Published online Aug 14, 2008. doi: 10.3748/wjg.14.4826
Revised: July 21, 2008
Accepted: July 28, 2008
Published online: August 14, 2008
Major injuries of the pancreas may result in considerable morbidity and mortality when associated with vascular and visceral injuries. In such cases, a right diagnosis and a prompt surgical intervention are necessary to give a chance to the patient. We herein describe a case of blunt abdominal trauma in a 29-year-old man whose pancreatic rupture was associated with hepatic artery, splenic vein and extrahepatic bile duct damage. Immediate surgery was performed after computer tomography (CT), the haemorrhagic lesions dictate the emergency transfer to the operating room. Spleno-pancreatic resection was done with reconstruction of the hepatic artery, ligation of the splenic vein and a Roux-en-Y bilio-jejunal diversion. The early post-operative course was complicated by stenosis of the arterial reconstruction, which was treated by endovascular angioplasty followed by percutaneous drainage of symptomatic pseudocyst, rest and antibiotics. Finally, the patient was discharged and was alive without clinical problems at the time when we wrote this case report. The present case underlines the clinical relevance of vascular and visceral injuries associated with pancreatic trauma and the problems arising in the diagnostic evaluation and the surgical strategy of complex multiple visceral and vascular lesions in blunt abdominal trauma.
- Citation: Baiocchi GL, Tiberio GA, Gheza F, Gardani M, Cantù M, Portolani N, Giulini SM. Pancreatic transection from blunt trauma associated with vascular and biliary lesions: A case report. World J Gastroenterol 2008; 14(30): 4826-4829
- URL: https://www.wjgnet.com/1007-9327/full/v14/i30/4826.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.4826
Isolated pancreatic injury occurs in less than 5% of major blunt abdominal traumas due to its retroperitoneal location[1]. In the majority of patients, pancreatic trauma is associated with major thoraco-abdominal lesions, which are the main factors influencing its clinical evolution in the acute phase. On the contrary, in the subsequent period, its mortality is related to septic complications and subsequent pancreatic or biliary disruption.
Few retrospective series of blunt pancreatic trauma, including more than 30 patients, have been published[2-6]. Its postoperative morbidity ranges from 42%[3] to 62%[2], and its mortality is as high as 18.1%[6]. Age, severity of injury, amylasis level, abdominal pain, injury severity score (ISS), presence of associated lesions, duration of shock, unrecognised diagnosis, delay in treatment and postoperative sepsis are the factors that significantly influence its outcome. Cases of multiple visceral and vascular lesions in the pancreatic area are not reported in the literature, presumably because the gravity of such situations does not allow the patient to survive.
We herein describe a case of blunt abdominal trauma causing pancreatic rupture associated with multiple arterial, venous, and biliary lesions, and discussed the diagnostic and therapeutic approach to such a rare case of multiple severe traumatic lesions.
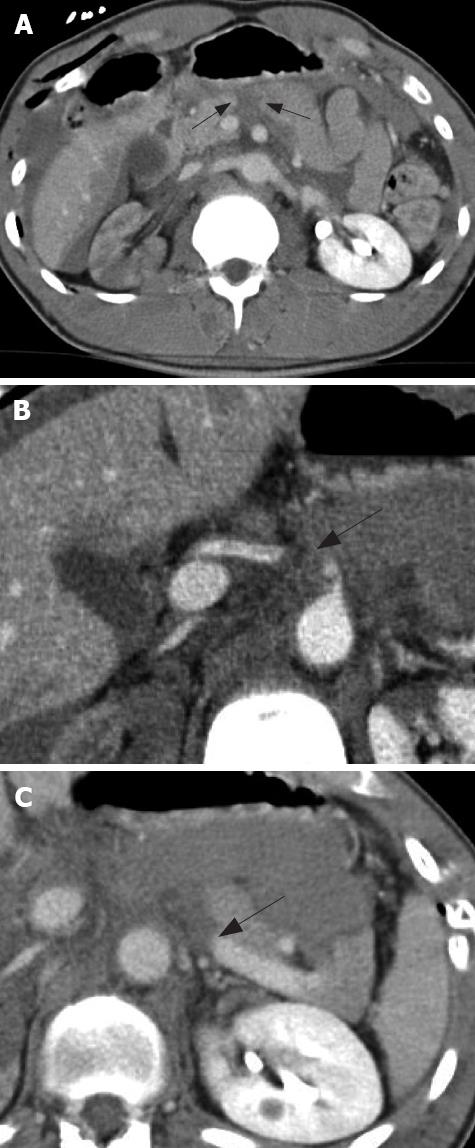
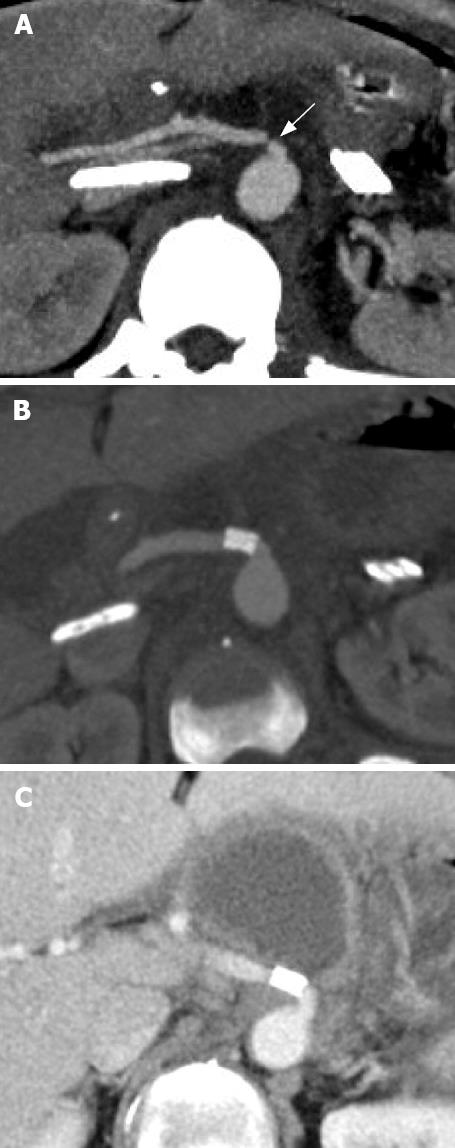
A 29-year-old male sustained a blunt abdominal trauma crushed by a carriage at work. At first observation he was in stable hemodynamic conditions, but complained of abdominal and back pain. Initial radiologic evaluation (chest and pelvis X-ray, and abdominal US) detected a right pneumothorax, bilateral rib fractures and a small amount of free blood in the abdominal cavity. Thoraco-abdominal computer tomography (CT) scan confirmed the presence of hemoperitoneum and revealed hepatic and spleen contusions, pancreatic transection at the junction between head and body (Figure 1A), thrombosis of the hepatic artery at its origin from the celiac trunk (Figure 1B), and thrombosis of the splenic vein (Figure 1C), as well as contusion of the right renal artery with no renal perfusion and fracture of D12 and L1. ISS was 34[7]. An immediate laparotomy was performed with free blood and bile found in the peritoneal cavity. After the gastro-colic ligament was cut open, the pancreatic transaction and contusion of the common hepatic artery at its origin were confirmed with their continuity maintained by adventitia, while intima and media layers were partitioned with consequent occlusion of the artery. Splenic vein was completely transected at its confluence with the mesenterico-portal axis. Removal of the retropancreatic hematoma induced bleeding, stopped at first by digital compression and then by clamping the splenic vein and tangentially suturing the spleno-portal confluence. A complete interruption of the choledocus was demonstrated, his distal stump was ligated and the proximal one was clamped. The intra operative Doppler evaluation demonstrated that the right kidney was perfused with normal flow in the renal artery. The arterial blood supply to the liver was maintained by the inverted flow into the gastro-duodenal artery, but no pulsation could be appreciated at porta hepatis. Thus, a distal spleno-pancreatectomy was performed. After a short resection of the dissected tract, the common hepatic artery was reconstructed by end-to-end direct anastomosis to the celiac artery. Cholecystectomy and hepatico-jejunal anastomosis completed the operation. In the first postoperative period, ALT abd AST increased up to 154 U/L and 121 U/L, respectively. Postoperative CT scan showed stenosis of the celiac-hepatic anastomosis (Figure 2A), requiring operative angiography with stenting of the hepatic origin. A further CT control demonstrated the good results of the procedure (Figure 2B). Prophylactic octreotide acetate, 300 mg/d, was given after the intervention, as previously described[8], and serum lipases were in the normal range. The patient was finally discharged on day 27 after operation.
Three months later, the patient complained of abdominal pain and dyspepsia, fever and leucocytosis. Abdominal US and CT scan showed a pancreatic pseudocyst (8 cm in diameter) in the epigastric region, between the residual pancreas, the posterior part of the stomach and the hepatic artery (Figure 2C), requiring percutaneous drainage, rest and antibiotic therapy. A significant reduction in size of the pseudocyst was achieved and the patient was discharged. At the 3-year control, the patient had normal quality of life, laboratory tests and abdominal US.
Blunt pancreatic trauma is frequently combined with other organ injuries, which may cause early death of the patient[2-6]. The case reported in the present paper is of particular significance for the presence of multiple severe lesions involving vital structures in the pancreatic region, as a consequence of a violent trauma focused in this area, substantially sparing the rest of the patient’s body. In our knowledge, this is the first reported case of contemporary traumatic disruption of the pancreatic neck, choledocus, spleno-portal confluence and common hepatic artery, probably because a patient so severely damaged is unlike to survive to the required diagnostic and therapeutic time. In a paper analysing over 300 cases of traumatic vascular injury, the overall mortality was 54%, increasing up to 73% when 3 vessels were involved and 100% when 4 vessels were involved[9]. Patients affected by associated vascular and pancreatic injuries were even more rarely described (only 3 out of 101 cases analysed by Bradley and Coll)[6].
The good outcome of the presented case is in our opinion due to the spontaneous partial haemostasis, but also to the prompt intervention, whose indication was dictated by the contrast-enhanced CT scan. The limits of this examination in defining the presence and gravity of pancreas trauma are well known. It was reported that the sensitivity of pancreatic rupture is 42.9%[6,10,11] and its low accuracy is particularly critical in defining the damage of the main pancreatic duct, the single most important factor both for surgical indication and choice of the best surgical strategy[12-14]. In our case, CT allowed to exclude thoracic lesions and to focus on the pancreatic region, demonstrating the pancreatic body fracture and the presence of associated vascular damage. At the same time, choledocus fracture was not demonstrated, a wrong diagnosis of right renal artery thrombosis was suggested and also the hepatic artery and the splenic vein thrombosis were not clearly evaluated. This is in agreement with the literature, which reported that the mean injury grade resulting from CT is significantly lower than that resulting from surgical exploration[11].
To avoid this limit of CT, endoscopic retrograde cholangio-pancreatography has been proposed to allow a more accurate identification of the biliary and Wirsung duct discontinuity, the superiority of which over CT scan in the evaluation of such structures is well documented[5]. However, in emergency situations, endoscopic examination is rarely considered since it requires a significant loss of time and is uselessly invasive, particularly if a surgical intervention has already proved to be necessary. In the reported case, the demonstrated vascular lesions dictated the necessity of immediate laparotomy, due to either the haemorrhagic risk or the ischemic damage to the liver. Thus, CT scan, even though it may be considered not completely accurate, is very useful for the correct management of this case.
These considerations shift the problem of complete diagnostic evaluation to the operating table, namely surgical exploration must be meticulous and systematic to demonstrate, define and treat the lesions associated with a pancreatic rupture. Undervaluation of the associated lesions is the most important negative prognostic factor for pancreatic trauma. By sectioning the gastro-colic ligament and the lesser omentum and completely mobilizing the right colon with the hepatic flexure and the right part of the transverse colon, or by performing a wide Kocher manoeuvre, a complete control of the structures potentially involved in pancreatic trauma is obtained. Surgical exploration can be completed by intraoperative instrumental evaluations such as cholangiography, endoscopy and doppler ultrasound, especially in cases in which preoperative imaging has been lacking or not exhaustive. In the presented case, the only employed intraoperative diagnostic tool was Doppler spectral analysis of the hepatic and portal flow. Evident lesions of the choledocus and pancreatic duct could be observed at inspection and irrigation. A vascular lesion may be really difficult to ascertain by simple exploration. However, after a complete transection, the haemorrhage can spontaneously stop and a complete thrombosis may be undiagnosed by a simple palpation. Intraoperative Doppler scan finally allows evaluation of the flow dynamics of suspected vascular lesions. In our case, it enabled us to demonstrate the preservation of a normal mesenterico-portal flow, the absence of residual stenosis of the mesenterico-portal axis after its suture and to document the collateral arterial flow at the hepatic hilum maintained by the gastroduodenal artery in presence of a contusion with short dissection occluding the common hepatic artery. In case of a post-traumatic hepatic artery thrombosis, in the context of a complex trauma, reconstruction of this artery can be considered not necessary if a compensating inverted gastroduodenal artery flow is demonstrated. Reconstruction of a damaged hepatic artery is difficult, time-consuming and not rarely ineffective. However, when a bilio-digestive anastomosis has to be performed, a normal arterial flow is needed for the optimal perfusion of the biliary anastomotic stump. Intraoperative evaluation of the arterial collateral liver vascularisation may be misleading, lacking of quantitative determination. For these reasons, we did prefer to reconstruct the celiac-hepatic artery continuity by an end-to-end direct anastomosis, that later has proved to be technically imperfect and to require a post-operative percutaneous angioplasty with stenting. Our effort to maintain the continuity of the hepatic artery was justified by the transitory post-operative rise of hepatic enzymes, which returned to the normal range after stenting of the anastomosis. Moreover, a case of unrecognised hepatic artery dissection, having as a consequence a fatal fulminate hepatic failure, was recently reported[15]. Alternative techniques of revascularization by means of a prosthetic conduit should be avoided if possible, because septic complications are frequent in the postoperative course.
With regard to the biliary reconstruction, hepatico-jejunal anastomosis is preferable to a direct end-to-end reconstruction, as it allows a wide resection of the contused choledocus and anstomosis on a healthy tissue without tension[16].
For the treatment of pancreatic transection, a number of techniques have been proposed, as an alternative to the distal pancreatectomy, accounting for 30% of the operations for pancreatic injuries[17]. With the aim to preserve endocrine pancreatic function, the distal pancreas can be anatomised to a Roux-en-Y jejunal loop, or to the stomach[18]. In presence of multiple lesions associated with the pancreatic injury, the strategy should be guided by the principle of obtaining repair of the lesions by a more simple and safe technical solution, reducing the risk of postoperative complications. Distal pancreatectomy with splenectomy, or whenever possible with splenic preservation, has a complication rate of 22.2%, lower than that of distal pancreas preserving procedures[2]. Moreover, postoperative exocrine and endocrine insufficiency is quite rare when the cephalic portion of the gland is preserved. The risk of developing proximal pancreatic stump fistula, with eventual pseudocyst formation, is independent of the treatment of the distal portion of the pancreas.
Our case demonstrates that if the haemorrhage can be spontaneously and temporarily controlled, giving to the surgeon the time strictly necessary to obtain the basilar diagnostic indications and to perform laparotomy, a systematic exploration and a surgical strategy inspired by the principle of doing all but just what is necessary to save the patient, allow to obtain both immediate survival and long-term good quality of life.
Peer reviewer: Michael Steer, Professor, Department of Surgery, Tufts-Nemc, 860 Washington St, Boston Ma 02111, United States
S- Editor Li DL L- Editor Wang XL E- Editor Yin DH
| 1. | Craig MH, Talton DS, Hauser CJ, Poole GV. Pancreatic injuries from blunt trauma. Am Surg. 1995;61:125-128. |
| 2. | Lin BC, Chen RJ, Fang JF, Hsu YP, Kao YC, Kao JL. Management of blunt major pancreatic injury. J Trauma. 2004;56:774-778. |
| 3. | Akhrass R, Yaffe MB, Brandt CP, Reigle M, Fallon WF Jr, Malangoni MA. Pancreatic trauma: a ten-year multi-institutional experience. Am Surg. 1997;63:598-604. |
| 4. | Farrell RJ, Krige JE, Bornman PC, Knottenbelt JD, Terblanche J. Operative strategies in pancreatic trauma. Br J Surg. 1996;83:934-937. |
| 5. | Wind P, Tiret E, Cunningham C, Frileux P, Cugnenc PH, Parc R. Contribution of endoscopic retrograde pancreatography in management of complications following distal pancreatic trauma. Am Surg. 1999;65:777-783. |
| 6. | Bradley EL 3rd, Young PR Jr, Chang MC, Allen JE, Baker CC, Meredith W, Reed L, Thomason M. Diagnosis and initial management of blunt pancreatic trauma: guidelines from a multiinstitutional review. Ann Surg. 1998;227:861-869. |
| 7. | Baker SP, O'Neill B, Haddon W Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187-196. |
| 8. | Amirata E, Livingston DH, Elcavage J. Octreotide acetate decreases pancreatic complications after pancreatic trauma. Am J Surg. 1994;168:345-347. |
| 9. | Asensio JA, Chahwan S, Hanpeter D, Demetriades D, Forno W, Gambaro E, Murray J, Velmahos G, Marengo J, Shoemaker WC. Operative management and outcome of 302 abdominal vascular injuries. Am J Surg. 2000;180:528-533; discussion 533-534. |
| 10. | Akhrass R, Kim K, Brandt C. Computed tomography: an unreliable indicator of pancreatic trauma. Am Surg. 1996;62:647-651. |
| 11. | Udekwu PO, Gurkin B, Oller DW. The use of computed tomography in blunt abdominal injuries. Am Surg. 1996;62:56-59. |
| 13. | Takishima T, Sugimoto K, Hirata M, Asari Y, Ohwada T, Kakita A. Serum amylase level on admission in the diagnosis of blunt injury to the pancreas: its significance and limitations. Ann Surg. 1997;226:70-76. |
| 14. | Peitzman AB, Makaroun MS, Slasky BS, Ritter P. Prospective study of computed tomography in initial management of blunt abdominal trauma. J Trauma. 1986;26:585-592. |
| 15. | Kirchhoff C, Stegmaier J, Krotz M, Muetzel Rauch E, Mutschler W, Kanz KG, Heindl B. Celiac dissection after blunt abdominal trauma complicated by acute hepatic failure: case report and review of literature. J Vasc Surg. 2007;46:576-580. |
| 16. | Sheldon GF, Lim RC, Yee ES, Petersen SR. Management of injuries to the porta hepatis. Ann Surg. 1985;202:539-545. |