Published online Aug 14, 2008. doi: 10.3748/wjg.14.4776
Revised: June 30, 2008
Accepted: July 7, 2008
Published online: August 14, 2008
AIM: To evaluate a new technique of temporary ileal anastomotic stoma, following small bowel resection, in patients where the anastomosis is anticipated to have borderline margins with dubious viability.
METHODS: Five patients underwent enterectomy and partially anastomosed end-loop ileostomy at the University Hospital of Larissa between 2000 and 2006. Enterectomy was performed because of conditions such as mesenteric vascular occlusive disease, radiation entritis and small bowel injury.
RESULTS: Postoperatively, none of the patients developed any stoma-related or anastomotic complications. There were no major complications. All patients were discharged between the 8th and 15th day after the procedure, and the stoma was closed 3 wk to 4 wk later.
CONCLUSION: We believe that our proposed modification of end-loop ileostomy is a simple, quick and safe technique with minimal stoma-related morbidity, and with simple and safe reversion. This technique can be considered as a useful option in the treatment of ischemic or radiation-induced enteritis, and in the management of severe intestinal trauma.
- Citation: Tepetes K, Liakou P, Balogiannis I, Kouvaraki M, Hatzitheofilou K. Modification of end-loop ileostomy for the treatment of ischemic or radiation enteritis. World J Gastroenterol 2008; 14(30): 4776-4778
- URL: https://www.wjgnet.com/1007-9327/full/v14/i30/4776.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.4776
| Patient | Age/Sex | Diagnosis | Procedure | Time of stoma closure (wk) |
| 1 | 65/F | Radiation enteritis ileal obstruction | 50 cm small bowel resection | 4 |
| 2 | 71/F | Radiation enteritis ileal obstruction | 60 cm small bowel resection | 4 |
| 3 | 74/F | Intestinal ischemia | 60 cm small bowel resection | 3 |
| 4 | 72/M | Intestinal ischemia | 80 cm small bowel resection | 4 |
| 5 | 52/M | Blunt abdominal injury, ileal rupture | 50 cm small bowel resection | 3 |
Fecal diversion by colostomy or ileostomy represents an important treatment in colorectal surgery. Fecal diversion may be either temporary for decompression, or permanent for palliation. The indications for fecal diversion include inflammatory bowel diseases, familial adenomatous polyposis, colorectal carcinoma, nongastrointestinal obstructing tumors, pelvic sepsis, trauma, diverticulitis, fistulas, ischemic bowel disease, radiation enteritis, pseudomembranous enterocolitis, fecal incontinence and paraplegia[1].
An ileostomy may be performed as an end stoma, or as a loop stoma constructed either for decompression of the gastrointestinal tract or for the protection of a distal colonic anastomosis. The majority of loop ileostomies are performed as a temporary treatment, except for those performed for palliation (i.e. non-respectable tumors in patients with low expected survival)[2-5]. Occasionally, a small bowel stoma is required in patients with high risk of small intestinal anastomosis.
In this report, we present a new technique of ileal anastomotic stoma, following small bowel resection, in patients in whom the anastomosis is anticipated to have borderline margins with dubious viability. These include patients with mesenteric ischemia, radiation induced stenosis or fistulas, bowel necrosis due to hernias or adhesions, intestinal trauma and necrotizing enterocolitis in children[6].
Five patients underwent enterectomy and partially anastomosed end-loop ileostomy at the University Hospital of Larissa between 2000 and 2006. The patient’s mean age at stoma formation was 66 years (range, 52-74 years). There were three female and two male patients, and all were Caucasian. Enterectomy was performed secondary to mesenteric vascular occlusive disease, radiation entritis and small bowel injury. The clinical characteristics of patients are shown in Table 1.
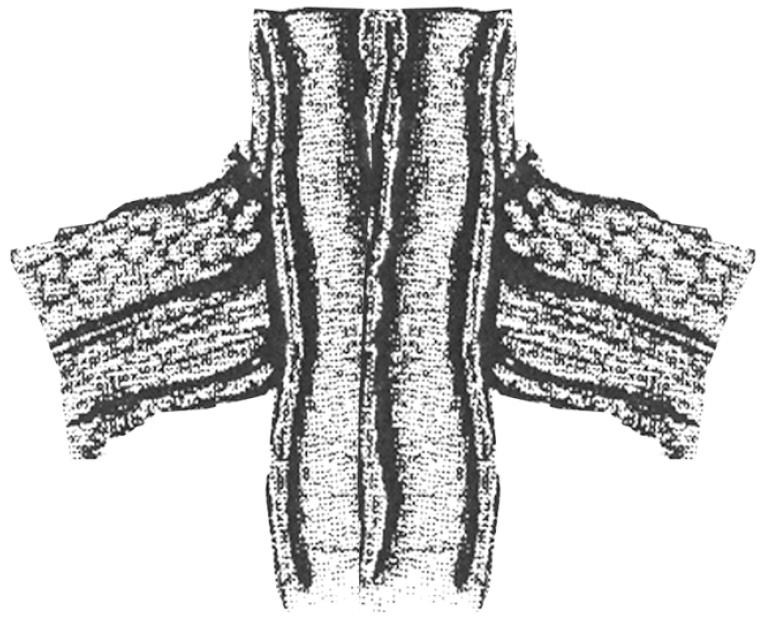
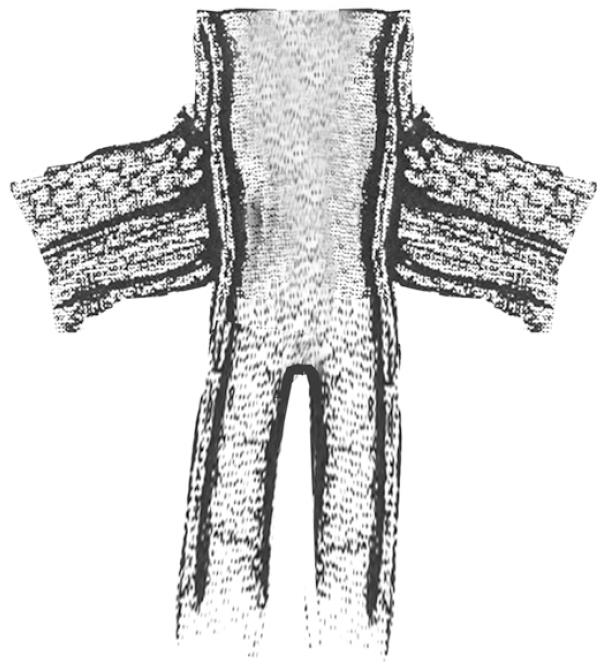
Following resection of the diseased intestinal segment, the afferent and efferent limbs were anastomosed side-to-side using a GIA 100-38 linear stapler (Autosuture, Norwalk, Connecticut, USA; Figure 1). The common blind end remained open and was brought out as a stoma (Figure 2). Using this technique the integrity and the viability of both limbs could be inspected and both the proximal and distal bowel loops were vented.
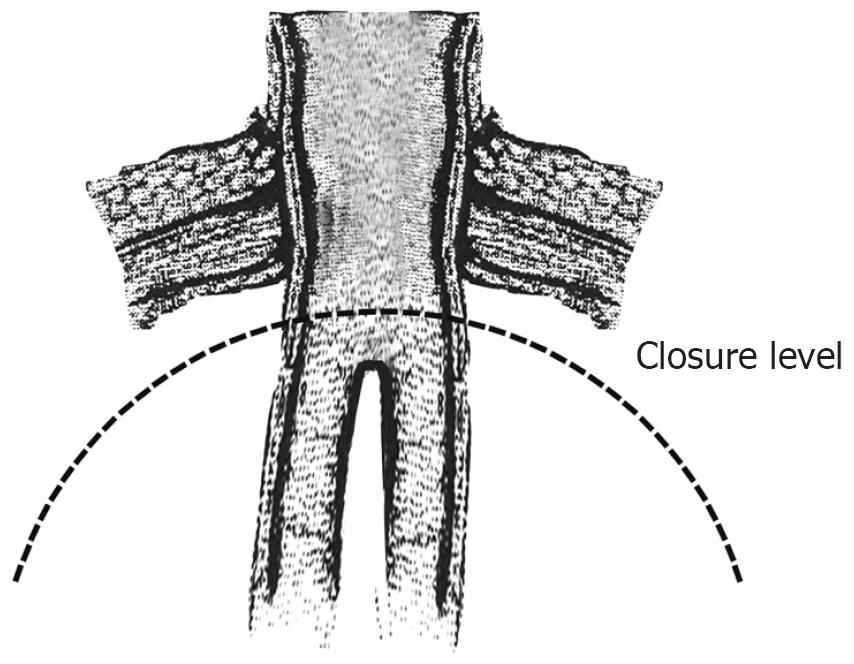
Closure of the enterostomy is a simple procedure that can be performed under local anesthesia and sedation. The common blind end-stoma was mobilized from the skin, subcutaneous tissue and fascia and was closed just below the fascia level using a TA-55 stapler (Autosuture, Norwalk, Connecticut, USA).
The short amputation of the common limb (4-5 cm) enabled side-to-side anastomosis to restore anatomic continuity without sacrificing any length of the intestines (Figure 3).
Closure of the stoma was accomplished in 3 wk to 4 wk. Direct inspection of both limbs of the already fashioned side-to-side anastomosis was possible during that period.
Postoperatively, none of the patients developed any stoma-related or anastomotic complication. There were no major complications. Two of the five patients developed a mild wound infection which was managed conservatively with local measures. All patients were discharged between the 8th and 15th day after the procedure and the stoma was closed 3 wk to 4 wk later.
Small bowel enterostomies are occasionally required following emergent small bowel resection in conditions such as bowel ischemic, and inflammatory or traumatic disorders. The clinical setting of these patients requires a quick and safe procedure preserving as much of the intestinal length as possible. A small intestinal diverting stoma, however, carries significant morbidity, mostly due to fluid, electrolyte and nutrient imbalance. Furthermore, the restoration of intestinal continuity usually requires meticulous dissection of the afferent and efferent segments and the formation of a new anastomosis, usually under general anesthesia.
Even a loop or “end loop” stoma requires an anastomosis for its closure, as well as peritoneal breaching for the intraabdominal position of the anastomotic segment.
Because of the aforementioned reasons, closure itself is associated with complications such as small bowel obstruction (0%-15%), anastomotic leak (0%-8%), fistula formation (0%-7%), wound infection (up to 18%) and development of hernia at the stoma site (1%-12%)[7,8].
Finally, morbidity related to general anesthesia should also be taken into consideration, because the majority of these patients have poor general health and nutritional status secondary to the underlying medical disorders[9].
A special variant of ileal stoma was first described by Bishop, in 1957, for the treatment of meconium ileus, and shortly afterwards by Santuli, in 1961, for the treatment of congenital atresia of the intestines in pediatric patients. After resection of the diseased bowel, either the distal (Bishop) or the proximal (Santuli) limb is brought out as a stoma, while the remaining limb is anastomosed end-to-side to the former, a few centimeters below the abdominal wall, in order to avoid creating a blind loop. These stomas provide satisfactory decompression of the proximal bowel, along with the passage of some amounts of intestinal content into the distal limb. Although the construction of such stomas is rather demanding, they have the advantage of easy closure, even under local anesthesia.
However, the presence of an intrabdominal anastomosis carries several risks such as obstruction, breakdown, leakage and sepsis. Nevertheless, the Santuli enterostomy, the mirror image of the Bishop procedure, has been reported to be efficacious in adult patients as well, in conditions such as mesenteric ischemia, bowel necrosis due to an incarcerated hernia and trauma[10-12].
In the present study, we modified the anastomotic stoma, a “partially anastomosed end-loop ileostomy” for the treatment of adult patients, who presented with conditions such as small intestinal necrosis due to extended mesenteric vascular occlusive disease, radiation-induced stenosis, and intestinal trauma with macroscopically borderline margins with respect to the viability of the intestinal wall after extended bowel resection. In order to preserve as much length of the small intestine as possible, and also to protect the terminal ileum, we constructed a side-to-side anastomosis between the remaining bowel limbs and fastened the common blind end as a stoma. Thus, spontaneous decompression was achieved along with the ability to easily inspect the bowel integrity through the stoma. Furthermore, both limbs were vented, and the distal limb received bowel contents within 48 h, minimizing massive intestinal fluid loss. Thus, we created a low output ileo-cutaneous fistula. The formation of the anastomosis in a side-to-side fashion provides richer blood supply, augmenting the viability of its intrabdominal portion. Moreover, the procedure requires less time than an end-to-side anastomosis. The formation of such a stoma was simple and quick, with no risk of stenosis or kinking. We believe that the short duration of our technique is an important advantage since operative time is a critical factor in the survival of these patients (urgent cases, unstable patients, “damage control” in trauma)[6].
In addition, closure of the stoma can be performed easily and quickly under local anesthesia, by mobilizing the common limb from the abdominal wall and stapling it just below the fascia without entering the abdominal cavity. Moreover, it can be performed within 4 wk, since the integrity of the intestine can be assured by direct inspection of both limbs.
We believe that our proposed modification of end-loop ileostomy is a simple, fast and safe technique with minimal stoma-related morbidity, and with simple and safe reversion. It should be considered as a useful treatment option in patients with ischemic and radiation-induced enteritis, and in the management of severe intestinal trauma.
Enterostomies are usually high output stomas, that often result in fluid and electrolyte depletion.
A variety of techniques have been proposed for the formation of a low morbidity ileostomy.
Our technique is a combination of a low output stoma and an anastomosis with minimal risk of rupture.
This technique should be taken into consideration in patients who are at a high risk of small bowel resection such as those with ischemic and radiation enteritis. We believe that our technique provides a fast, simple and safe surgical treatment of patients with small bowel necrosis.
Our proposed modification of end-loop ileostomy appears to be simple, fast and safe technique with minimal stoma-related morbidity, and with simple and safe reversion. It should be considered as a useful option in the treatment of ischemic and radiation-induced enteritis, and in the management of severe intestinal trauma.
Peer reviewers: Paul E Sijens, PhD, Associate Professor, Department of Radiology, UMCG, Groningen 9713GZ, the Netherlands; Alessandrhera, MD, FACS, FASCRS, Assistant Professor, Department of Surgery, University of Chicago, 5841 S. Maryland Ave, MC 5031, Chicago IL 60637, United States
S- Editor Zhong XY L- Editor Anand BS E- Editor Lin YP
| 1. | Kaidar-Person O, Person B, Wexner SD. Complications of construction and closure of temporary loop ileostomy. J Am Coll Surg. 2005;201:759-773. |
| 2. | Shellito PC. Complications of abdominal stoma surgery. Dis Colon Rectum. 1998;41:1562-1572. |
| 3. | O'Toole GC, Hyland JM, Grant DC, Barry MK. Defunctioning loop ileostomy: a prospective audit. J Am Coll Surg. 1999;188:6-9. |
| 4. | Garcia-Botello SA, Garcia-Armengol J, Garcia-Granero E, Espi A, Juan C, Lopez-Mozos F, Lledo S. A prospective audit of the complications of loop ileostomy construction and takedown. Dig Surg. 2004;21:440-446. |
| 5. | Mosdell DM, Doberneck RC. Morbidity and mortality of ostomy closure. Am J Surg. 1991;162:633-636; discussion 636-637. |
| 6. | Lange R, Dominguez Fernandez E, Friedrich J, Erhard J, Eigler FW. The anastomotic stoma: a useful procedure in emergency bowel surgery. Langenbecks Arch Chir. 1996;381:333-336. |
| 7. | Hasegawa H, Radley S, Morton DG, Keighley MR. Stapled versus sutured closure of loop ileostomy: a randomized controlled trial. Ann Surg. 2000;231:202-204. |
| 8. | Hull TL, Kobe I, Fazio VW. Comparison of handsewn with stapled loop ileostomy closures. Dis Colon Rectum. 1996;39:1086-1089. |
| 9. | Bakx R, Busch OR, Bemelman WA, Veldink GJ, Slors JF, van Lanschot JJ. Morbidity of temporary loop ileostomies. Dig Surg. 2004;21:277-281. |
| 11. | Anadol AZ, Topgul K. Santulli enterostomy revisited: indications in adults. World J Surg. 2006;30:1935-1938. |
| 12. | Wong KS, Remzi FH, Gorgun E, Arrigain S, Church JM, Preen M, Fazio VW. Loop ileostomy closure after restorative proctocolectomy: outcome in 1,504 patients. Dis Colon Rectum. 2005;48:243-250. |