Published online Aug 21, 2007. doi: 10.3748/wjg.v13.i31.4274
Revised: April 23, 2007
Accepted: April 26, 2007
Published online: August 21, 2007
Intussusception of the appendix is a rare condition. Most cases are diagnosed during operation of the patients suspected to have appendicitis. In this report we present a seventy one year-old man with a history of periumbilical intermittent abdominal pain for several months. None of the paraclinical tests were useful for determining the diagnosis. Colonoscopy performed during the last episode of abdominal pain revealed the prolapsed appendix in the cecum and the patient was sent to the operating room. Macroscopic appearance of the appendix was normal and microscopic examination revealed follicular hyperplasia and acute focal appendicitis. Appendiceal intussusception should be considered in differential diagnosis of intermittent abdominal pain and colonoscopic diagnosis could be very important to avoid dangerous or unnecessary decision making.
- Citation: Tavakkoli H, Sadrkabir SM, Mahzouni P. Colonoscopic diagnosis of appendiceal intussusception in a patient with intermittent abdominal pain: A case report. World J Gastroenterol 2007; 13(31): 4274-4277
- URL: https://www.wjgnet.com/1007-9327/full/v13/i31/4274.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i31.4274
Intussusception of the appendix into the cecum is a very rare type of intussusception, with an incidence of 0.01%[1]. Its clinical picture may mimic various acute and chronic abdominal diseases and colonoscopically it should be differentiated from a cecal polyp or mass[2,3]. Misdiagnosis has resulted in patients undergoing colonoscopic poly-pectomy to subsequent perforation and peritonitis[4]. More over, an intussuscepted appendix may be regarded as a malignancy and the patient will undergo unnecessary partial resection of the ileum, cecum or hemicolectomy[5,6].
In this report we present colonoscopic diagnosis of appendiceal intussusception without an underlying cause.
A seventy one-year old man presented with abdominal pain relapsing every one to two months during the nine months before diagnosis. The pain did last 24 to 48 h in each episode. It was a sustained periumbilical dull pain with colicky exacerbations and was associated with nausea and loss of appetite. Physical examination revealed a soft, non-distended abdomen with mild periumbilical tenderness and normal bowel sounds. No abdominal mass was palpated. Blood or mass was not detected in rectal examination. The remainder of his physical examination and vital signs were normal. Complete blood count examination (CBC), stool examination, upright and supine abdominal radiographies were normal. Each time the pain was relieved by administration of antispasmodic medication. In one of the episodes the patient was admitted to the hospital due to right lower quadrant tenderness on physical exam and appendectomy was planned. Before going to the operating room the pain was relieved spontaneously. All paraclinical tests including CBC, stool examination, urine analysis, liver function tests and abdominopelvic sonography during the episode and CT scanning, taken after the pain episode, were reported as normal. He had refused to do colonoscopy in previous episodes of pain.
He denied any past history of weight loss, urinary symptoms, melena, hematochezia constipation or recent change in bowel habits. He reported a family history of metastatic neuroendocrine tumor of cecal origin in his brother and adenocarcinoma of the colon in a cousin.
He was visited in our hospital during the last episode of abdominal pain for the first time. He had a mild tenderness in the right lower quadrant without guarding or rigidity. A total colonoscopy was accomplished before the symptoms completely subsided. The mucosal appearance of all parts was normal up to the cecum where a polypoid erythematous lesion with a diameter of 1.5 cm was observed at the cecal base (Figure 1). The border of the lesion was firm and its central part was soft (Figure 2).
Despite relief of symptoms, an exploratory laparotomy and appendectomy was considered because of a strong family history of malignancy and long lasting symptoms. At laparotomy the appendix had not an inflammatory feature and was not intussuscepted but it could be pushed easily in and out of the cecum. No other abnormality was observed and a simple appendectomy was performed.
Gross appearance of the appendix did not show any sign of congestion or dilatation of small blood vessels on the serosal surface. Cut sections did not show pus or inspissated fecal materials.
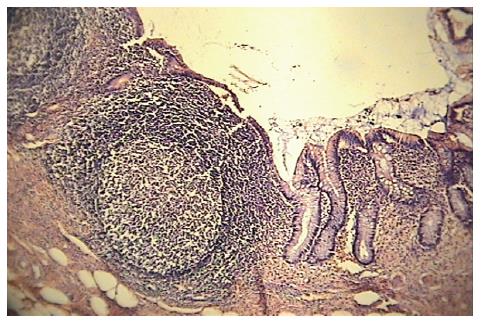
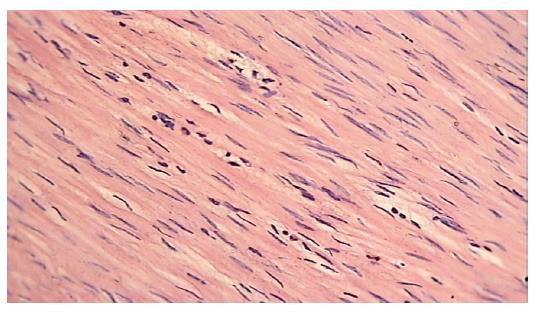
Histological examination of the specimen was only remarkable for follicular hyperplasia in part of the mucosa (Figure 3) and infiltration of muscularis propria by a few polymorphonuclear leukocytes compatible with acute focal appendicitis (Figure 4). The patient was discharged in a few days and he was asymptomatic after 5 mo. Since he had episodes of abdominal pain every 1 to 2 mo, this would be a good sign of recovery. The patient’s follow up will be continued.
Intussusception of the appendix may occur at any age. In a review of 118 cases, the age of occurrence is reported to range from 10 mo to 75 years with an average age of 16 years. The majority occurred in children younger than 10 years of age, most commonly in males (male: female ratio 4-5:1)[7]. Four different presentations have been described for appendiceal intussusception. The first type of presentation mimics acute appendicitis. The second type presents with typical symptoms of intussusception, that is, abdominal pain and vomiting for several days, occasionally associated with diarrhea and melena. The third type presents with recurrent bouts of right lower quadrant pain, vomiting and melena, which may last for weeks to months. The final presentation is totally asymptomatic. Painless hematochezia may also be present[8].
Specific anatomic requirements as well as pathological conditions causing irritation or increasing peristalsis should be present for appendiceal intussusception to occur[9]. Pathologic lesions within the lumen of the appendix that may lead to intussusception have been reported as calcified fecalith[10], mucosa-associated lymphoma[11], juvenile polyp[12], villus adenoma[13], mucocele[14], adenocarcinoma[15,16], carcinoid tumor[17], endometriosis[18,19] and inflammatory polyp in Crohn’s disease[20]. In some cases no underlying abnormality is identified and abnormal peristalsis caused by local irritation seems to be the essential mechanism. While some authors favor hyperperistalsis of the vermiform appendix, others consider the intestinal peristalsis responsible for milking the appendix into the cecum[21,22]. In our case, there was no significant pathologic lead point for intussusception.
According to the literature, intussusception of the appendix has been classified into different types (Table 1)[23]. In our case, colonoscopic appearance and surgical findings were compatible with type III of this classification.
| Intussusceptions | Invaginated portion of appendix | Type |
| Distal appendix | Tip | I |
| Proximal appendix | Tip | II |
| Cecum | Base | III |
| Distal appendix | Proximal wall | IV |
| Entire appendix | Entire appendix | V |
Spontaneous reduction of appendiceal intussusception has been reported[24]. In our patient the appendix had been already reduced incidentally before the laparotomy, but according to the surgery reports it was easily possible to push it back into the cecum from the base. Therefore, the episodic exacerbations of the abdominal pain can be explained by intermittent intussusceptions of the appendix.
Although more than 200 cases of appendiceal intussusception have been reported in the literature[2], very few have been diagnosed colonoscopically. Preoperative diagnosis of appendiceal intussusception due to similarity of symptoms with appendicitis is extremely difficult. Several imaging modalities are of limited value in diagnosing this rare condition, including barium enema, transabdominal sonography, CT scan and endoscopic ultrasonography. Sonographic findings include multiple concentric hypoechoic and hyperechoic rings[25,26]. On barium enema, oval, round (in partial invagination) and finger-like filling defect (in complete invagination) is demonstrated at the tip of the cecum. The classic coiled-spring appearance in appendiceal intussusception is more obvious on double contrast barium enema[27,28]. Intussusception has classically been described as having a target, layered, sausage-shaped or reniform appearance on CT; when present, this appearance is virtually pathognomonic[29]. Endoscopic sonography demonstrates a multi-concentric structure and enables the tentative procedure for diagnosis of appendiceal intussusception[30]. In fact, few cases of appendiceal intussusception have been diagnosed by colonoscopy. The appearance is described as a polypoid or mushroom like lesion with a central dimple found in the anatomic place of the appendix[2,31,32].
Different approaches have been used to treat appendiceal intussusceptions that diagnosed by colonoscopy. Although two cases of successful colonoscopic appendectomy with the use of an endoloop ligating system has been reported[33,34] this procedure can be harmful in patients with partial intussusception of appendix[35]. As adults will typically have lead points which are frequently neoplastic[36], laparotomy is indicated. Cases of appendiceal intussusception can be treated by appendectomy, but associated neoplasms may require performance of a right hemicolectomy[37,38].
Although all imaging studies including a CT scan failed to reveal any pathologic finding in the presented case, a strong family history of malignancy and frequent relapses of abdominal pain necessitated the laparotomy to exclude undetermined underlying malignancy and relieve the symptoms.
In conclusion, colonoscopy is a useful diagnostic tool in evaluation of unexplained abdominal pain and equivocal radiographic studies and it is accurate and valuable in diagnosis of intussusception of the appendix and selecting the appropriate management.
S- Editor Zhu LH L- Editor Alpini GD E- Editor Lu W
| 1. | Langsam LB, Raj PK, Galang CF. Intussusception of the appendix. Dis Colon Rectum. 1984;27:387-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Duncan JE, DeNobile JW, Sweeney WB. Colonoscopic diagnosis of appendiceal intussusception: case report and review of the literature. JSLS. 2005;9:488-490. [PubMed] |
| 3. | Ram AD, Peckham C, Akobeng AK, Thomas AG, David TJ, Patel L. Inverted appendix mistaken for a polyp during colonoscopy and leading to intussusception. J Cyst Fibros. 2005;4:203-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Fazio RA, Wickremesinghe PC, Arsura EL, Rando J. Endoscopic removal of an intussuscepted appendix mimicking a polyp--an endoscopic hazard. Am J Gastroenterol. 1982;77:556-558. [PubMed] |
| 5. | Flint R, Wright T. Intussusception of a normal appendix: how to avoid a right hemicolectomy. N Z Med J. 2003;116:U403. [PubMed] |
| 6. | Kawamura YJ, Toyama N, Kasamatsu T, Ota M, Konishi F. Intussusception of appendiceal adenoma mimicking invasive carcinoma. Endoscopy. 2002;34:749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Rudek B, von Herbay A, Schmidt J. Intussusception of the appendix secondary to mucinous cystadenoma. Dig Surg. 2001;18:422-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Reijnen JA, Festen C, Joosten HJ. Chronic intussusception in children. Br J Surg. 1989;76:815-816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Kegelaers B, Storms P, Eyckens A, Sebrechts R. Intussusception of vermiform appendix. A case report and review of the literature. Acta Chir Belg. 1996;96:287-290. [PubMed] |
| 10. | Itoh J, Soeno T, Koizumi R. Intussusception of the appendix with a calcified fecalith. Jpn J Surg. 1987;17:195-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Karabulut R, Sönmez K, Türkyilmaz Z, Yilmaz Y, Akyürek N, Başaklar AC, Kale N. Mucosa-associated lymphoid tissue lymphoma in the appendix, a lead point for intussusception. J Pediatr Surg. 2005;40:872-874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Bailey DJ, Courington KR, Andres JM, Bagwell CE, Hitchcock CL. Cecal polyp and appendiceal intussusception in a child with recurrent abdominal pain: diagnosis by colonoscopy. J Pediatr Gastroenterol Nutr. 1987;6:818-820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Tonsekar KS, Cacdac R, Ashare R, Libcke JH. Villous adenoma of the vermiform appendix with cecal intussusception: a case report and review of literature. Am Surg. 1994;60:982-984. [PubMed] |
| 14. | Tsunoda T, Eto T, Maeda H, Mochinaga N, Terada M, Matsuo S, Tsuchiya R, Takahara Y. Intussusception of an appendiceal mucocele: report of a case. Surg Today. 1992;22:470-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Chen YC, Chiang JM. Appendiceal intussusception with adenocarcinoma mimicking a cecal polyp. Gastrointest Endosc. 2000;52:130-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Takahashi M, Sawada T, Fukuda T, Furugori T, Kuwano H. Complete appendiceal intussusception induced by primary appendiceal adenocarcinoma in tubular adenoma: a case report. Jpn J Clin Oncol. 2003;33:413-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Kantarovsky A, Levy RD, Smit DP, Grayson W. Intussusception of appendix with carcinoid tumour. A case report. S Afr J Surg. 1993;31:104-106. [PubMed] |
| 18. | Mann WJ, Fromowitz F, Saychek T, Madariaga JR, Chalas E. Endometriosis associated with appendiceal intussusception. A report of two cases. J Reprod Med. 1984;29:625-629. [PubMed] |
| 19. | Martin LF, Tidman MK, Jamieson MA. Appendiceal intussusception and endometriosis. J Can Assoc Radiol. 1980;31:276-277. [PubMed] |
| 20. | Solomon DJ, Freson M, Price SK. Complete appendicular inversion: the "inside-out" appendix. An unusual presentation of Crohn's disease. A case report and review of the literature. J Belge Radiol. 1991;74:115-116. [PubMed] |
| 21. | Akbayir N, Yildirim S, Sökmen HM, Kiliç G, Erdem L, Alkim C. Intussusception of vermiform appendix with microscopic melanosis coli: a case report. Turk J Gastroenterol. 2006;17:233-235. [PubMed] |
| 22. | Ozuner G, Davidson P, Church J. Intussusception of the vermiform appendix: preoperative colonoscopic diagnosis of two cases and review of the literature. Int J Colorectal Dis. 2000;15:185-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 23. | Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 13-2000. A 26-year-old woman with bouts of abdominal pain, vomiting, and diarrhea. N Engl J Med. 2000;342:1272-1278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 24. | Komine N, Yasunaga C, Nakamoto M, Shima I, Iso Y, Takeda Y, Nakamata T. Intussusception of the appendix that reduced spontaneously during follow-up in a patient on hemodialysis therapy. Intern Med. 2004;43:479-483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 25. | Maglinte DD, Fleischer AC, Chua GT, Kelvin FM. Sonography of appendiceal intussusception. Gastrointest Radiol. 1987;12:163-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Pumberger W, Hörmann M, Pomberger G, Hallwirth U. Sonographic diagnosis of intussusception of the appendix vermiformis. J Clin Ultrasound. 2000;28:492-496. [PubMed] [DOI] [Full Text] |
| 27. | Koumanidou C, Vakaki M, Theofanopoulou M, Nikas J, Pitsoulakis G, Kakavakis K. Appendiceal and appendiceal-ileocolic intussusception: sonographic and radiographic evaluation. Pediatr Radiol. 2001;31:180-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 28. | Levine MS, Trenkner SW, Herlinger H, Mishkin JD, Reynolds JC. Coiled-spring sign of appendiceal intussusception. Radiology. 1985;155:41-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 45] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 29. | Luzier J, Verhey P, Dobos N. Preoperative CT diagnosis of appendiceal intussusception. AJR Am J Roentgenol. 2006;187:W325-W326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 30. | Tseng PH, Lee YC, Chiu HM, Wu MS, Lin JT, Wang HP. Appendiceal intussusception diagnosed with endoscopic sonography. J Clin Ultrasound. 2006;34:348-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 31. | Chijiiwa Y, Kabemura T, Toyota T, Tanaka A, Misawa T. Endoscopic appearance of the intussuscepted appendix and accurate preoperative diagnosis. Am J Gastroenterol. 1988;83:1301-1303. [PubMed] |
| 32. | Ryu BY, Kim TH, Jeon JY, Kim HK, Choi YH, Baik GH. Colonoscopic diagnosis of appendiceal intussusception: a case report. J Korean Med Sci. 2005;20:680-682. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 33. | de Hoyos A, Monroy MA, Gallegos C, Checa G. Intussusception of the appendix resected at colonoscopy. Endoscopy. 2006;38:763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 34. | Sriram PV, Seitz U, Soehendra N, Schroeder S. Endoscopic appendectomy in a case of appendicular intussusception due to endometriosis, mimicking a cecal polyp. Am J Gastroenterol. 2000;95:1594-1596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 35. | Pardoll PM, Wilcoxen JK, Trudeau WL. Primary asymptomatic appendiceal intussusception: a colonoscopic view. Gastrointest Endosc. 1976;23:44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 36. | Thomas RE, Maude K, Rotimi O. A case of an intussuscepted neuroendocrine carcinoma of the appendix. World J Gastroenterol. 2006;12:971-973. [PubMed] |
| 37. | Miyahara M, Saito T, Etoh K, Shimoda K, Kitano S, Kobayashi M, Yokoyama S. Appendiceal intussusception due to an appendiceal malignant polyp--an association in a patient with Peutz-Jeghers syndrome: report of a case. Surg Today. 1995;25:834-837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 38. | Sadahiro S, Ohmura T, Yamada Y, Saito T, Akatsuka S. A case of cecocolic intussusception with complete invagination and intussusception of the appendix with villous adenoma. Dis Colon Rectum. 1991;34:85-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |