Published online Aug 21, 2007. doi: 10.3748/wjg.v13.i31.4219
Revised: April 10, 2007
Accepted: April 16, 2007
Published online: August 21, 2007
AIM: To accurately assess the prevalence of GERD symptoms in general practice.
METHODS: 4139 consecutive patients (2025 men and 2114 women with a mean age of 43 years), who first attended the Outpatient Department of General Medicine and Emergency Care at Toho University Omori Hospital, were asked to respond to the F-scale questionnaire regardless of their chief complaints. The questionnaire is a self-report instrument, written in a simple and easy-to-understand language, containing 12 questions.
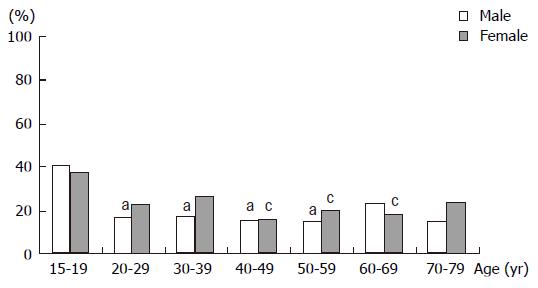
RESULTS: Of 4139 subjects, 1554 patients (37.6%) were identified as GERD according to their F-scale score (> 7). However, there were only 45 consultations (1.1%) for typical GERD symptoms. Although GERD symptoms are common in adults of all ages, the prevalence of GERD was highest in the 20-29 years age group and the age group 70-79 years had the lowest prevalence for both males and females.
CONCLUSION: Although there was a high rate indicating GERD in our primary care population, only 1.1% of outpatients attended our hospital with a chief complaint of GERD symptoms. Since about one-third of GERD patients are affected by atypical symptoms, general physicians need to be cautious about extrapolating these results to patients with a chief complaint other than typical GERD symptoms.
- Citation: Watanabe T, Urita Y, Sugimoto M, Miki K. Gastro-esophageal reflux disease symptoms are more common in general practice in Japan. World J Gastroenterol 2007; 13(31): 4219-4223
- URL: https://www.wjgnet.com/1007-9327/full/v13/i31/4219.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i31.4219
Symptoms of gastro-esophageal reflux disease (GERD) are common, affecting 10%-30% of the population in Western countries[1]. Recently, the prevalence of GERD is also increasing in the Japanese population with a high prevalence of atrophic gastritis[2]. Although GERD symptoms are common in adults of all ages, the prevalence of reflux esophagitis is increasing with age, when evaluated endoscopically[3]. However, limitations in the available diagnostic tests and a bias in subjects tested may result in a lower prevalence of GERD. Since the symptoms are accompanied by endoscopic esophagitis in up to 50% of individuals with GERD[4,5], and endoscopy is routinely used in patients with dyspeptic symptoms in Japan, it has been difficult to diagnose GERD accurately by endoscopy. Furthermore, accurate quantitative estimates of the prevalence of GERD are difficult to obtain because GERD symptoms vary, and there has been no gold standard for the diagnosis of GERD[6,7].
Recently, a simple questionnaire (F-scale) to score GERD symptoms has been developed in Japan[8]. Results using the F-scale have been shown to correlate with endoscopic findings. Diagnosis on the basis of history is simple and noninvasive and it has been favored in general practice. The aim of this study was to accurately assess the prevalence of GERD symptoms in general practice.
Between August 2005 and April 2006, 4139 consecutive patients (2025 men and 2114 women with a mean age of 43 years), who first attended the Outpatient Department of General Medicine and Emergency Care at Toho University Omori Hospital, were enrolled in the present study regardless of their chief complaint. Informed consent was obtained from all patients. The study was carried out in accordance with the Declaration of Helsinki, and was approved by the ethical committee at Toho University.
All of the patients who first attend our hospital were asked to respond to the F-scale questionnaire regardless of their chief complaints. The questionnaire is a self-report instrument, written in simple and easy-to-understand language, containing 12 questions. As reported previously by Kusano et al[8], the following definitions were used to identify symptoms in the F-scale: (1) Do you get heartburn; (2) Does your stomach feel bloated?; (3) Does your stomach ever feel heavy after meals?; (4) Do you sometimes subconsciously rub your chest with your hand?; (5) Do you ever feel sick after meals?; (6) Do you get heartburn after meals?; (7) Do you have an unusual sensation in your throat?; (8) Do you feel full while eating meals?; (9) Do some things get stuck when you swallow?; (10) Do you get bitter liquid coming up into your throat?”; (11) Do you burp a lot?; and (12) Do you get heartburn if you bend over? Symptom frequency was measured on the following scale: never = 0; occasionally = 1; sometimes = 2; often = 3; and always = 4.
If the patient scores more than 7 points, GERD is considered to be present.
All values are expressed as means ± SD. Comparisons of groups were made using Student’s t test or χ2 tests as appropriate. A P value of < 0.05 was accepted as indicating statistical significance.
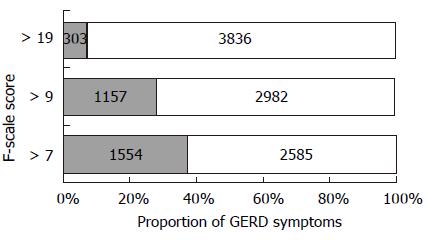
Among 4139 subjects, a total of 1554 patients (37.5%) were identified as having GERD according to their F-scale score (> 7) (Figure 1). However, there were only 45 consultations (1.1%) for typical GERD symptoms, including heartburn and regurgitation. The scores among the population were distributed as follows: 635 (15.3%) subjects scored zero, 959 (23.2%) subjects scored 1 to 3, 576 (13.9%) subjects scored 4 to 5, 415 (10.0%) subjects scored 6 to 7, 395 (9.5%) subjects scored 8 to 9, 348 (8.4%) subjects scored 10 to 12, 274 (6.6%) subjects scored 13 to 15, 238 (5.8%) subjects scored 16 to 19, and 299 (7.2%) subjects scored more than 20. As shown in Figure 1, when the cutoff point for diagnosing GERD was increased to 9-points or 19-points, the prevalence of GERD symptoms was 28.0% (1159/4139) and 7.2% (299/4139), respectively.
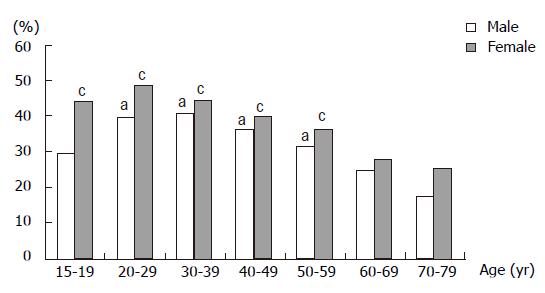
The positive rate for GERD was 705 of 2025 men (35%) and 849 of 2114 women (40%). Unexpectedly, the prevalence of GERD was highest in the 20-29 years age group, followed by the 30-39 years age group and the 40-49 years age group. The age group 70-79 years had the lowest prevalence for both males and females (Figure 2). The prevalence was higher in females than in males in all age groups. The significant differences in the prevalence of GERD were found between those aged 20 to 59 years and those over the age of 70 years in females (Chi-Square test, P < 0.02). The prevalence of GERD was significantly different between those aged 20 to 59 years and those over the age of 70 in males (Chi-Square test, P < 0.05).
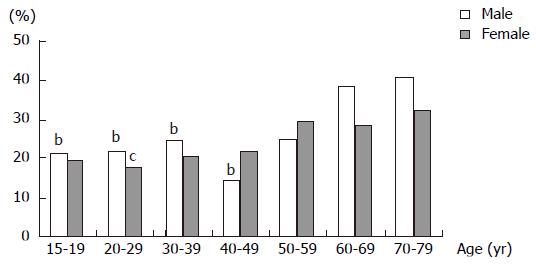
Among the 2585 GERD-negative patients, those with points 1 to 3 were the most prevalent (959 persons, 37.1%). The proportion of patients with a score of zero points was 24.6% (635/2585) and this proportion increased with age in females, whereas in males the proportion was the lowest for the 40-49 years age group and the proportion increased with age in the older groups (Figure 3). Significant differences were found between the 60-69 years and 70-79 years age groups and the 15-19 years, 20-29 years, 30-39 years, and 40-49 years age groups in males (chi-square test, P < 0.01), and between the 20-29 years age group and the 60-69 years and 70-79 years age groups in females (Chi-Square test, P < 0.05).
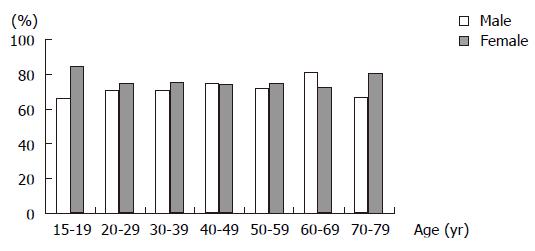
As shown in Figure 4, there was no significant difference in the proportion of patients with a score of more than 9 points among GERD-positive patients for each age group. This suggests that the age distribution of GERD is unchanged if a cutoff point for diagnosing GERD is increased to 10 points. Patients with a high score of more than 19 points were found more frequently in the 15-19 years age group than other groups for both males and females (Figure 5). Significant differences were found between the 15-19 years age group and the 20-29 years, 30-39 years, 40-49 years, and 50-59 years age groups for males, and between the 15-19 years age group and the 40-49 years, 50-59 years, and 60-69 years age groups in females.
GERD refers to the abnormal exposure of esophageal mucosa to gastric contents. Although GERD symptoms affect 10%-30% of the population in Western countries[1], endoscopic esophagitis is less prevalent, and is reported to occur in up to 2% of individuals[9,10]. Only one-third of GERD patients have endoscopic positive findings, while others have no obvious mucosal breaks, even though GERD symptoms are present[11]. Furthermore, up to 50% of endoscopically diagnosed cases of reflux esophagitis present with symptoms other than heartburn or acid regurgitation[12]. Thus, accurate diagnosis of GERD is difficult with currently accepted criteria including symptoms of heartburn and/or acid regurgitation.
Recently, it has been reported that the prevalence of endoscopic esophagitis is increasing in Japan[2,13], with most patients diagnosed as having mild esophagitis, classified into grade A and B in the Los Angeles Classification[2] system. In addition, since the majority of Japanese GERD patients present with mild symptoms[14], most of them may not seek consultation with a gastroenterologist. Nandurkar et al[15] reported that only about half of the patients with GERD symptoms in a community seek health care over a 10-year period and only 19% of them had endoscopy. Isolauri et al[16] showed that medication was used by only 16% of subjects with symptoms in Norway. Based on these previous reports, it is difficult to evaluate a genuine prevalence of GERD in the Japanese population when the study is conducted in the gastroenterology unit of the hospital. Therefore, the present study was carried out in the General Medicine unit to accurately estimate prevalence of GERD symptoms in the Japanese population.
A total of 1554 patients (37.5%) with GERD were identified in the present study. Several population-based surveys have reported typical GERD symptoms, including heartburn and acid regurgitation, occurring at least yearly to range from 26% to 60%[17-20]. These results are concordant with our findings, although GERD symptoms in the general population are less common in the East compared to the West[21,22]. Since H pylori infection may result in hypochlorhydria, as seen in individuals with atrophic gastritis, H pylori-infected patients seem to be at lower risk of developing GERD[23], as is generally observed in Japan where there is a high prevalence of H pylori infection. Several reports showed an increasing trend of GERD in Asian countries in recent years[21,22,24]. Although it has been thought that low acid secretion would be associated with a lower prevalence of GERD in the Far East, Kinoshita et al[25] demonstrated that gastric acid secretion in Japan is rising in both H pylori-positive and -negative individuals. Actually, decreasing prevalence of H pylori was observed in many countries[26-28] as well as in Japan[29].
A decreasing prevalence of H pylori infection, which is positively correlated with age, may influence the age distribution of GERD. Contrary to previous reports[20,30,31], in our study the prevalence of GERD was highest in the 20-29 years age group and decreased with age. Fujiwara et al[30] also reported similar findings that the prevalence of GERD symptoms was relatively higher in the 40-49 years age group and lower in the > 60 years age group. However, as reported by Wong et al[31], age and male sex are considered to be risk factors for heartburn and acid regurgitation even in Asia. There have been a few reports that the prevalence of endoscopic esophagitis or GERD symptoms among men reached a peak when they were in their 20 s. It has been reported in Singapore[21], China[22], Argentina[32], Japan[30], USA[33], and Germany[34] that middle age subjects have GERD symptoms most frequently.
For endoscopically proven erosive esophagitis, Shimazu et al[35] demonstrated that its prevalence was more frequent in older individuals, whereas Mishima et al[24] showed that there were no significant differences in age between subjects with and without erosive esophagitis. For women, the prevalence of GERD increased with age and was higher than in males in the elderly[2]. This variability of prevalence of GERD symptoms may be explained by a heterogeneous symptom pattern. The result of questionnaires in the same patient by different physicians may lead to different conclusions[36]. Therefore, the F-scale was self-assessed by patients in the present study. Second, the lower prevalence may be due to the term ‘heartburn’ being poorly understood by older patients. The proportion of patients with a score of zero points was 24.6% (637/2593) and increased with age in both males (Figure 2) and females (Figure 3) in our study. Among white American subjects, only 35% understood the meaning of heartburn, and the figure dropped to 13% for Asians living in the USA[37], although heartburn and acid regurgitation are known to be specific for GERD. Mishima et al[24] showed that only 51 of 195 patients with endoscopically proven esophagitis had GERD symptoms. This difference may be due to the vague term 'heartburn'. In addition, when the symptoms do not reach the threshold required to define ‘disease’, the patient may not report having heartburn. Such patients might not seek consultation with a gastroenterologist. Finally, severe esophagitis is less common in Japan[14]. Although medical attention to GERD has increased, it has not been easy for endoscopists to detect small mucosal breaks in the distal esophagus by endoscopy. Futhermore, a limitation of the endoscopic survey is that endoscopic reporting is performed by various personnel, leading to some degree of inter-observer variation with endoscopic diagnoses.
Studies that examined the influence of gender on the prevalence of GERD symptoms have found either no differences[19,22,38], female predominance[15,39,40] or male predominance[21,41]. The positive rate for GERD was 705 of 2025 men (35%) and 849 of 2114 women (40%), and the prevalence was higher in females than in males at all age groups in the present study. Although it has been well-known that a possible reason for high prevalence in elderly women is thought to be lumbar kyphosis, a similar age distribution of GERD symptoms in males and females may be due to environmental changes, including decreased prevalence of H pylori infection and atrophic gastritis, or the Westernization of dietary and lifestyle habits.
An epidemiological study on GERD could be considered accurate only when the whole study population undergoes invasive procedures. However, this would dramatically reduce the number of participants and prejudice the response rate of the study. The F-scale, therefore, seems to be the most appropriate test for general practice patients in the management of GERD because there is no requirement of endoscopy. About 4% of the population consults a general practitioner each year because of dyspepsia[42], whereas GERD symptoms are more common in 10%-20% of the population reporting heartburn on a weekly basis in community studies[19,38]. Although increasing attention has been paid recently to the epidemiology of GERD, the lack of a standard definition and of a diagnostic gold standard may make interpretation of data more complex. In the present study, the prevalence of GERD symptoms was 37.5%, higher than previous reports in which GERD was diagnosed by the presence of single specific symptoms, such as heartburn or regurgitation. This suggests that diagnosis by key items is not sufficient to determine a person’s level of GERD and that a multidimensional approach, which covers all symptom aspects, is needed. The F-scale includes two types of symptoms: one is possibly caused by gastro-esophageal reflux (#1, 4, 6, 7, 10, 12); and the other is due to dysmotility of the upper gastrointestinal tract (#2, 3, 5, 8, 9, 11). The F-scale, therefore, is thought to result in a higher prevalence of GERD.
Despite the high prevalence of GERD, most GERD is self managed, and not presented to doctors. Won et al[43] reported that 24% of GERD patients had no GERD symptoms one year after a survey and that the disappearance rate of GERD was numerically greater than the onset rate. Agreus et al[44] showed that more than half of the individuals in their study had changed their main symptom profile to either dyspepsia, irritable bowel syndrome, unspecified symptoms or were symptom-free 1-year after the first survey, although the prevalence of GERD was stable for 7 years. Actually, only 1.1% of 4139 outpatients attended our hospital with a chief complaint of GERD symptoms, despite 1554 being diagnosed as GERD by the F-scale. This indicates that most GERD symptoms do not reach the threshold required to define ‘disease’. Such patients may not seek consultation with a doctor although the result of the questionnaire is positive. Since general practice registers offer the best means of sampling the general population[44], the GERD prevalence of 37.5% obtained in the present study is considered to be accurate for Japan. Furthermore, GERD symptoms are less important as the determinants of consultation in primary care than other symptoms. This is probably due to a high proportion of mild esophagitis in Japanese GERD patients.
In conclusion, GERD symptoms were highly prevalent in our primary care population. However, only 1.1% of outpatients attended our hospital with a chief complaint of GERD symptoms. Although GERD symptoms are common in adults of all ages, the prevalence of GERD was highest in the 20-29 years age group and the group aged 70-79 years had the lowest prevalence in both male and female groups. GERD is associated with organic esophageal findings, such as esophagitis and Barrett’s esophagus, but these are also present in asymptomatic individuals[4,45]. Since up to one-third of GERD patients are affected by atypical symptoms[5], general physicians need to be cautious in extrapolating these results to patients with a chief complaint other than typical GERD symptoms, such as heartburn and regurgitation.
S- Editor Zhu LH L- Editor Lutze M E- Editor Liu Y
| 1. | Holtmann G. Reflux disease: the disorder of the third millennium. Eur J Gastroenterol Hepatol. 2001;13 Suppl 1:S5-S11. [PubMed] |
| 2. | Furukawa N, Iwakiri R, Koyama T, Okamoto K, Yoshida T, Kashiwagi Y, Ohyama T, Noda T, Sakata H, Fujimoto K. Proportion of reflux esophagitis in 6010 Japanese adults: prospective evaluation by endoscopy. J Gastroenterol. 1999;34:441-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 160] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 3. | Johnson DA, Fennerty MB. Heartburn severity underestimates erosive esophagitis severity in elderly patients with gastroesophageal reflux disease. Gastroenterology. 2004;126:660-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 120] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 4. | Ronkainen J, Aro P, Storskrubb T, Johansson SE, Lind T, Bolling-Sternevald E, Graffner H, Vieth M, Stolte M, Engstrand L, Talley NJ, Agréus L. High prevalence of gastroesophageal reflux symptoms and esophagitis with or without symptoms in the general adult Swedish population: a Kalixanda study report. Scand J Gastroenterol. 2005;40:275-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 315] [Cited by in RCA: 315] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 5. | Jaspersen D, Kulig M, Labenz J, Leodolter A, Lind T, Meyer-Sabellek W, Vieth M, Willich SN, Lindner D, Stolte M. Prevalence of extra-oesophageal manifestations in gastro-oesophageal reflux disease: an analysis based on the ProGERD Study. Aliment Pharmacol Ther. 2003;17:1515-1520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 188] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 6. | Kahrilas PJ. Diagnosis of symptomatic gastroesophageal reflux disease. Am J Gastroenterol. 2003;98:S15-S23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | DeVault KR, Castell DO. Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. The Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1999;94:1434-1442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 287] [Cited by in RCA: 252] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 8. | Kusano M, Shimoyama Y, Sugimoto S, Kawamura O, Maeda M, Minashi K, Kuribayashi S, Higuchi T, Zai H, Ino K. Development and evaluation of FSSG: frequency scale for the symptoms of GERD. J Gastroenterol. 2004;39:888-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 302] [Cited by in RCA: 356] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 9. | Mansi C, Savarino V, Mela GS, Picciotto A, Mele MR, Celle G. Are clinical patterns of dyspepsia a valid guideline for appropriate use of endoscopy? A report on 2253 dyspeptic patients. Am J Gastroenterol. 1993;88:1011-1015. [PubMed] |
| 10. | Kagevi I, Löfstedt S, Persson LG. Endoscopic findings and diagnoses in unselected dyspeptic patients at a primary health care center. Scand J Gastroenterol. 1989;24:145-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 53] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Dent J. Gastro-oesophageal reflux disease. Digestion. 1998;59:433-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 84] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Klauser AG, Schindlbeck NE, Müller-Lissner SA. Symptoms in gastro-oesophageal reflux disease. Lancet. 1990;335:205-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 500] [Cited by in RCA: 457] [Article Influence: 13.1] [Reference Citation Analysis (2)] |
| 13. | El-Serag HB, Sonnenberg A, Jamal MM, Inadomi JM, Crooks LA, Feddersen RM. Corpus gastritis is protective against reflux oesophagitis. Gut. 1999;45:181-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 108] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 14. | Okamoto K, Iwakiri R, Mori M, Hara M, Oda K, Danjo A, Ootani A, Sakata H, Fujimoto K. Clinical symptoms in endoscopic reflux esophagitis: evaluation in 8031 adult subjects. Dig Dis Sci. 2003;48:2237-2241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 98] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 15. | Nandurkar S, Locke GR, Murray JA, Melton LJ, Zinsmeister AR, Dierkhising R, Talley NJ. Rates of endoscopy and endoscopic findings among people with frequent symptoms of gastroesophageal reflux in the community. Am J Gastroenterol. 2005;100:1459-1465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Isolauri J, Laippala P. Prevalence of symptoms suggestive of gastro-oesophageal reflux disease in an adult population. Ann Med. 1995;27:67-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 210] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 17. | Stanghellini V. Three-month prevalence rates of gastrointestinal symptoms and the influence of demographic factors: results from the Domestic/International Gastroenterology Surveillance Study (DIGEST). Scand J Gastroenterol Suppl. 1999;231:20-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 152] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 18. | Kennedy T, Jones R. The prevalence of gastro-oesophageal reflux symptoms in a UK population and the consultation behaviour of patients with these symptoms. Aliment Pharmacol Ther. 2000;14:1589-1594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 138] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 19. | Diaz-Rubio M, Moreno-Elola-Olaso C, Rey E, Locke GR, Rodriguez-Artalejo F. Symptoms of gastro-oesophageal reflux: prevalence, severity, duration and associated factors in a Spanish population. Aliment Pharmacol Ther. 2004;19:95-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 166] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 20. | Ruth M, Månsson I, Sandberg N. The prevalence of symptoms suggestive of esophageal disorders. Scand J Gastroenterol. 1991;26:73-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 117] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 21. | Ho KY, Chan YH, Kang JY. Increasing trend of reflux esophagitis and decreasing trend of Helicobacter pylori infection in patients from a multiethnic Asian country. Am J Gastroenterol. 2005;100:1923-1928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 67] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 22. | Chen M, Xiong L, Chen H, Xu A, He L, Hu P. Prevalence, risk factors and impact of gastroesophageal reflux disease symptoms: a population-based study in South China. Scand J Gastroenterol. 2005;40:759-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 92] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 23. | El-Omar EM, Oien K, El-Nujumi A, Gillen D, Wirz A, Dahill S, Williams C, Ardill JE, McColl KE. Helicobacter pylori infection and chronic gastric acid hyposecretion. Gastroenterology. 1997;113:15-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 411] [Cited by in RCA: 399] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 24. | Mishima I, Adachi K, Arima N, Amano K, Takashima T, Moritani M, Furuta K, Kinoshita Y. Prevalence of endoscopically negative and positive gastroesophageal reflux disease in the Japanese. Scand J Gastroenterol. 2005;40:1005-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 117] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 25. | Lim SL, Goh WT, Lee JM, Ng TP, Ho KY. Changing prevalence of gastroesophageal reflux with changing time: longitudinal study in an Asian population. J Gastroenterol Hepatol. 2005;20:995-1001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 49] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 26. | Banatvala N, Mayo K, Megraud F, Jennings R, Deeks JJ, Feldman RA. The cohort effect and Helicobacter pylori. J Infect Dis. 1993;168:219-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 328] [Cited by in RCA: 334] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 27. | Kosunen TU, Aromaa A, Knekt P, Salomaa A, Rautelin H, Lohi P, Heinonen OP. Helicobacter antibodies in 1973 and 1994 in the adult population of Vammala, Finland. Epidemiol Infect. 1997;119:29-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 107] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 28. | Roosendaal R, Kuipers EJ, Buitenwerf J, van Uffelen C, Meuwissen SG, van Kamp GJ, Vandenbroucke-Grauls CM. Helicobacter pylori and the birth cohort effect: evidence of a continuous decrease of infection rates in childhood. Am J Gastroenterol. 1997;92:1480-1482. [PubMed] |
| 29. | Asaka M, Kimura T, Kudo M, Takeda H, Mitani S, Miyazaki T, Miki K, Graham DY. Relationship of Helicobacter pylori to serum pepsinogens in an asymptomatic Japanese population. Gastroenterology. 1992;102:760-766. [PubMed] |
| 30. | Fujiwara Y, Higuchi K, Watanabe Y, Shiba M, Watanabe T, Tominaga K, Oshitani N, Matsumoto T, Nishikawa H, Arakawa T. Prevalence of gastroesophageal reflux disease and gastroesophageal reflux disease symptoms in Japan. J Gastroenterol Hepatol. 2005;20:26-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 81] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 31. | Wong BC, Kinoshita Y. Systematic review on epidemiology of gastroesophageal reflux disease in Asia. Clin Gastroenterol Hepatol. 2006;4:398-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 151] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 32. | Chiocca JC, Olmos JA, Salis GB, Soifer LO, Higa R, Marcolongo M. Prevalence, clinical spectrum and atypical symptoms of gastro-oesophageal reflux in Argentina: a nationwide population-based study. Aliment Pharmacol Ther. 2005;22:331-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 94] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 33. | Majumdar SR, Soumerai SB, Farraye FA, Lee M, Kemp JA, Henning JM, Schrammel P, LeCates RF, Ross-Degnan D. Chronic acid-related disorders are common and underinvestigated. Am J Gastroenterol. 2003;98:2409-2414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 34. | Nocon M, Keil T, Willich SN. Prevalence and sociodemographics of reflux symptoms in Germany--results from a national survey. Aliment Pharmacol Ther. 2006;23:1601-1605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 35. | Shimazu T, Matsui T, Furukawa K, Oshige K, Mitsuyasu T, Kiyomizu A, Ueki T, Yao T. A prospective study of the prevalence of gastroesophageal reflux disease and confounding factors. J Gastroenterol. 2005;40:866-872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 36. | Rothman M, Farup C, Stewart W, Helbers L, Zeldis J. Symptoms associated with gastroesophageal reflux disease: development of a questionnaire for use in clinical trials. Dig Dis Sci. 2001;46:1540-1549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 79] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 37. | Spechler SJ, Jain SK, Tendler DA, Parker RA. Racial differences in the frequency of symptoms and complications of gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2002;16:1795-1800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 113] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 38. | Locke GR, Zinsmeister AR, Talley NJ, Fett SL, Melton LJ. Familial association in adults with functional gastrointestinal disorders. Mayo Clin Proc. 2000;75:907-912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 180] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 39. | Räihä I, Impivaara O, Seppälä M, Knuts LR, Sourander L. Determinants of symptoms suggestive of gastroesophageal reflux disease in the elderly. Scand J Gastroenterol. 1993;28:1011-1014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 40. | Fujiwara Y, Higuchi K, Shiba M, Yamamori K, Watanabe Y, Sasaki E, Tominaga K, Watanabe T, Oshitani N, Arakawa T. Differences in clinical characteristics between patients with endoscopy-negative reflux disease and erosive esophagitis in Japan. Am J Gastroenterol. 2005;100:754-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 71] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 41. | Kay L, Jørgensen T, Jensen KH. Epidemiology of abdominal symptoms in a random population: prevalence, incidence, and natural history. Eur J Epidemiol. 1994;10:559-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 42. | Heikkinen M, Pikkarainen P, Takala J, Julkunen R. General practitioners' approach to dyspepsia. Survey of consultation frequencies, treatment, and investigations. Scand J Gastroenterol. 1996;31:648-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 43. | Wong WM, Lai KC, Lam KF, Hui WM, Huang JQ, Xia HH, Hu WH, Lam CL, Chan CK, Lam SK. Onset and disappearance of reflux symptoms in a Chinese population: a 1-year follow-up study. Aliment Pharmacol Ther. 2004;20:803-812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 44. | Fleming DM. Morbidity registration and the fourth general practice morbidity survey in England and Wales. Scand J Prim Health Care Suppl. 1993;2:37-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 45. | Ronkainen J, Aro P, Storskrubb T, Johansson SE, Lind T, Bolling-Sternevald E, Vieth M, Stolte M, Talley NJ, Agréus L. Prevalence of Barrett's esophagus in the general population: an endoscopic study. Gastroenterology. 2005;129:1825-1831. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 668] [Cited by in RCA: 644] [Article Influence: 32.2] [Reference Citation Analysis (0)] |