Published online Jul 14, 2009. doi: 10.3748/wjg.15.3276
Revised: June 11, 2009
Accepted: June 18, 2009
Published online: July 14, 2009
AIM: To explore the impact of fecal incontinence (FI) on quality of life (QOL) of patients attending urogynecology and colorectal clinics (CCs).
METHODS: Cross-sectional study of 154 patients (27 male) with FI, who attended the clinics at a regional hospital in North Queensland, Australia in 2003 and 2004, and completed the Fecal Incontinence Quality of Life Scale (FIQL: 1 = very affected; 4 = not affected).
RESULTS: More than 22% of patients had their QOL affected severely by FI. Patients reported that they had not previously been asked about FI by a medical practitioner nor did they voluntarily disclose its presence. The median FIQL scores for all participants were: lifestyle = 3.24; coping = 2.23; depression = 2.42; and embarrassment = 2.33. Increasing frequency of soiling had a negative effect on all four FIQL scales (P < 0.001) as did the quantity of soiling (P < 0.01). Female CC patients had poorer FIQL scores than urogynecology clinic patients for lifestyle (P = 0.015), coping (P = 0.004) and embarrassment (P = 0.009), but not depression (P = 0.062), despite having experienced FI for a shorter period.
CONCLUSION: Failure to seek treatment for FI degrades the quality of patients’ lives over time. FI assessment tools should incorporate the quantity of fecal loss.
- Citation: Bartlett L, Nowak M, Ho YH. Impact of fecal incontinence on quality of life. World J Gastroenterol 2009; 15(26): 3276-3282
- URL: https://www.wjgnet.com/1007-9327/full/v15/i26/3276.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.3276
Fecal incontinence (FI) is the involuntary discharge of liquid or solid stools. FI severity has been described as a combination of the frequency and type of stools, the severity of urgency, and frequency of pad usage[12]. This problem affects both men and women, irrespective of social, employment or financial status[34]. The prevalence of FI increases with age[56] and Australian studies have reported some of the highest rates in the world[578].
People with mild fecal loss such as staining are unwilling to admit to themselves that they have an FI problem[9]. As the problem worsens and patients inevitably accept that they have FI, they are reluctant to disclose the problem to others[9–15], with only 5%-27% seeking help from their doctors[15]. Lack of disclosure may be to the result of embarrassment, the erroneous belief that FI is a normal part of aging, or the perception that no treatment is available. Doctors may fail to comprehend patient hints about diarrhea and FI[15] or may be reluctant to ask about fecal leakage, perhaps because of their own embarrassment or the perception that FI is a trivial concern[16].
FI can range from causing mild embarrassment to becoming an insidious burden on the person’s quality of life (QOL)[17–21]. Tools used to measure the impact of FI on QOL have been under development for 20 years and include lifestyle components in summary scales, generic measures, disease-specific measures, utility measures, and more recently, direct questioning of objective measures[1]. The Fecal Incontinence Quality Of Life (FIQL) questionnaire, a disease-specific tool, was designed to evaluate the impact of FI on four aspects of patients’ QOL: lifestyle; coping behavior; depression or self perception; and level of embarrassment. Each aspect is described as a score measured on a scale between 1 and 4, where 1 is very affected and 4 is not affected[22]. Validity and reliability of the FIQL have been established and it has been recommended as a useful tool to assess FI[23].
This study was designed to explore the impact of FI on the QOL of patients attending urogynecology and colorectal surgical outpatient clinics at a publicly funded regional hospital with a large rural catchment[24].
Participants were consecutive patients attending the colorectal clinic (CC) and urogynecology clinic (UC) at The Townsville Hospital, in North Queensland Australia, between January and June 2003 and August and November 2004. Ethical approval was obtained from the ethics committees of Townsville Hospital and James Cook University.
The study procedure has been described previously[59]. Briefly, a cross-sectional survey was conducted among patients at the CC and UC. On arrival, all patients attending these clinics were invited to participate in the study. Exclusion criteria included children (under 18 years), pregnancy, terminal illness, mental illness, or gastrointestinal stoma. Eligible subjects completed a patient consent form. Participants were then given a self-administered questionnaire that contained questions about patient demographics, alcohol consumption, preexisting medical conditions, and prior surgical history; all known risk factors for FI. Patients who answered “yes” to the question “do you ever accidentally soil your clothes or underclothes with feces?” proceeded to questions relating to the frequency, severity and management of FI, and the 29 question FIQL survey tool[22]. The physicians of participating patients also surveyed them using the Cleveland Clinic Florida Fecal Incontinence Score[25], which was compared with the self-administered survey tool results to investigate disclosure problems[9]. Here, we report information about the QOL questions from the self-administered questionnaire.
Mean and SD were used to describe age. Medians and interquartile ranges were used as measures of central tendency and estimates for dispersion for duration of FI and FIQL scales. FIQL scales were calculated in accordance with the developers recommendations[26]. For bivariate testing of categorical variables, exact versions of χ2 tests were conducted for nominal items, while exact trend tests were used for ordinal variables. Multiple linear regressions were used to investigate relationships between FIQL scales and clinics, basic severity (type × frequency) and duration of FI among female participants, and FIQL scales and components of severity[2], with and without quantity of fecal loss, in all participants. Potential components were initially considered separately and were then combined. As FIQL scales were not distributed normally, they were transformed by taking the square root. As no major differences between transformed and untransformed regression results were found, the untransformed regression data have been presented. Results of linear regression analyses are presented by regression coefficients (r) with 95% CIs and/or P values. A significance level of 0.05 was adopted a priori.
The recruitment methodology and tools used were the same in 2003 and 2004. There were no differences in age (P = 0.603), sex (P = 0.149) or prevalence of FI (P = 0.076) in participants between the two recruitment periods, thus the data were combined for analysis.
A total of 769 patients (451 in 2003 and 318 in 2004) were invited to participate. Of these, 423 women attended the UC and 146 men and 200 women attended the CC, with 93.4% (n = 718) of the eligible patients completing the self-administered FI questionnaire. As 43 patients completed the survey more than once, the initial responses were used and duplicate data were removed from the combined database, which left a total of 675 unique entries.
Of the 675 patients in the study 154 (22.8%; 95% CI: 19.6%-26.0%) reported having accidentally soiled their clothes or underclothes with feces and answered the FIQL questions. There were 27 men from the CC, and 127 women, 52 from the CC and 75 from the UC, with FI. The mean age (SD) of the participants with FI was 56.2 (14.3) years. There was no age difference between sexes (P = 0.281) or clinics (P = 0.82), or the women attending the two clinics (P = 0.87).
Patients reported the following etiological risk factors for FI. There were 27 participants who reported having bowel disease (25 from CC, nine male), with 14 of them (all from CC, two male) having been diagnosed with colorectal cancer. Twenty seven women (eight from CC) had undergone vaginal repair surgery, whilst 51 women (16 from CC) reported difficult vaginal births using forceps, vacuum extraction or long second-stage labor. Twenty-one participants (11 from CC, two male) reported rectal prolapse; 23 (20 from CC, nine male) had undergone surgery for hemorrhoids, anal fissures or fistulas; 101 (39 from CC, 10 male) had urinary incontinence; 11 (six from CC, four male) had anal injuries; 18 (10 from CC, four male) had diabetes; six (four from CC, two male) reported spinal cord disease; three (one from CC, one male) had neurological disease; 39 (21 from CC, seven male) reported chronic constipation; and 17 women (five from CC) had psychiatric problems that required medication. Some patients had multiple factors.
Patients attending the UC documented having FI for a significantly longer period (median: 24 mo, IQR: 12-60), than those attending the CC [12 (6-24), P = 0.001). Similarly, women in the UC clinic had FI for longer than those in the CC clinic [UC = 24 (12-60); CC = 12 (6-24), P = 0.002].
More than half (55.8%) of the participants admitted to soiling at least once per month: 17% (25) of patients reported soiling daily, 24% (35) weekly, 15% (22) monthly, and 44% (65) less than once a month. There was no difference in the frequency of incontinent episodes between sexes (P = 0.678). However, women who attended the CC reported more frequent leakage, with 27.5% soiling daily compared with 11.0% of those in the UC (P = 0.037), possibly as a result of their bowel condition.
In the CC, significantly more men (79%) disclosed liquid bowel leakage than women (46%), whilst fewer men reported solid (8%) and combined solid/liquid (13%) leakage than women (solid = 18%, combined = 36%; P = 0.008). There was no significant difference between women attending the CC or UC with regard to type of leakage (UC: liquid bowel leakage, 46%; solid bowel leakage, 28%; combined solid/liquid bowel leakage, 25%, P > 0.05). More women attending the CC reported passive leakage (80%) than those attending the UC (62.5%, P = 0.037) or men (48%, P = 0.026). There were no differences between sexes or clinics for fecal urgency or quantity of fecal soiling.
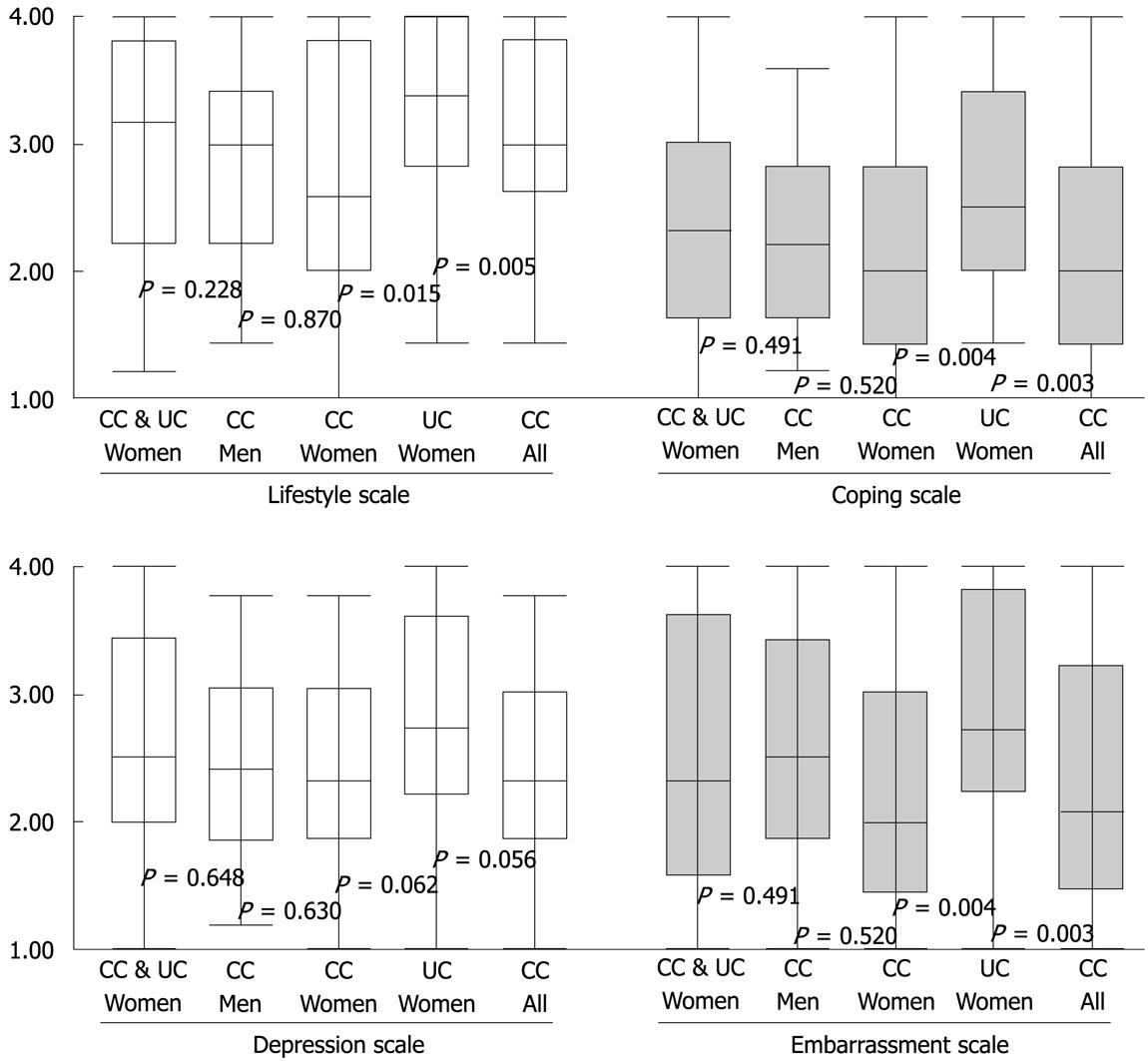
The median (IQR) results of the FIQL scales (range: 1-4; 4 = not affected) for all participants were: lifestyle = 3.24 (2.22-3.80); coping = 2.23 (1.60-3.00); depression = 2.42 (1.95-3.33); and embarrassment = 2.33 (1.67-3.58) (Table 1). Participants who attended the CC had significantly poorer scores than those who attended the UC for lifestyle (P = 0.005), coping (P = 0.003) and embarrassment (P = 0.024) but not depression (P = 0.056).
There were no significant differences in any of the FIQL scales between sexes when compared in total or within the CC (Figure 1). Women who attended the CC had lower scores on all scales compared with those who attended the UC (lifestyle: P = 0.015; coping: P = 0.004; depression: P = 0.062; embarrassment: P = 0.009; Figure 1). The four multiple linear regression analyses [FIQL = clinic + duration + basic FI severity (type × frequency) + error] used to investigate the relationships between QOL of women by clinic, FI type/frequency and duration determined that the poorer QOL results in the CC with regard to clinic and type/frequency remained significant (all P < 0.05), whilst duration of soiling remained significant for the lifestyle, depression and embarrassment scales (all P < 0.05) but not for the coping scale (P = 0.103, Table 2).
| Lifestyle | P | Coping | P | Depression | P | Embarrassment | P | |
| CC | -0.582 (-0.938, -0.225) | 0.002 | -0.499 (-0.835, -0.162) | 0.004 | -0.365 (-0.685, -0.045) | 0.026 | -0.568 (-0.923, -0.214) | 0.002 |
| Duration (mo) | -0.002 (-0.004, 0.000) | 0.042 | -0.002 (-0.004, 0.000) | 0.103 | -0.002 (-0.004, 0.000) | 0.041 | -0.003 (-0.005, 0.000) | 0.020 |
| Severity (1-8)1 | -0.159 (-0.241, -0.076) | < 0.001 | -0.176 (-0.255, -0.097) | < 0.001 | -0.143 (-0.216, -0.069) | < 0.001 | -0.207 (-0.290, -0.124) | < 0.001 |
Increasing frequency and quantity of soiling had a significant negative effect across all four QOL scales (frequency, P < 0.001; quantity, P < 0.01). QOL was poorer in participants with greater urgency and passive soiling, whilst those participants who documented both solid and liquid bowel leakage had poorer QOL than those with either alone. Not all scales reached significance (Table 3). When comparing QOL between female participants who attended the CC and UC, the scores for frequency, quantity, type and fecal urgency were significantly poorer across all FIQL scales for female participants in the CC (P < 0.05). Women who reported passive FI in the CC had poorer QOL scores than those in the UC for lifestyle (P = 0.040), coping (P = 0.020), depression (P = 0.181), and embarrassment (P = 0.019).
| Categorical variables | Scale 1: lifestyle1 | Scale 2: coping1 | Scale 3: depression1 | Scale 4: embarrassment1 | ||||||||
| n(missing) | Median (IQR)2 | P value | n(missing) | Median (IQR)2 | P value | n(missing) | Median (IQR)2 | P value | n(missing) | Median (IQR)2 | P value | |
| Frequency of fecal soiling (seven cases not stated) | ||||||||||||
| Daily | 24 (1) | 2.10 (1.33-2.91) | < 0.001a | 24 (1) | 1.33 (1.18-1.83) | < 0.001a | 23 (2) | 1.71 (1.37-2.29) | < 0.001a | 23 (2) | 1.46 (1.00-2.07) | < 0.001a |
| Weekly | 31 (4) | 3.10 (2.40-3.60) | 32 (3) | 2.26 (1.47-2.82) | 30 (5) | 2.54 (2.06-3.08) | 30 (5) | 2.33 (1.33-3.00) | ||||
| Monthly | 18 (4) | 3.30 (2.60-3.70) | 18 (4) | 2.14 (1.94-2.82) | 19 (3) | 2.29 (1.77-3.38) | 19 (3) | 2.33 (2.00-3.33) | ||||
| Less often | 48 (17) | 3.70 (2.85-4.00) | 54 (11) | 2.88 (2.15-3.57) | 52 (13) | 3.02 (2.19-3.66) | 50 (15) | 3.00 (2.33-4.00) | ||||
| Type of fecal soiling (eight cases not stated) | ||||||||||||
| Liquid | 59 (16) | 3.26 (2.50-3.80) | 0.077a | 64 (11) | 2.44 (1.78-3.11) | 0.024a | 62 (13) | 2.78 (2.14-3.57) | 0.005a | 62 (13) | 2.67 (2.00-3.67) | 0.003a |
| Solid | 24 (7) | 3.37 (2.60-3.93) | 27 (4) | 2.33 (1.63-3.22) | 27 (4) | 2.64 (2.09-3.50) | 25 (6) | 2.33 (1.83-3.67) | ||||
| Both | 35 (5) | 3.00 (1.50-3.70) | 38 (2) | 2.00 (1.26-2.50) | 37 (3) | 2.19 (1.60-2.57) | 36 (4) | 2.00 (1.33-2.67) | ||||
| Quantity of fecal soiling (four cases not stated) | ||||||||||||
| Minimal soiling | 65 (18) | 3.60 (3.00-4.00) | < 0.001a | 71 (12) | 2.67 (2.17-3.40) | < 0.001a | 69 (14) | 2.80 (2.20-3.61) | 0.001a | 69 (14) | 2.67 (2.00-3.67) | 0.010a |
| Major soiling | 41 (11) | 3.00 (2.06-3.55) | 46 (6) | 2.06 (1.44-2.58) | 45 (7) | 2.27 (1.89-2.92) | 43 (9) | 2.32 (2.00-3.00) | ||||
| Soiling outer clothes | 8 (1) | 2.12 (1.63-2.45) | 8 (1) | 1.28 (1.14-1.46) | 8 (1) | 2.00 (1.72-2.59) | 7 (2) | 1.67 (1.33-2.33) | ||||
| Soiling furniture | 5 (1) | 1.30 (1.25-1.95) | 5 (1) | 1.00 (1.00-2.14) | 5 (1) | 1.37 (1.19-2.28) | 5 (1) | 1.00 (1.00-2.67) | ||||
| Fecal urgency (four cases not stated) | ||||||||||||
| Never | 15 (10) | 4.00 (3.30-4.00) | 0.001a | 16 (9) | 3.40 (2.24-3.76) | < 0.001a | 20 (5) | 2.45 (2.19-3.40) | 0.177a | 17 (8) | 2.67 (1.56-3.83) | 0.507a |
| Sometimes | 88 (21) | 3.25 (2.22-3.70) | 98 (11) | 2.24 (1.60-2.96) | 92 (17) | 2.48 (1.88-3.37) | 91 (18) | 2.33 (2.00-3.33) | ||||
| Always | 15 (1) | 2.30 (1.80-2.60) | 15 (1) | 1.50 (1.33-2.06) | 15 (1) | 2.24 (1.77-2.64) | 15 (1) | 2.00 (1.33-3.33) | ||||
| Women only UC-ever | 47 (11) | 3.30 (2.70-3.80) | 0.005b | 52 (6) | 2.44 (1.79-3.11) | 0.002b | 50 (8) | 2.72 (2.08-3.56) | 0.034b | 49 (9) | 2.67 (2.00-3.67) | 0.003b |
| Women only CC-ever | 38 (7) | 2.45 (1.72-3.60) | 42 (3) | 1.86 (1.28-2.44) | 39 (6) | 2.24 (1.65-2.86) | 39 (6) | 2.00 (1.33-2.67) | ||||
| Passive fecal soiling (seven cases not stated) | ||||||||||||
| Never | 38 (12) | 3.40 (2.67-4.00) | 0.086a | 41 (9) | 2.56 (1.97-3.42) | 0.049a | 43 (7) | 3.05 (2.28-3.66) | 0.008a | 40 (10) | 3.33 (2.33-4.00) | < 0.001a |
| Sometimes | 63 (16) | 3.10 (2.20-3.60) | 69 (10) | 2.17 (1.56-2.78) | 65 (14) | 2.23 (1.80-2.90) | 64 (15) | 2.00 (1.42-2.92) | ||||
| Always | 15 (3) | 2.50 (1.70-3.90) | 17 (1) | 2.06 (1.39-3.20) | 17 (1) | 2.27 (1.90-3.39) | 17 (1) | 2.00 (1.00-2.96) | ||||
| Women only UC-ever | 36 (9) | 3.30 (2.76-3.82) | 0.040b | 39 (6) | 2.44 (1.78-3.22) | 0.020b | 39 (6) | 2.48 (1.94-3.27) | 0.181b | 38 (7) | 2.33 (1.92-3.00) | 0.019b |
| Women only CC-ever | 33 (7) | 2.50 (1.61-3.60) | 37 (3) | 1.91 (1.28-2.44) | 34 (6) | 2.20 (1.70-2.86) | 34 (6) | 1.83 (1.33-2.67) | ||||
The model (FIQL = frequency + type + urgency + pad use + error) used to investigate the relationships between the four FIQL scales and the components of severity showed that the significant components that affected QOL were frequency and fecal urgency with regard to lifestyle and coping (all P < 0.05); and frequency and type with regard to depression and embarrassment (all P < 0.05). As a result of the low rate of pad usage (36% wore pads), passive leakage (68% reported) was included in the model, and the quantity of fecal loss was also investigated. This amended model (Table 4) showed: daily, solid, and large losses of stool to be significant factors for lifestyle (P < 0.05); monthly and daily leakage, urgency, pad wearing and large quantities of fecal loss to be significant factors for coping (P < 0.05); frequent and major leakage of both solid and liquid stool were significant factors for depression (P < 0.05); whilst frequent, solid and liquid, and passive stool loss significantly affected embarrassment (P < 0.05).
| Components of FI severity | FIQL scales | |||
| Lifestyle | Coping | Depression | Embarrassment | |
| Frequency | ||||
| Monthly | 0.061 | 0.002 | 0.008 | 0.006 |
| Weekly | 0.241 | 0.846 | 0.531 | 0.595 |
| Daily | < 0.001 | 0.012 | 0.023 | 0.021 |
| Type | ||||
| Solid | 0.010 | 0.192 | 0.515 | 0.633 |
| Both solid/liquid | 0.254 | 0.085 | 0.007 | 0.014 |
| Urgency | ||||
| Sometimes | 0.961 | 0.325 | 0.565 | 0.888 |
| Always | 0.106 | 0.023 | 0.554 | 0.636 |
| Wears pads | 0.209 | 0.022 | 0.488 | 0.107 |
| Passive leakage | ||||
| Sometimes | 0.659 | 0.169 | 0.103 | 0.787 |
| Always | 0.626 | 0.485 | 0.252 | 0.007 |
| Quantity of leakage | ||||
| Major (Requires immediate underwear change) | 0.001 | < 0.001 | 0.004 | 0.096 |
| Soiling of outer clothes | 0.023 | 0.217 | 0.969 | 0.405 |
| Soiling of furniture/bedding | 0.578 | 0.781 | 0.381 | 0.662 |
The major findings of this study were that more than 22% of patients who attended the UC and CC in 2003 and 2004 for matters other than FI had their QOL severely affected by FI, with the QOL of participants who attended the CC being poorer than that of those from the UC. Furthermore, the negative impact on participants’ lives worsened with the loss of both solid and liquid stool and the increased frequency and quantity of soiling.
In this study of the impact on QOL of FI in rural and regional north Queensland, our overall FIQL results for lifestyle (3.24), coping (2.23), depression (2.42) and embarrassment (2.33) were within the range of comparable clinic-based studies in other countries[21–31], and closely reflected the scores found in a similar study conducted at a Pelvic Floor Center in Minnesota, USA[21] and baseline scores from two Victorian (Australia) clinical studies that investigated injectable material for FI[3233].
The QOL of patients who attended the CC was more severely affected than that of participants from the UC, even though they had reported FI for a shorter duration. There were no significant differences between those who had a diagnosis of bowel disease and those who did not. Thus the poorer QOL in CC participants may be a direct result of recent colorectal surgery, in which the sudden and unexpected onslaught of FI was more devastating than for the UC participants who may have learnt to cope with their progressive FI over an extended time period. These CC FIQL results are comparable with previously published results from a pouch, non-pouch study[29], but the participants in our study were less able to cope, and were more depressed and embarrassed, although this did not affect their lifestyle to the same degree.
The UC patients’ QOL scores were lower than those in a similar study in Texas, USA[30] but higher than in the study in Minnesota, USA[21], for lifestyle, coping and embarrassment, but not depression. This difference may have been caused by a longer duration with FI in the older cohorts in our study and the Minnesota study, (mean age 56 years), compared with the younger cohort in the Texas study (mean age 39 years). This suggests that older women with FI had poorer QOL than younger affected women, which implies that delaying treatment for this condition results in poorer QOL over time.
This study investigated the relationship between FI severity and the FIQL scales individually and collectively. A negative impact was found on patients’ lives, which increased with frequency of soiling. This was evident on all scales of the FIQL, but there was little difference in each of the FIQL scales between weekly and monthly incontinent episodes. This lack of difference may be because an incontinent episode that occurs infrequently is unexpected, and hence, would be similarly distressing.
The data collected for pad wearing was dichotomous, which may explain why only significant results for the coping scale were obtained. If, in addition, the number of pads worn per day had been assessed, the embarrassment scale may also have reached significance.
The type of soiling affected participants’ QOL differently. Patients with both solid and liquid soiling reported a poorer QOL than those with either solid or liquid only incontinent episodes. This is consistent with the Texas study in which a liquid component of anal incontinence was reported to have a greater impact upon QOL of participants than either flatal or non-liquid incontinence[30].
The association between quantity of fecal loss and FIQL scales was found to be highly significant. Patients with the most soiling, i.e. those who soiled furniture, had the lowest possible FIQL score for coping and embarrassment, and performed only marginally better on the lifestyle and depression scales. There are few reports of the relationship between quantity of fecal loss and QOL, however, a Japanese study investigating the QOL of patients following total proctocolectomy and ileal J-pouch-anal anastomosis determined that greater soiling resulted in higher levels of frustration, which is an anxiety measure calculated using a Japanese translation of Cattell’s anxiety scale[34]. When quantity was included in the FIQL/severity regression model, it was found to be significant (P < 0.05) for the lifestyle, coping and depressions scales, but did not reach significance for the embarrassment scale (P = 0.065). Given this relationship between the FIQL scales and quantity of fecal soiling, it is suggested that the definition of FI severity should include quantity of fecal loss as well as frequency, type, urgency and pad wearing.
In conclusion, to the best of our knowledge, this is the first study to measure the effect of FI on QOL of people in rural and regional Australia. More than 22% of the patients attending the UC and CC in North Queensland, for matters other than FI, had their QOL severely affected by this condition. Patients reported that they had not been asked about FI by their general practitioners or hospital physicians, nor did they voluntarily disclose its presence[9]. Women who have obstetric-injury-related FI suffer in silence, and their QOL deteriorates as they age. The definition of FI severity should include quantity of fecal loss[35]. Further community-based research in Australia is warranted in regard to the impact of FI on QOL of people who suffer with this complaint.
As many as one in seven adults suffer with fecal incontinence (FI), which can have a devastating effect on the lifestyle of people with frequent, ad hoc or large amounts of fecal seepage. These people often fail to seek treatment due to embarrassment, believing the problem is uniquely theirs, or because they are unaware of the existence of available treatments.
Patients referred to urogynecology and colorectal surgical clinics, for other reasons, have a high incidence of FI. They do not seek assistance whilst attending these clinics from physicians who can recommend or refer for treatment. In this study, the authors demonstrated the impact that FI had on these patients’ quality of life (QOL).
Recent reports have highlighted the impact conservative treatments, such as biofeedback, and more invasive treatments, such as injectable bulking agents, sacral nerve stimulation, artificial bowel sphincter and dynamic graciloplasty, have had on the QOL of patients with FI. This study reports that despite these improvements many people continue to suffer unaware of such advances.
By understanding more than one in five patients attending colorectal and urogynecological clinics have their QOL severely affected by FI, attending physicians can enable access to treatment by directly asking patients about this problem.
FI is the involuntary discharge of solid or liquid stools.
FI severity, including the quantity of stool loss, can have a severe negative impact on QOL. This is an interesting and relevant study that deals with a demanding subject.
| 1. | Baxter NN, Rothenberger DA, Lowry AC. Measuring fecal incontinence. Dis Colon Rectum. 2003;46:1591-1605. |
| 2. | Bharucha AE, Locke GR 3rd, Seide BM, Zinsmeister AR. A new questionnaire for constipation and faecal incontinence. Aliment Pharmacol Ther. 2004;20:355-364. |
| 3. | Miner PB Jr. Economic and personal impact of fecal and urinary incontinence. Gastroenterology. 2004;126:S8-S13. |
| 4. | Deutekom M, Dobben AC, Dijkgraaf MG, Terra MP, Stoker J, Bossuyt PM. Costs of outpatients with fecal incontinence. Scand J Gastroenterol. 2005;40:552-558. |
| 5. | Ho YH, Muller R, Veitch C, Rane A, Durrheim D. Faecal incontinence: an unrecognised epidemic in rural North Queensland? Results of a hospital-based outpatient study. Aust J Rural Health. 2005;13:28-34. |
| 6. | Whitehead WE, Borrud L, Goode PS, Meikle S, Mueller ER, Tuteja A, Weidner A, Weinstein M, Ye W. Fecal Incontinence in US Adults: Epidemiology and Risk Factors. Gastroenterology. 2009;13:Epub ahead of print. |
| 7. | Lam TCF, Kennedy ML, Chen FC, Lubowski DZ, Talley NJ. Prevalence of faecal incontinence: obstetric and constipation-related risk factors; a population-based study. Colorectal Dis. 1999;1:197-203. |
| 8. | Kalantar JS, Howell S, Talley NJ. Prevalence of faecal incontinence and associated risk factors; an underdiagnosed problem in the Australian community? Med J Aust. 2002;176:54-57. |
| 9. | Bartlett L, Nowak M, Ho YH. Reasons for non-disclosure of faecal incontinence: a comparison between two survey methods. Tech Coloproctol. 2007;11:251-257. |
| 11. | Drossman DA, Sandler RS, Broom CM, McKee DC. Urgency and fecal soiling in people with bowel dysfunction. Dig Dis Sci. 1986;31:1221-1225. |
| 12. | Enck P, Bielefeldt K, Rathmann W, Purrmann J, Tschöpe D, Erckenbrecht JF. Epidemiology of faecal incontinence in selected patient groups. Int J Colorectal Dis. 1991;6:143-146. |
| 13. | Johanson JF, Lafferty J. Epidemiology of fecal incontinence: the silent affliction. Am J Gastroenterol. 1996;91:33-36. |
| 14. | Edwards NI, Jones D. The prevalence of faecal incontinence in older people living at home. Age Ageing. 2001;30:503-507. |
| 15. | Whitehead WE. Diagnosing and managing fecal incontinence: if you don't ask, they won't tell. Gastroenterology. 2005;129:6. |
| 16. | Stevens TK, Soffer EE, Palmer RM. Fecal incontinence in elderly patients: common, treatable, yet often undiagnosed. Cleve Clin J Med. 2003;70:441-448. |
| 17. | Rothbarth J, Bemelman WA, Meijerink WJ, Stiggelbout AM, Zwinderman AH, Buyze-Westerweel ME, Delemarre JB. What is the impact of fecal incontinence on quality of life? Dis Colon Rectum. 2001;44:67-71. |
| 18. | Colquhoun P, Kaiser R Jr, Efron J, Weiss EG, Nogueras JJ, Vernava AM 3rd, Wexner SD. Is the quality of life better in patients with colostomy than patients with fecal incontience? World J Surg. 2006;30:1925-1928. |
| 19. | Deutekom M, Terra MP, Dobben AC, Dijkgraaf MG, Baeten CG, Stoker J, Bossuyt PM. Impact of faecal incontinence severity on health domains. Colorectal Dis. 2005;7:263-269. |
| 20. | Damon H, Dumas P, Mion F. Impact of anal incontinence and chronic constipation on quality of life. Gastroenterol Clin Biol. 2004;28:16-20. |
| 21. | Bordeianou L, Rockwood T, Baxter N, Lowry A, Mellgren A, Parker S. Does incontinence severity correlate with quality of life? Prospective analysis of 502 consecutive patients. Colorectal Dis. 2008;10:273-279. |
| 22. | Rockwood TH, Church JM, Fleshman JW, Kane RL, Mavrantonis C, Thorson AG, Wexner SD, Bliss D, Lowry AC. Fecal Incontinence Quality of Life Scale: quality of life instrument for patients with fecal incontinence. Dis Colon Rectum. 2000;43:9-16; discussion 16-17. |
| 23. | Avery KN, Bosch JL, Gotoh M, Naughton M, Jackson S, Radley SC, Valiquette L, Batista J, Donovan JL. Questionnaires to assess urinary and anal incontinence: review and recommendations. J Urol. 2007;177:39-49. |
| 24. | Queensland Health. The Townsville Hospital. Available from: URL: http://www.health.qld.gov.au/townsville/Facilities/tville_hosp.asp. |
| 25. | Jorge JM, Wexner SD. Etiology and management of fecal incontinence. Dis Colon Rectum. 1993;36:77-97. |
| 26. | Rockwood T. The author replies. Dis Colon Rectum. 2008;51:1434. |
| 27. | Colquhoun PH, Efron J, Wexner SD. Attainment of continence with J-pouch and artificial bowel sphincter for concomitant imperforate anus and familial adenomatous polyposis: report of a case. Dis Colon Rectum. 2004;47:538-541. |
| 28. | Rullier E, Zerbib F, Marrel A, Amouretti M, Lehur PA. Validation of the French version of the Fecal Incontinence Quality-of-Life (FIQL) scale. Gastroenterol Clin Biol. 2004;28:562-568. |
| 29. | Park JG, Lee MR, Lim SB, Hong CW, Yoon SN, Kang SB, Heo SC, Jeong SY, Park KJ. Colonic J-pouch anal anastomosis after ultralow anterior resection with upper sphincter excision for low-lying rectal cancer. World J Gastroenterol. 2005;11:2570-2573. |
| 30. | Boreham MK, Richter HE, Kenton KS, Nager CW, Gregory WT, Aronson MP, Vogt VY, McIntire DD, Schaffer JI. Anal incontinence in women presenting for gynecologic care: prevalence, risk factors, and impact upon quality of life. Am J Obstet Gynecol. 2005;192:1637-1642. |
| 31. | Pla-Martí V, Moro-Valdezate D, Alos-Company R, Solana-Bueno A, Roig-Vila JV. The effect of surgery on quality of life in patients with faecal incontinence of obstetric origin. Colorectal Dis. 2007;9:90-95. |
| 32. | Tjandra JJ, Lim JF, Hiscock R, Rajendra P. Injectable silicone biomaterial for fecal incontinence caused by internal anal sphincter dysfunction is effective. Dis Colon Rectum. 2004;47:2138-2146. |
| 33. | Tjandra JJ, Chan MK, Yeh HC. Injectable silicone biomaterial (PTQ) is more effective than carbon-coated beads (Durasphere) in treating passive faecal incontinence--a randomized trial. Colorectal Dis. 2009;11:382-389. |
| 34. | Fujita S, Kusunoki M, Shoji Y, Owada T, Utsunomiya J. Quality of life after total proctocolectomy and ileal J-pouch-anal anastomosis. Dis Colon Rectum. 1992;35:1030-1039. |
| 35. | Landefeld CS, Bowers BJ, Feld AD, Hartmann KE, Hoffman E, Ingber MJ, King JT Jr, McDougal WS, Nelson H, Orav EJ. National Institutes of Health state-of-the-science conference statement: prevention of fecal and urinary incontinence in adults. Ann Intern Med. 2008;148:449-458. |