Published online Aug 21, 2008. doi: 10.3748/wjg.14.4909
Revised: April 16, 2008
Accepted: April 23, 2008
Published online: August 21, 2008
AIM: To compare the outcome of laparoscopic versus open appendectomy.
METHODS: Prospectively collected data from 293 consecutive patients with acute appendicitis were studied. These comprised of 165 patients who underwent conventional appendectomy and 128 patients treated laparoscopically. The two groups were compared with respect to operative time, length of hospital stay, postoperative pain, complication rate and cost.
RESULTS: There were no statistical differences regarding patient characteristics between the two groups. Conversion to laparotomy was necessary in 2 patients (1.5%). Laparoscopic appendectomy was associated with a shorter hospital stay (2.2 d vs 3.1 d, P = 0.04), and lower incidence of wound infection (5.3% vs 12.8%, P = 0.03). However, in patients with complicated disease, intra-abdominal abscess formation was more common after laparoscopic appendectomy (5.3% vs 2.1%, P = 0.002). The operative time and analgesia requirements were similar in the two groups. The cost of treatment was higher by 370 € in the laparoscopic group.
CONCLUSION: Laparoscopic appendectomy is as safe and efficient as open appendectomy, provided surgical experience and equipment are available.
-
Citation: Kehagias I, Karamanakos SN, Panagiotopoulos S, Panagopoulos K, Kalfarentzos F. Laparoscopic
versus open appendectomy: Which way to go? World J Gastroenterol 2008; 14(31): 4909-4914 - URL: https://www.wjgnet.com/1007-9327/full/v14/i31/4909.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.4909
| Open appendectomy | Laparoscopic appendectomy | P | |
| Number of patients | 165 | 128 | |
| Male (%) | 55.1 | 44.5 | 0.33 |
| Female (%) | 44.9 | 55.5 | 0.38 |
| Mean age | 33.4 ± 18 | 33.8 ± 17.8 | 0.44 |
| WBC count | 15497 ± 3000/mm3 | 15728 ± 2793/mm3 | 0.80 |
| Co-morbidities (%) | |||
| CAD | 6 (3.6) | 5 (3.9) | 0.63 |
| Hypertension | 13 (7.8) | 9 (7) | 0.71 |
| COPD | 5 (3) | 4 (3.1) | 0.27 |
| DM | 6 (3.6) | 3 (2.3) | 0.14 |
| Open appendectomy | Laparoscopic appendectomy | P | |
| Intraoperative findings (%) | |||
| Normal appendix | 16 (9.6) | 8 (6.2) | 0.20 |
| Acute appendicitis | 102 (61.8) | 82 (64) | 0.72 |
| Gangrenous appendicitis | 19 (11.5) | 20 (15.6) | 0.17 |
| Appendiceal abscess | 19 (11.5) | 12 (9.3) | 0.32 |
| Peritonitis | 9 (5.4) | 6 (4.6) | 0.14 |
| Mean operative time (min) | 47 ± 19.7 | 44.3 ± 24 | 0.31 |
| Open appendectomy | Laparoscopic appendectomy | P | |
| Uncomplicated disease | 118 | 90 | |
| Wound infection | 1 (0.8) | 0 (0) | 0.01 |
| Bowel injury | 0 (0) | 1 (1.1) | < 0.001 |
| Morbidity (%) | 0.8 | 1.1 | 0.5 |
| Complicated disease | 47 | 38 | |
| Wound infection | 6 (12.8) | 2 (5.3) | 0.03 |
| Intra-abdominal abscess | 1 (2.1) | 2 (5.3) | 0.002 |
| Bowel obstruction | 5 (10.6) | 3 (7.9) | 0.37 |
| Respiratory infection | 4 (8.5) | 2 (5.3) | 0.18 |
| Morbidity | 34 | 23.7 | 0.12 |
| Total morbidity (%) | 10.3 | 7.8 | 0.43 |
The introduction of laparoscopic surgery has dramatically changed the field of surgery. With improvements in the equipment and increasing clinical experience it is now possible to perform almost any kind of procedure under laparoscopic visualization.
Although more than a century has elapsed since McBurney first performed open appendectomy[1], this procedure remains the treatment of choice for acute appendicitis for most surgeons.
In 1983, Semm performed the first laparoscopic appendectomy[2]. Ever since then, the efficiency and superiority of laparoscopic approach compared to the open technique has been the subject of much debate[3-23]. The idea of minimal surgical trauma, resulting in significantly shorter hospital stay, less postoperative pain, faster return to daily activities, and better cosmetic outcome has made laparoscopic surgery for acute appendicitis very attractive. However, several retrospective studies[3-12], several randomized trials[13-19] and meta-analyses[20-24] comparing laparoscopic with open appendectomy have provided conflicting results. Some of these studies have demonstrated better clinical outcomes with the laparoscopic approach[13-17], while other studies have shown marginal or no clinical benefit[18-22] and higher surgical costs[19,23].
At present, although there is no consensus regarding the superiority of the laparoscopic approach over the conventional technique, there is trend towards greater utilization of laparoscopic appendectomy[24,25].
In the present study, we aim to compare the laparoscopic approach and the conventional technique in the treatment of acute appendicitis, using prospectively collected data from patients subjected to appendectomy between January 2006 and January 2008.
Data was collected prospectively on patients with acute appendicitis who underwent open or laparoscopic appendectomy from January 2006 to January 2008 in the surgery department of the University Teaching Hospital at Patras. The clinical data base contained information such as patient characteristics, postoperative course, length of hospital stay, postoperative morbidity and mortality, 30-d readmission and hospital charges.
All human studies were performed according to the principles of the declaration of Helsinki. The study was approved by the research and ethics committee at the University Hospital of Patras.
The diagnosis of appendicitis was made in the emergency department and was based on the presence of right lower quadrant pain, nausea or vomiting, and abdominal guarding on physical examination. In patients where a clinical diagnosis could not be established, imaging studies such as abdominal ultrasound or CT were performed. Exclusion criteria included pregnancy, homodynamic instability, chronic medical or psychiatric illness, cirrhosis, coagulation disorders, previous laparotomy for small bowel obstruction, and ascites. In order to increase the homogeneity of the group, a total of 37 patients (11.2%), who underwent elective interval appendectomy or had incidental appendectomy in the presence of other intra-abdominal pathology were excluded from the study. The decision about the type of the operation was made according to the preference and experience of the surgical team on duty.
Prior to the surgery, all the patients received a standard regimen of intravenous antibiotics (1.5 g of Cefuroxime and 500 mg of Metronidazole). Provided purulent appendicitis was not observed at surgery, two additional doses were given. In patients with complicated appendicitis, antibiotics were not discontinued but were modified according to the culture results.
Open appendectomy was typically performed through a 3 cm McBurney muscle splitting incision in the right lower quadrant. Following appendectomy the stump was double ligated with an absorbable suture. In the presence of complicated appendicitis the abdomen was irrigated with warm saline solution and the skin incision was closed loosely.
In the laparoscopic group, pneumoperitoneum was produced by continuous pressure of 10-12 mmHg of carbon dioxide via a Verres canula, positioned in the left subcostal area. Following gas insufflation, a 12 mm trocar for the 30 degree angled laparoscope was placed in the left periumbilical area and two additional trocars, a 12 mm trocar in the suprapubic area to accommodate the stapling device and to facilitate specimen extraction, and a third 5 mm trocar in the left lower abdominal quadrant were introduced under direct visualization. The patient was placed in a Trendelenburg position, with a slight rotation to the left. The abdominal cavity was thoroughly inspected in order to exclude other intra-abdominal or pelvic pathology. After the mesoappendix was divided with bipolar forceps, the base of the appendix was secured with two ligating loops, followed by dissection distal to the second loop using a curved dissector. In patients with severe inflammation, a stapling device was used for the dissection of the appendix. The specimen was placed in an endobag and was extracted through the suprapubic trocar. All specimens were sent for histopathology.
The parameters examined in this study included patient’s characteristics (age, sex), operation time (from skin incision to wound closure), conversion to open procedure, and intraoperative findings (normal, gangrenous or perforated appendix). Furthermore, during the postoperative follow up, pain was assessed both by the patient’s requirements for analgesia, and with a visual analog score. The length of hospital stay, complications and cost were also added to the plot. The discharge criteria were met once the patients’ were afebrile, with audible bowel sounds and were able to tolerate a liquid diet.
Statistical analysis was performed using SPSS statistical software, version 12.0 (SPSS Inc., Chicagi, IL). The data were expressed as mean and standard deviation. Parameters such as length of hospitalization, mortality and morbidity, and hospital cost are given as mean variable. Bivariate analyses were performed to determine the differences between laparoscopic versus open appendectomy in patient characteristics, length of hospital stay and costs using independent sample t tests for continuous variables and chi-square analysis for categorical variables. A P value of less than 0.05 was considered statistically significant.
A total of 293 patients with acute appendicitis were admitted during the study period. 165 patients were subjected to open appendectomy and 128 patients to laparoscopic appendectomy. The patient characteristics are shown in Table 1. There were no significant differences with respect to gender, age, white blood cell count at presentation, and associated co-morbidities.
Out of the total 165 open procedures, 118 (71.5%) were performed for uncomplicated appendicitis and 47 (28.5%) for complicated disease including appendiceal perforation with local or widespread peritonitis.
In the laparoscopic group, 90 (70.3%) procedures involved uncomplicated disease and 38 (29.7%) complicated appendicitis (Table 2). Additionally, in 16 (9.6%) open and 8 (6.2%) laparoscopic procedures, no pathology was observed in the appendix and other intra-abdominal structures (Table 2).
The actual operating room time was similar between the two groups (47 ± 19.7 min in the open group vs 44.3 ± 24 min in the laparoscopic group; P = 0.31, Table 2). Conversion to an open procedure was required in two patients (1.5%) with extensive cecal adhesions secondary to severe inflammation rendering appendiceal mobilization and visualization difficult and dangerous.
There was no mortality in either group and the overall morbidity was not significantly different (10.3% in the open group vs 7.8% in the laparoscopic group; P = 0.43, Table 3).
In patients with uncomplicated disease, the morbidity rates were low (0.8% in open appendectomy and 1.1% in laparoscopic appendectomy; P = 0.5, Table 3). One patient subjected to open appendectomy developed wound infection. The culture of pus revealed E. coli and the patient was successfully treated with antibiotics and wound debridement. Similarly, in one patient in the laparoscopic group, intestinal injury occurred during insertion of the visiport. The lesion was recognized intraoperatively and was successfully managed with endoscopic sutures. The end result was favorable and no further manipulations were required.
In contrast to uncomplicated disease, patients with complicated appendicitis were prone to postoperative complications (34% after open appendectomy and 23.7% after laparoscopic approach; P = 0.12, Table 3). Postoperative bowel obstruction was observed in patients with complicated disease in both study groups (10.6% after conventional appendectomy and 7.8% after laparoscopic appendectomy; P = 0.37, Table 3). In addition, complicated appendicitis was associated postoperatively with respiratory infection in 4 patients subjected to open appendectomy, and 2 patients treated laparoscopically (P = 0.18, Table 3).
Infectious complications were seen in both study groups in patients with complicated disease. Open appendectomy was associated with a significantly higher incidence of wound infection compared with the laparoscopic group (12.8% vs 5.3%; P = 0.03, Table 3).
On the other hand, the incidence of intra-abdominal abscess formation was higher in patients with severe peritonitis who were treated laparoscopically (5.3% vs 2.1%; P = 0.002, Table 3). All patients who developed intra-abdominal abscess were treated successfully with antibiotics and CT-guided drainage of the collection, and had an uneventful recovery.
Bowel movements in the first postoperative day were observed in 92% patients subjected to laparoscopic appendectomy and 67% in the open group (P < 0.001). As a result, 78% patients in the laparoscopic group and 51% in the open group were able to tolerate a liquid diet within the first 24 postoperative hours (P < 0.001). The mean postoperative hospital stay was 2.2 d (range, 1-17 d) after laparoscopic appendectomy and 3.1 d (range, 1-18 d) after open appendectomy (P = 0.04).
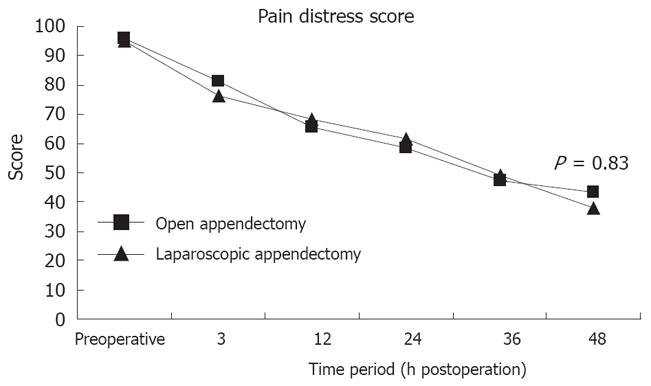
Visual analogue pain scores were similar in the two groups for the first two postoperative days (Figure 1). There was a significant decline after the first 3 postoperative hours to 48 h in both groups. There was no difference between open and laparoscopic groups with respect to either overall pain level (P = 0.93) or degree of pain remission (P = 0.82). Eventually, the need for analgesic medication usage for the control of postoperative pain was similar in the two groups.
Finally, the operative costs were higher by 370 € in the laparoscopic group. In the present study, the costs were calculated based on the most cost effective materials used such as laparoscopic equipment, versatile laparoscopic instruments, endoloops and collection bags. Hospital charges regarding anesthesia were not added to the plot since there was no difference in the operative times.
Acute appendicitis is the most common intra-abdominal condition requiring emergency surgery[26]. Although more than 20 years have elapsed since the introduction of laparoscopic appendectomy, there is no consensus on its advantages and disadvantages compared to the conventional technique.
Recent studies have shown significant advantages of laparoscopic appendectomy with respect to the length of hospital stay, postoperative pain and infectious complications[5,8,12,14,18]. These findings have been challenged by other authors who observed no significant difference in the outcome between the two procedures, and moreover noted higher costs with laparoscopic appendec-tomy[3,17,19,25,27].
Bearing in mind that laparoscopic appendectomy, unlike other laparoscopic procedures, has not been found superior to open surgery for acute appendicitis, we designed the present study to determine any possible benefits of the laparoscopic approach.
Operation time remains a topic of much debate among experts. Preliminary studies[28-30] have shown significantly longer operative times for laparoscopic appendectomy. The inexperience of the surgeons with the new technique may contribute to the longer duration of the operation in the early studies. However, recent studies[16-18] have supported the initial findings. Because in these studies, most of the operations were performed by residents, the longer operation times can be attributed to the learning curve. By contrast, in the present study, the operation times were nearly similar in the two techniques, and the learning curve effect was minimal as the surgeons performing the procedures were highly experienced with a wide spectrum of laparoscopic procedures, including laparoscopic bariatric surgery and laparoscopic colectomy. This experience is reflected in our study by the relatively narrow range of operative times in the laparoscopic group (44.3 ± 24).
Previous studies have given conflicting results with respect to the length of hospital stay after laparoscopic appendectomy. Guller et al[12] in a population- based analysis using a national administrative data base showed that laparoscopic appendectomy is associated with significantly shorter hospital stay. These findings were supported by the Cochrane Collaboration large scale meta-analysis[24]. In agreement with these studies, we found that hospital stay was significantly shorter in patients subjected to laparoscopic appendectomy (P = 0.004). In the present study, bowel movements were observed significantly earlier in patients managed laparoscopically, leading to earlier feeding and discharge from hospital.
In the present study, pain was assessed both subjectively via a visual analogue scale and objectively by the tabulation of analgesic use. Although some studies have reported less pain in the first 48 h after laparoscopic appendectomy[20,21,24,25,31], in our series there was no difference between the two groups with respect to either the visual analogue scores or the use of analgesics. Our study suffered from the drawback that it was not blinded. As a result, the perception of pain may have been influenced by the patient’s enthusiasm for a novel technique.
There was no mortality in our study. This is consistent with the majority of previous publications. It has been reported that the mortality rate is 0.05% and 0.3% in laparoscopic and open appendectomy respectively[12]. The low mortality rates indicate that appendectomy, especially in the absence of complicated disease, is a safe procedure regardless of the technique used.
In the present study, the overall complication rates were 10.6% and 8.1% for open and laparoscopic appendectomy respectively. These results are in agreement with previous reports, which vary from 5.7% to 25.8% for open appendectomy and 3% to 19% for laparoscopic appendectomy[13-15,20-23].
Complicated appendicitis was initially considered as a contraindication to laparoscopic appendectomy[32,33]. However, recent studies have shown that laparoscopic approach in complicated disease is feasible and may even be superior to the conventional approach[6,7,10].
In our series, 28.5% patients in the open group and 29.7% in the laparoscopic group had complicated disease. These patients are considered to be at increased risk of postoperative infections such as wound infection and intra-abdominal abscess formation[34,35]. According to the Cochrane systemic review of the literature[24], wound infection is about one-half after laparoscopic appendectomy, while intra-abdominal abscess formation is 3 times higher after laparoscopic appendectomy.
In the present study, the rate of wound infection in patients with complicated disease was significantly lower after laparoscopic appendectomy (5.3% vs 12.8%, P = 0.03). Placement of the detached appendix into an endobag before its removal from the abdominal cavity reduces contact with the fascial surfaces and minimizes contamination.
Intra-abdominal abscess formation was more common after laparoscopic appendectomy in complicated disease (5.3% vs 2.1%, P = 0.002). It has been suggested that carbon dioxide insufflation may promote mechanical spread of bacteria in the peritoneal cavity, especially in cases of ruptured appendix[21,36-38]. In order to decrease the bacterial load and hence the risk of abscess formation, we advocate extensive irrigation of the abdominal cavity. However, in our practice, we observed that meticulous irrigation was unnecessary and even more dangerous as it leads to contamination of the entire abdominal cavity, which is difficult to aspirate latter. That was the case in two patients with severe peritonitis where intra-abdominal abscess formation occurred. Ever since we have changed our practice to simple suctioning of the infected area, we have not observed any postoperative abscess formation, even in patients with severe peritonitis.
The higher cost of laparoscopic appendectomy compared to the conventional technique is considered as an obstacle to its greater use. However, hospital charges for laparoscopic appendectomy have reduced dramatically over the past several years[39]. Surgical expertise and the abundance of laparoscopic equipment have significantly reduced the economical mismatch in favor of the conventional technique. In addition, Moore and coworkers, using a decision analysis model, have demonstrated an economic benefit of laparoscopic appendectomy from a social perspective, since shorter hospital stay and earlier return to daily activities is very important, especially for patients who are young and lead a productive life[40].
In the present study, the operative costs for laparoscopic appendectomy were only 370 € higher. The greater cost of laparoscopic appendectomy observed in various studies[3,14,25] can be attributed to the use of disposable laparoscopic instruments and the longer operative time. In our series, we were able to minimize the operative costs, mainly by employing reusable laparoscopic instruments.
Although there is no consensus with regard to the advantages of the laparoscopic approach compared to the conventional technique, the use of laparoscopic appendectomy has increased significantly in the last several years. In the present study, we were able to demonstrate the superiority of the laparoscopic approach in terms of hospital stay and wound infection, with only marginally higher hospital costs. Although the incidence of intra-abdominal abscess formation was higher after laparoscopic appendectomy, all complications occurred early in our practice. Greater experience and improvements in our technique has made it possible to eradicate this catastrophic complication.
Provided that surgical experience and equipment are available, laparoscopic appendectomy is safe and equally efficient compared to the conventional technique. However, as long as there is no consensus to the best approach for appendicitis, the choice of the procedure will be based on the preference of the surgeons and patients.
Laparoscopic surgery has been available for a long time. Today, even the most complicated procedures can be performed laparoscopically. However, laparoscopic appendectomy, a relatively easy procedure, has not gained wide acceptance among surgeons, and the conventional technique remains the procedure of choice in many centres worldwide.
Intra-abdominal abscess formation is the most catastrophic complication of laparoscopic appendectomy. By simple suctioning of the infected area, rather than using widespread irrigation we were able to decrease the incidence of postoperative abscess formation.
In the present study, we were able to demonstrate that laparoscopic appendectomy is superior to the conventional technique in terms of hospital stay and wound infection. Additionally, in expert hands, even the most serious complications such as an intra-abdominal abscess formation can be minimized. Furthermore, in the present study, we were able to decrease medical costs by employing reusable laparoscopic equipment.
The present study has shown that laparoscopic surgery should be considered in every patient with appendicitis.
The authors demonstrated a prospective study of laparoscopic versus open appendectomy and concluded “Provided that surgical experience and equipment are available, laparoscopic appendectomy is safe and equally efficient alternative to conventional technique.” This present study is an interesting and novel.
Peer reviewer: Yasuji Arase, MD, Department of Gastro-enterology, Toranomon Hospital, 2-2-2Toranomonminato-ku, Tokyo 105-8470, Japan
S- Editor Zhong XY L- Editor Anand BS E- Editor Ma WH
| 1. | McBurney C. IV. The Incision Made in the Abdominal Wall in Cases of Appendicitis, with a Description of a New Method of Operating. Ann Surg. 1894;20:38-43. |
| 3. | Kurtz RJ, Heimann TM. Comparison of open and laparoscopic treatment of acute appendicitis. Am J Surg. 2001;182:211-214. |
| 4. | Wullstein C, Barkhausen S, Gross E. Results of laparoscopic vs. conventional appendectomy in complicated appendicitis. Dis Colon Rectum. 2001;44:1700-1705. |
| 5. | Fogli L, Brulatti M, Boschi S, Di Domenico M, Papa V, Patrizi P, Capizzi FD. Laparoscopic appendectomy for acute and recurrent appendicitis: retrospective analysis of a single-group 5-year experience. J Laparoendosc Adv Surg Tech A. 2002;12:107-110. |
| 6. | Lin HF, Wu JM, Tseng LM, Chen KH, Huang SH, Lai IR. Laparoscopic versus open appendectomy for perforated appendicitis. J Gastrointest Surg. 2006;10:906-910. |
| 7. | Cueto J, D’Allemagne B, Vazquez-Frias JA, Gomez S, Delgado F, Trullenque L, Fajardo R, Valencia S, Poggi L, Balli J. Morbidity of laparoscopic surgery for complicated appendicitis: an international study. Surg Endosc. 2006;20:717-720. |
| 8. | Towfigh S, Chen F, Mason R, Katkhouda N, Chan L, Berne T. Laparoscopic appendectomy significantly reduces length of stay for perforated appendicitis. Surg Endosc. 2006;20:495-499. |
| 9. | Roviaro GC, Vergani C, Varoli F, Francese M, Caminiti R, Maciocco M. Videolaparoscopic appendectomy: the current outlook. Surg Endosc. 2006;20:1526-1530. |
| 10. | Ball CG, Kortbeek JB, Kirkpatrick AW, Mitchell P. Laparoscopic appendectomy for complicated appendicitis: an evaluation of postoperative factors. Surg Endosc. 2004;18:969-973. |
| 11. | Nguyen NT, Zainabadi K, Mavandadi S, Paya M, Stevens CM, Root J, Wilson SE. Trends in utilization and outcomes of laparoscopic versus open appendectomy. Am J Surg. 2004;188:813-820. |
| 12. | Guller U, Hervey S, Purves H, Muhlbaier LH, Peterson ED, Eubanks S, Pietrobon R. Laparoscopic versus open appendectomy: outcomes comparison based on a large administrative database. Ann Surg. 2004;239:43-52. |
| 13. | Ortega AE, Hunter JG, Peters JH, Swanstrom LL, Schirmer B. A prospective, randomized comparison of laparoscopic appendectomy with open appendectomy. Laparoscopic Appendectomy Study Group. Am J Surg. 1995;169:208-212; discussion 212-213. |
| 14. | Milewczyk M, Michalik M, Ciesielski M. A prospective, randomized, unicenter study comparing laparoscopic and open treatments of acute appendicitis. Surg Endosc. 2003;17:1023-1028. |
| 15. | Martin LC, Puente I, Sosa JL, Bassin A, Breslaw R, McKenney MG, Ginzburg E, Sleeman D. Open versus laparoscopic appendectomy. A prospective randomized comparison. Ann Surg. 1995;222:256-261; discussion 261-262. |
| 16. | Bresciani C, Perez RO, Habr-Gama A, Jacob CE, Ozaki A, Batagello C, Proscurshim I, Gama-Rodrigues J. Laparoscopic versus standard appendectomy outcomes and cost comparisons in the private sector. J Gastrointest Surg. 2005;9:1174-1180; discussion 1180-1181. |
| 17. | Ignacio RC, Burke R, Spencer D, Bissell C, Dorsainvil C, Lucha PA. Laparoscopic versus open appendectomy: what is the real difference? Results of a prospective randomized double-blinded trial. Surg Endosc. 2004;18:334-337. |
| 18. | Olmi S, Magnone S, Bertolini A, Croce E. Laparoscopic versus open appendectomy in acute appendicitis: a randomized prospective study. Surg Endosc. 2005;19:1193-1195. |
| 19. | Katkhouda N, Mason RJ, Towfigh S, Gevorgyan A, Essani R. Laparoscopic versus open appendectomy: a prospective randomized double-blind study. Ann Surg. 2005;242:439-448; discussion 448-450. |
| 20. | Golub R, Siddiqui F, Pohl D. Laparoscopic versus open appendectomy: a metaanalysis. J Am Coll Surg. 1998;186:545-553. |
| 21. | Chung RS, Rowland DY, Li P, Diaz J. A meta-analysis of randomized controlled trials of laparoscopic versus conventional appendectomy. Am J Surg. 1999;177:250-256. |
| 22. | Temple LK, Litwin DE, McLeod RS. A meta-analysis of laparoscopic versus open appendectomy in patients suspected of having acute appendicitis. Can J Surg. 1999;42:377-383. |
| 23. | Garbutt JM, Soper NJ, Shannon WD, Botero A, Littenberg B. Meta-analysis of randomized controlled trials comparing laparoscopic and open appendectomy. Surg Laparosc Endosc. 1999;9:17-26. |
| 24. | Sauerland S, Lefering R, Neugebauer EA. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2004;9:CD001546. |
| 25. | Merhoff AM, Merhoff GC, Franklin ME. Laparoscopic versus open appendectomy. Am J Surg. 2000;179:375-378. |
| 26. | Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132:910-925. |
| 27. | Moore DE, Speroff T, Grogan E, Poulose B, Holzman MD. Cost perspectives of laparoscopic and open appendectomy. Surg Endosc. 2005;19:374-378. |
| 28. | Apelgren KN, Molnar RG, Kisala JM. Laparoscopic is not better than open appendectomy. Am Surg. 1995;61:240-243. |
| 29. | Hart R, Rajgopal C, Plewes A, Sweeney J, Davies W, Gray D, Taylor B. Laparoscopic versus open appendectomy: a prospective randomized trial of 81 patients. Can J Surg. 1996;39:457-462. |
| 30. | Mutter D, Vix M, Bui A, Evrard S, Tassetti V, Breton JF, Marescaux J. Laparoscopy not recommended for routine appendectomy in men: results of a prospective randomized study. Surgery. 1996;120:71-74. |
| 31. | Sauerland S, Lefering R, Holthausen U, Neugebauer EA. Laparoscopic vs conventional appendectomy--a meta-analysis of randomised controlled trials. Langenbecks Arch Surg. 1998;383:289-295. |
| 32. | Frazee RC, Bohannon WT. Laparoscopic appendectomy for complicated appendicitis. Arch Surg. 1996;131:509-511; discussion 511-513. |
| 33. | Bonanni F, Reed J 3rd, Hartzell G, Trostle D, Boorse R, Gittleman M, Cole A. Laparoscopic versus conventional appendectomy. J Am Coll Surg. 1994;179:273-278. |
| 34. | Andersson RE, Hugander A, Thulin AJ. Diagnostic accuracy and perforation rate in appendicitis: association with age and sex of the patient and with appendicectomy rate. Eur J Surg. 1992;158:37-41. |
| 35. | Krukowski ZH, Irwin ST, Denholm S, Matheson NA. Preventing wound infection after appendicectomy: a review. Br J Surg. 1988;75:1023-1033. |
| 36. | Evasovich MR, Clark TC, Horattas MC, Holda S, Treen L. Does pneumoperitoneum during laparoscopy increase bacterial translocation? Surg Endosc. 1996;10:1176-1179. |
| 37. | Gurtner GC, Robertson CS, Chung SC, Ling TK, Ip SM, Li AK. Effect of carbon dioxide pneumoperitoneum on bacteraemia and endotoxaemia in an animal model of peritonitis. Br J Surg. 1995;82:844-848. |
| 38. | Jacobi CA, Ordemann J, Bohm B, Zieren HU, Volk HD, Lorenz W, Halle E, Muller JM. Does laparoscopy increase bacteremia and endotoxemia in a peritonitis model? Surg Endosc. 1997;11:235-238. |
| 39. | Glasgow RE, Adamson KA, Mulvihill SJ. The benefits of a dedicated minimally invasive surgery program to academic general surgery practice. J Gastrointest Surg. 2004;8:869-873; discussion 873-875. |
| 40. | Moore DE, Speroff T, Grogan E, Poulose B, Holzman MD. Cost perspectives of laparoscopic and open appendectomy. Surg Endosc. 2005;19:374-378. |