Published online Feb 28, 2008. doi: 10.3748/wjg.14.1293
Revised: December 5, 2007
Published online: February 28, 2008
We report a case of a 32-year-old woman with episodic right lower quadrant abdominal pain. With the diagnosis of either acute appendicitis or tubo-ovarian abscess, she was treated with antibiotics, which successfully relieved the pain and the inflammatory findings. She repeated the clinical condition a few times and antibiotics worked each time. In a year, her subjective symptoms became milder, however, a giant pelvic cyst appeared. She had an exploratory laparotomy to confirm this diagnosis. Histopathological studies revealed herniated appendiceal mucosa through the muscular layer associated with chronic inflammation and marked fibrosis. Gynecological disorders such as endometriosis or lutein cyst rupture was denied. These findings represent appendiceal diverticulitis. We discuss the clinical features of the disease and its relation with the pelvic pseudocyst.
- Citation: Niwa H, Hiramatsu T. A rare presentation of appendiceal diverticulitis associated with pelvic pseudocyst. World J Gastroenterol 2008; 14(8): 1293-1295
- URL: https://www.wjgnet.com/1007-9327/full/v14/i8/1293.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.1293
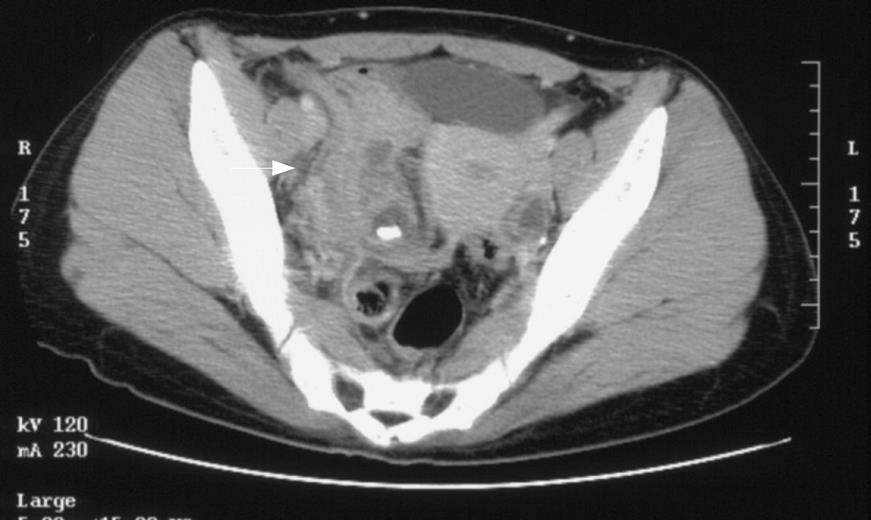
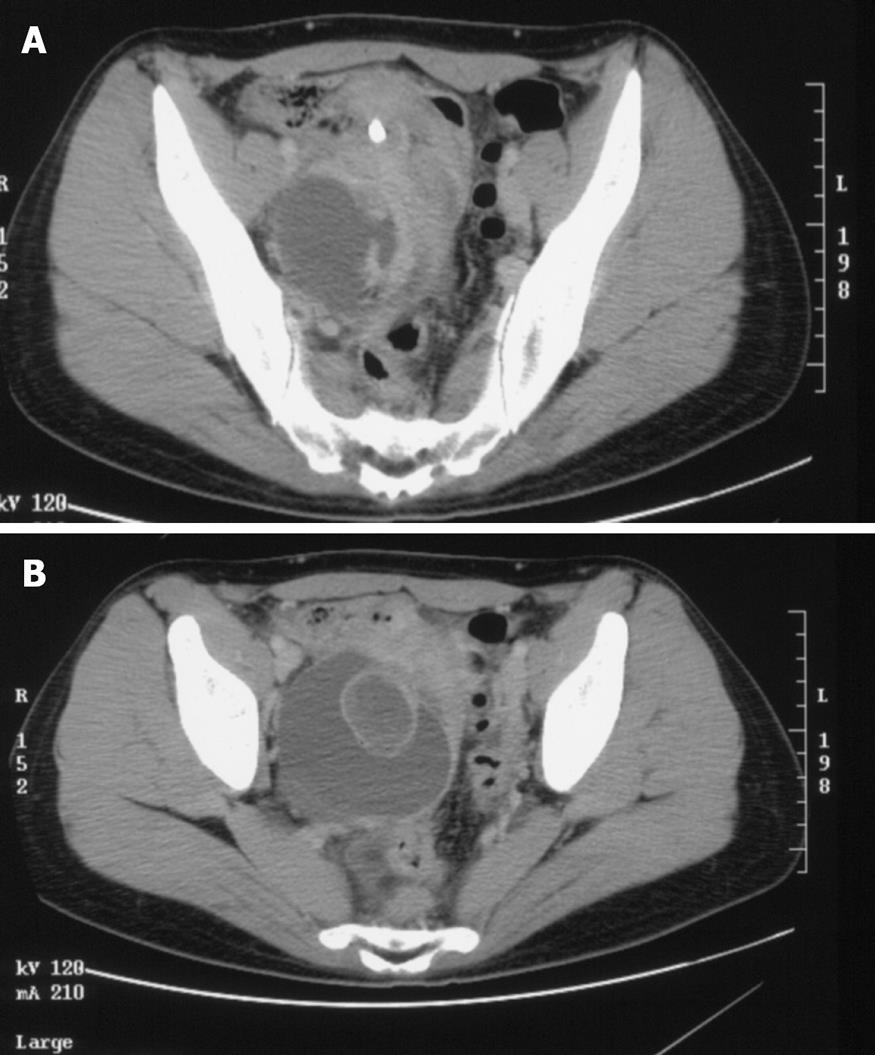
A 32-year-old woman visited our hospital with diarrhea, abdominal pain and fever. With the diagnosis of acute enteritis, an oral antibiotic was given, which resolved her symptoms. Eight months later, pain in the upper abdomen, then in the lower, appeared. Inflammatory markers such as WBC and CRP arose up to 13.0 × 109/L and 57 mg/L respectively. Ultrasonography detected no more than the wall thickening of the small intestine. Enteritis was the diagnosis and antibiotics worked again. Two months later, upper stomachache relapsed, which afterwards moved to the right lower quadrant. At this time, the pain was accompanied by remittent fever up to 39 centigrade. Pelvic CT scan showed a whip-shaped low-density structure with a high-density spot at its caudal end extending downwards along the bulging right pelvic wall which was then assumed to be the effect of inflammation (Figure 1). The lesion was thought to be either the swollen appendix with a fecal stone or tubo-ovarian abscess with calcification. In order to be effective in either case, an intravenous antibiotics, flomoxef sodium, was infused for a week, which successfully subsided the inflammatory symptoms but occasional abdominal pain. In four months, lower abdominal pain, neither accompanied by high fever nor related with gynecological episodes such as ovulation or menstruation, gradually became worse. The laboratory data suggested the presence of inflammation again, with WBC 11.7 × 109/L and CRP 45 mg/L. The outstanding finding of CT scan was a cyst in cyst structure in the pelvis, with the diameter of 3 cm and 8 cm respectively. The high density spot, without low density lesion nearby at this time, relocated cranially into the right iliac fossa and the bulging of the right pelvis disappeared (Figure 2A and B).
Though our initial diagnosis was the pelvic abscess caused by appendiceal perforation, the abscess of tubo-ovarian origin was still possible. So, laparotomy was chosen to confirm the diagnosis and the treatment.
At laparotomy, peritoneal cavity was free of ascites. The terminal ileum and the top of the uterus adhered to each other to block the exploration down the pelvic cavity. While dissecting the conglomerated organs, the dark brown serous fluid without pus-like odor or feel came out. Then, the ruptured cyst with the right ovary appeared. The atrophic appendix adhered to the back of the cecum, being entirely wrapped by dense fibrous tissue.
Though other cysts were not elsewhere as far as we explored, we tentatively made the diagnosis of ovarian endometriosis. That was because the inner wall of the cystic lesion was chocolate brown and bumpy, and in addition, the appendix lacked acute inflammatory findings. We first resected the right ovary and tube together and scraped the ruptured cystic wall as much as possible. Then appendectomy was added. She recovered well except the wound infection at the subdermal level and was discharged on the postoperative d 14. The abdominal annoyances have not recurred since then.
The pathologic examination was as follows. The cystic wall did not have any endometrial components, but had hemosiderin deposits, which suggests a pseudocyst with old bleeding. The ovarian cyst was composed of luteal body and follicles. The appendix had a mucosal protrusion in the subserosal layer near its orifice, which is thought to be a diverticulum. Only chronic inflammation was found both along the peridiverticulum and in the whole appendix.
Appendiceal diverticulum is classified as either congenital or acquired form like other intestinal diverticulum[1]. The congenital diverticulum has full layers, that is, mucosa, submucosa, muscle, and serosa, and therefore it hardly perforates. The congenital form is exceedingly rare and was found in 0.0014% in the study of a series of 50 000 appendices[2]. The acquired form lacks muscular layer, which explains its mechanical weakness and inclination to perforation[1]. The acquired one is more common and its incidence ranges from 0.004% to 2.1%[1]. Diverticula are usually located in the distal one third of the appendix[2]. A high proportion of diverticula occurs along the mesenteric border, which is structurally weak because of the existence of vascular hiatuses[3]. Although appendiceal diverticulitis presents with similar signs and symptoms to appendicitis, its clinical features are different in some ways. Appendiceal diverticulitis is seen mainly after the third decade of life while the average age of appendicitis patient is 19 years[145]. The disease is more common in men, is usually accompanied by previous attacks of pain, and presents fewer gastrointestinal symptoms[14].
Those with appendiceal diverticulitis are four times more likely to have a perforation compared with simple appendicitis, which is thought to be responsible for a longer convalescence and 30-fold more mortality[1467]. Importantly, the incidence of perforation in cases of diverticulitis was 66%[6]. However, the way of perforation, whether to free peritoneal cavity or into retroperitoneal space is not well documented. Simpson et al reported a case of diverticular abscess of the appendix in the right iliac fossa[4]. According to their CT figures, the abscess extends over to the preperitoneal space anteromedial to the right iliac crest, which implies retroperitoneal perforation of the diverticulum. Place et al reported a case of chronic appendicitis with diverticular formation of which CT finding suggested extensive inflammation in the right retroperitoneum and pericecal area[1].
Since most acquired appendiceal diverticula are on the mesoappendix, the inflammatory process may well be contained within the mesentery after perforation and cellulitis may develop in the nearby retroperitoneum. That may be one of the reasons why generalized peritonitis is uncommon in the appendiceal diverticulitis[7].
In acute appendicitis, on the contrary, perforation usually heads for the free peritoneal cavity followed by diffuse peritonitis.
In our case, we speculate that the appendiceal diverticulum also perforated into the retroperitoneal space and made phlegmon beneath the right pelvic peritoneum. Considering the above-mentioned case reports, we assume that inflamed diverticula may be apt to perforate into a less symptom presenting space, that is, retroperitoneum, at an earlier inflammatory stage. Moreover, unless appendicitis is accompanied, significant findings are hard to get by imaging tests. Prescribing antibiotics without keeping in mind the possibility of diverticulitis might just complicate the symptoms and make it insidious. Complication of a large pelvic cyst with appendiceal diverticulitis like our case has not been reported as far as we searched. Since the large cyst was not present 4 mo before and gynecological disorder such as endometriosis is pathologically unlikely, it should be related to diverticulitis. It is possible that the permeated appendiceal fluid brought about cellulites underneath the right pelvic retroperitoneum, which eventually developed the pooling of infectious exudates. We speculate that during the course of treatment, it may have re-perforated into the free pelvic cavity to form a large pseudocyst, while appendiceal diverticulitis became chronic and almost healed. The treatment strategy of appendiceal diverticulitis should depend on its degree and spread of inflammation. Because its direct diagnosis is not easy, in the patients with repeating lower abdominal pain with inflammatory findings, we should take this clinical entity into account.
We experienced a case of appendiceal diverticulitis associated with a large pelvic pseudocyst. We speculate that the appendiceal diverticulum perforated into the retroperitoneal space and made phlegmon beneath the right pelvic peritoneum, which eventually developed the pooling of infectious exudates. Then, during the course of treatment, it may have re-perforated into the free pelvic cavity to form a large pseudocyst. Since appendiceal diverticulitis has 30 times mortality compared with simple appendicitis, to recognize this disease is clinically most important.
| 1. | Place RJ, Simmang CL, Huber PJ Jr. Appendiceal diverticulitis. South Med J. 2000;93:76-79. |
| 2. | COLLINS DC. A study of 50,000 specimens of the human vermiform appendix. Surg Gynecol Obstet. 1955;101:437-445. |
| 3. | Chong KC. Diverticula of the vermiform appendix: a report of nine cases. Postgrad Med J. 1976;52:504-510. |
| 4. | Simpson J, Lobo DN, Spiller RC, Scholefield JH. Diverticular abscess of the appendix: report of a case and review of the literature. Dis Colon Rectum. 2003;46:832-834. |
| 5. | Trollope ML, Lindenauer SM. Diverticulosis of the appendix: a collective review. Dis Colon Rectum. 1974;17:200-218. |
| 6. | Lipton S, Estrin J, Glasser I. Diverticular disease of the appendix. Surg Gynecol Obstet. 1989;168:13-16. |