 2009
We report a case of jejunoileal intussusception in a 42-year-old patient with Crohn’s disease caused by a gastrointestinal stromal tumor. The patient complained of vague diffuse abdominal pain for a period of 4 mo. Intussusception was suspected at computer tomography and magnetic resonance imaging scans. Segmental resection of the small intestine was performed. Pathological examination of the surgical specimen revealed a gastrointestinal stromal tumor as well as aphthous ulcerations and areas of inflammation, which were characteristic of Crohn’s disease. This is the first report of small bowel intussusception due to a gastrointestinal stromal tumor coexisting with Crohn’s disease.
- Citation: Theodoropoulos GE, Linardoutsos D, Tsamis D, Stamopoulos P, Giannopoulos D, Zagouri F, Michalopoulos NV. Gastrointestinal stromal tumor causing small bowel intussusception in a patient with Crohn’s disease. World J Gastroenterol 2009; 15(41): 5224-5227
- URL: https://www.wjgnet.com/1007-9327/full/v15/i41/5224.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.5224
Intussusception, defined as the telescoping of a segment of the gastrointestinal tract into an adjacent one, is extremely rare in the stomach, but more common in the small intestine, ileocecal junction and colon. It is the leading cause of intestinal mechanical obstruction and the second most common surgical emergency in children[1]. However, it is rather infrequent in adults, accounting for 0.1% of all surgical admissions and 1%-5% of mechanical bowel obstructions[2]. In these cases, it is frequently related to malignancy.
Gastrointestinal stromal tumors (GISTs) are a subset of mesenchymal tumors of varying differentiation. They are rare clinical entities, constitute less than 3% of all gastrointestinal malignant neoplasms and represent only 20% of small-bowel malignant neoplasms (excluding lymphoma)[3]. With the improvement on immunohistochemical staining techniques and ultrastructural evaluation, GISTs are recognized as a distinct group of mesenchymal tumors now[4].
In the current report, we present a case of a 45-year-old man with Crohn’s disease complaining of intermittent vague abdominal pain for a period of 4 mo. Enteroclysis, computer tomography (CT) and magnetic resonance imaging (MRI) abdominal scans showed small bowel intussusception, a diagnosis which was confirmed after surgical exploration of the abdomen where a tumor causing a jejunoileal intussusception was identified. Pathological examination of the surgical specimen revealed a gastrointestinal stromal tumor as well as inflammation and aphthous ulcerations, which were characteristic of Crohn’s disease involving small bowel. Coexistence of these clinical entities resulting in intussusception has never been reported in the literature.
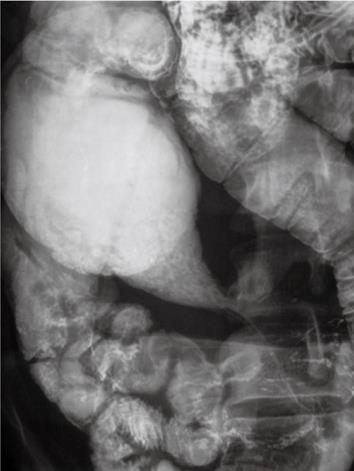
A 45-year-old man with symptoms of bowel obstruction was admitted to the surgical department of our hospital in April, 2008. He complained of diffuse blunt abdominal pain preceded by two episodes of vomiting and obstipation. The patient reported similar attacks of milder episodes, consisting of intermittent abdominal pain and bloating for the past 4 mo. He was diagnosed as Crohn’s disease following gastroenterological evaluation with colonoscopy and terminal ileum biopsies at sites of ileitis 1 year ago on the grounds of chronic diarrhea, cramp abdominal pain attacks and mild anemia. The patient did not receive any regular medication. Physical examination showed mild abdominal distention with slight tenderness and hypoactive bowel sounds. No mass was palpated and rectal examination did not reveal any blood or malignancy. Routine laboratory tests and chest films were normal. However, abdominal plain radiographs showed some small bowel air-fluid levels. The patient underwent a CT scan with po and intravenous contrast of 5-mm thick slice, which showed thickening of the distal ileum wall and an intraluminal mass resulting in partial obstruction of the small intestine. Sagittal fast spin echo (FSE) T2, FSE T2 with fat suppression and axial FSE T1 with 5-mm thick slice abdominal MRI (Figure 1) fortified the suspicion of intussusception since it showed a pathognomonic bowel within bowel configuration. In order to secure the diagnosis, an enteroclysis was performed, which showed a jejunoileal stricture caused by invagination of the jejunum into the ileum and proximal to the stenosis bowel dilatation (Figure 2).
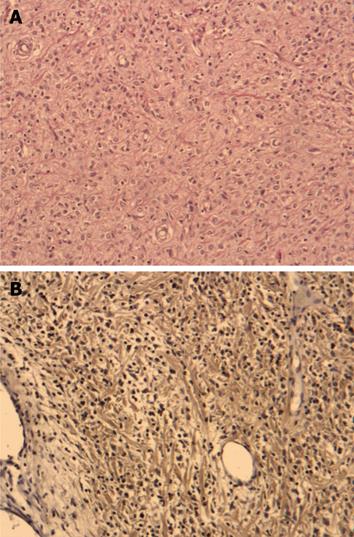
Taking into account the high possibility of a malignant mass causing bowel intussusception in an adult patient, laparoscopic approach was not considered in this case, in order to achieve the best possible oncologic clearance at the surgical intervention that followed. So, the patient underwent a laparotomy which identified a jejunoileal intussusception (Figure 3). An approximately 20-cm partial small bowel resection including wide margins and a wedge resection of the respective mesentery up to the beginning of the feeding vessels were performed. The bowel lumen was longitudinally opened immediately following removal of the specimen and an exophytic round-shaped mass of smooth circumference approximately 6 cm in maximum diameter, which was hard at palpation, was easily appreciated. Pathological examination of the surgical specimen proved the lesion to be a stromal tumor with an immunohistochemical profile of c-kit (+), S-100 (-), SMA (-), desmin (-), EMA (-), CD34 (-), AE1/AE3 CK8.18 (-), NSE (-), and synaptophysin (-). The tumor was invading the muscularis propria layer at the point of the intussusception (Figure 4A and B). No lymph node infiltration was identified. Microscopic examination of the remaining specimen disclosed findings consistent with Crohn’s disease. The lesion contained aphthous ulcerations and showed severe polymorphonuclear and lymphocytic infiltration as well as eosinophils and intraluminal abscesses.
The continuity of the small bowel was restored with a side-to-side entero-enteral anastomosis. The patient, discharged on the 7th postoperative day, following an uncomplicated recovery, was subjected to follow-up with clinical examinations and CT scans at 6-mo intervals and had no clinical or radiologic recurrence at the time when we wrote this paper.
Tumors of the small intestine are rare and usually benign. The majority of them are leiomyomas, but adenocarcinomas and GISTs, although uncommon, may also appear. Conventional histologic methods could not produce correct diagnoses and most tumors referred to as leiomyomas and leiomyosarcomas in the older medical literature are actually GISTs. On the basis of immunohistochemical and ultrastructural studies, GISTs are mesenchymal tumors of the gastrointestinal tract that may show myogenic and/or neurogenic characteristics[5], and are usually asymptomatic, but they have been reported to present with bleeding, obstruction or perforation in some cases[6].
Intussusception is the invagination of one bowel loop and its mesentery into the bowel lumen distal to it. It occurs when a proximal segment of intestine (intussusceptum) telescopes into the intestinal segment distal to it (intussuscipiens), and is the second most common complication when tumors locate in the ileum[7]. Invaginations of the lumen may also cause gastrointestinal bleeding or necrosis of the tumor. Usually patients have slightly enlarging tumors with no rapid onset. Their complaints are usually non specific and it is finally risky to miss the diagnosis. Our patient experienced vague abdominal pain for a period of 4 mo which led him to undergo a colonoscopy that came up normal.
Intussusception is correctly diagnosed preoperatively in only one-third of cases[7]. An accurate diagnosis of intussusception should include a good and specific medical history, a thorough physical examination, radiography, CT, MRI and enteroclysis or even an endoscopic ultrasound or capsule endoscopy. Ultrasound is useful in confirming obstruction and may sometimes identify the cause[8]. However, it is highly operator-dependent. Taking into account the rarity of such findings, it requires an experienced radiologist. In our case, ultrasound was not diagnostic of intussusception. It has been recently reported that CT and MRI offer great help in establishing the preoperative diagnosis of intussusception[9]. On CT, one can diagnose a bowel intussusception within its configuration, thickening of the wall and compressed mesenteric fat and vessels[9]. Although not routinely reported in such cases, an abdominal MRI, like in our report, can aid to establish the preoperative diagnostic suspicion of intussusception.
In contrast to childhood where intussusception is idiopathic in 90% of cases and the basic underlying cause of intussusception is the hypertrophy of Payer’s patches activity, adult intussusception has a definable pathologic lesion in over 90% of cases, with neoplasms considered to be the cause in 65% of them[10]. Any intraluminal lesion, especially polyps, which irritates and alters normal peristaltic activity, is able to trigger an intraluminal invagination finally causing an intussusception. Subsequent peristaltic bowel activity produces an area of sequence constriction and relaxation, thus telescoping the leading point through the distal bowel lumen[11]. The malignancy is more likely to be located in the colon rather than in the small bowel. Less common etiologies of intussusception in adults include postoperative factors (adhesions, suture lines, etc.), polyps, Meckel’s disease, sprue, cecal duplication and intramural hematoma[1]. The presentation of adult intussusception is usually subacute or chronic[2]. The most common symptoms are crampy abdominal pain, nausea, vomiting, abdominal distention or tenderness. Only up to 20% of all cases present with complete bowel obstruction and acute onset[10]. Moreover, it has been reported that a palpable mass is present in 7%-42% of the cases[11].
In the literature, five cases of small bowel intussusception from a stromal tumor in adults have been described[5,6,10,12,13]. The most recent one was an intraluminal leiomyoma of the small intestine in a 72-year-old female patient, which resulted in invagination and partial obstruction of the jejunum[12]. Another recent report presented a case of a 60-year-old woman with a jejunoileal intussusception due to a myxoid stromal tumor[10]. Others described a GIST as the cause of intussusception in a 32-year-old man and emphasized the role of ultrasound in preoperative diagnosis of the disease[13]. In an older report[5], a case of a 42-year-old patient with intussusception of the lower jejunum was presented and the patient was admitted with progressive anemia, massive melena and lower abdominal pain. Finally, a malignant GIST of the small intestine causing small bowel obstruction due to ileal invagination has also been described[6].
Coincidence of Crohn’s disease and gastrointestinal stromal tumor is extremely rare and only two cases have been reported to date[14,15]. The first one described a polypoid tumor within Meckel’s diverticulum in an 81-year-old male patient with Crohn’s disease and the tumor was immunohistochemically proved to be a GIST[14]. The second report presented a 51-year-old patient with a high risk GIST of the terminal ileum within an area of Crohn’s ileitis[15].
Conclusively, in the present report we describe a case of a 42-year-old man with no significant medical history other than a 4-mo intermittent dull abdominal pain who presented with symptoms of acute bowel obstruction. Laparotomy revealed a jejunoileal intussusception and histological examination of the surgical specimen indicated a GIST tumor causing the intussusception as well as patchy areas of inflammation and erosions similar to those identified in Crohn’s disease. Coexistence of these pathologically distinct and extremely rare entities has not been reported and represents a unique finding.
Peer reviewer: Gianlorenzo Dionigi, MD, FACS, ESES, ETA, Asscociate Professor of Surgery, Department of Surgical Sciences, University of Insubria, Ospedate di Circolo, v. guicciardini, 21100 Varese, Italy
S- Editor Tian L L- Editor Wang XL E- Editor Zheng XM
| 1. | Akçay MN, Polat M, Cadirci M, Gencer B. Tumor-induced ileo-ileal invagination in adults. Am Surg. 1994;60:980-981. |
| 2. | Tan KY, Tan SM, Tan AG, Chen CY, Chng HC, Hoe MN. Adult intussusception: experience in Singapore. ANZ J Surg. 2003;73:1044-1047. |
| 3. | Nishida T, Hirota S. Biological and clinical review of stromal tumors in the gastrointestinal tract. Histol Histopathol. 2000;15:1293-1301. |
| 4. | Kim CJ, Day S, Yeh KA. Gastrointestinal stromal tumors: analysis of clinical and pathologic factors. Am Surg. 2001;67:135-137. |
| 5. | Hoshino N, Murata T, Oka K, Kawakami K, Hoshino K, Sekoguchi S, Suga T, Nishimura A, Kato M, Hamada M. Gastrointestinal stromal tumors of the small intestine that expressed c-kit protein. Intern Med. 2000;39:914-919. |
| 6. | Occhionorelli S, Mitaritonno M, Pennella A, Carella M, Presicce L, Pellegrini D, Fiore MG, Pollinzi Fonte V. Gastro-intestinal stromal tumor (GIST): case report. G Chir. 2001;22:65-69. |
| 7. | Badreldina R, Bowling T. Disorders of the small bowel. Surgery (Oxford). 2008;26:338-342. |
| 8. | Nylund K, Ødegaard S, Hausken T, Folvik G, Lied GA, Viola I, Hauser H, Gilja OH. Sonography of the small intestine. World J Gastroenterol. 2009;15:1319-1330. |
| 9. | Sundaram B, Miller CN, Cohan RH, Schipper MJ, Francis IR. Can CT features be used to diagnose surgical adult bowel intussusceptions? AJR Am J Roentgenol. 2009;193:471-478. |
| 10. | Akçay MN, Aydinli B, Gürsan N, Balik AA, Onbaş O, Oztürk G. Intussusception in an adult patient with mild intermittent abdominal pain. Dig Dis Sci. 2005;50:1127-1129. |
| 12. | Sunamak O, Karabicak I, Aydemir I, Aydogan F, Guler E, Cetinkaya S, Korman MU. An intraluminal leiomyoma of the small intestine causing invagination and obstruction: a case report. Mt Sinai J Med. 2006;73:1079-1081. |
| 13. | Vijay S, Dahiya N, Sudha P. Radiology for the surgeon: soft-tissue case 56. Small-bowel intussusception. Can J Surg. 2004;47:453-455. |
| 14. | Mijandrusić Sincić B, Kovac D, Jasić M, Grbas H, Uravić M, Depolo A. Crohn's disease and a gastrointestinal stromal tumor in an 81-year-old man--a rare coincidence. Zentralbl Chir. 2005;130:597-599. |