Published online Apr 7, 2007. doi: 10.3748/wjg.v13.i13.2004
Revised: December 20, 2006
Accepted: January 4, 2007
Published online: April 7, 2007
Triplication of the gallbladder is a very rare congenital anomaly of the biliary tract; there are only eleven reported cases to date. Gallbladder multiplications are not likely to be discovered unless associated with cholelithiasis, sludge, cholecystitis and carcinoma. Here we report an incidentally diagnosed triplicate gallbladder in a patient with sigmoid diverticulitis; two of the triplicate gallbladder were demonstrated with ultrasound and computed tomography, and an additional galballder was found at surgery.
- Citation: Alicioglu B. An incidental case of triple gallbladder. World J Gastroenterol 2007; 13(13): 2004-2006
- URL: https://www.wjgnet.com/1007-9327/full/v13/i13/2004.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i13.2004
Vesica fellae triplex, also known as the triplication of the gallbladder, is a very rare congenital anomaly of the biliary tract. To our knowledge, only 11 cases have been reported in the literature to date. The first case was described by Huber in a human cadaver in 1752[1]. Multiple gallbladder anomalies are generally discovered if they are associated with symptoms caused by cholelithiasis, sludge, cholecystitis or carcinoma. We report a case of triple gallbladder which was incidentally diagnosed in a patient with sigmoid diverticulitis. Radiological workup revealed a duplication of gallbladder and chronic cholecystitis with sludge formation. However, a triplication was found during surgery.
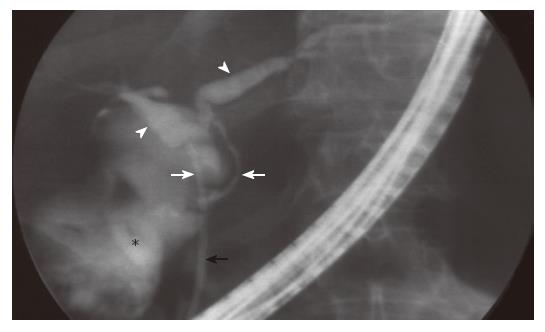
A 54-year-old woman was admitted to emergency department with complaints of nausea, dyspepsia and abdominal pain at the left lower quadrant. On physical examination, tenderness at the left lower quadrant was observed. Complete blood count revealed a mild leukocytosis (11 600/mm3) and blood chemistry revealed an elevated serum alkaline phosphatase level (167 mg/L). Patient was clinically diagnosed to have acute sigmoid diverticulitis. Ultrasonography (US) and computed tomography (CT) of the abdomen revealed a duplicated gallbladder, with thickened wall and considerable sludge in one gallbladder, while tortuous cystic duct but normal wall and luminal content in another gallbladder (Figures 1 and 2). Endoscopic retrograde cholangiopancreatography (ERCP) showed two cystic ducts, normal common hepatic duct, and no luminal opacification (Figure 3). Although her bowel and paracolic spaces had normal appearance, the patient was put on medical treatment for acute diverticulitis. Her symptoms were subsequently improved. Follow-up US examination in the third month revealed almost similar findings to the initial scan; one of the gallbladders had slightly tortuous wall but normal luminal content, while the other one had a 4-mm thickened wall and contained a small amount of sludge.
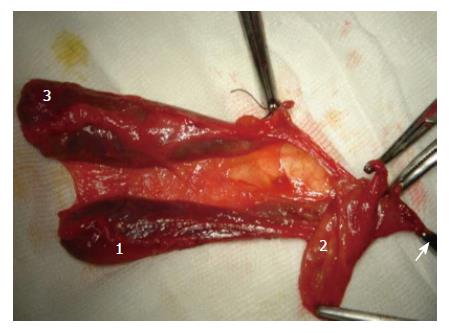
Cholecystectomy was performed to treat the chronic cholecystitis. Two gallbladders that were demonstrated during the radiological workup had normal walls and contained clear fluid (Figure 4). A third gallbladder was unexpectedly discovered during the operation. It had a thick wall and was filled with sludge, and its cystic duct was shorter than others. All gallbladders were dissected after the ligation of their cystic ducts and accompanying arteries. No stone was detected in any of the gallbladders. Pathological diagnosis revealed gallbladder triplication; two of them were normal and the other one showed ulcerated active chronic cholecystitis.
Multiple gallbladders are thought to be caused by the rudimentary bile ducts which failed to regress during embryological development. The persistence of these cellular out-pocketings along the common bile duct and their growth lead to this anomaly. The relationship of the gallbladder to the cystic duct and to the common bile duct seems to be determined by the location of persistent rudimentary duct buds: if the persistent buds originate from the hepatic duct or common bile duct, gallbladders will have separate cystic ducts; if they arise from the cystic duct, the gallbladders share single common cystic duct draining into a normal common bile duct. Based on the anatomic configuration of the cystic ducts, three distinct types are described. The first type is characterized by the presence of multiple gallbladders that drain into the common bile duct via separate cystic ducts. The second type is characterized by the presence of two gallbladders with a common cystic duct entering the common duct, and a third gallbladder with an independent cystic duct. The third type is characterized by the presence of three gallbladders that share a single cystic duct[1,2].
Multiple gallbladders are associated with choleli-thiasis, sludge, cholecystitis, cellular metaplasia and adenocarcinoma. Roeder et al[3] described a patient with cholecystitis and cholelithiasis in one gallbladder, and a papillary adenocarcinoma in the second one. In that case, the remaining gallbladder was intrahepatically located and was otherwise normal. Duplications and triplications are unlikely to be discovered unless there are associated symptoms. That statement was true for all but one of the reported cases[4]. Our case did not have a hepatobiliary symptom. Her anomaly was found incidentally upon her admittance to the hospital for acute diverticulitis.
Until 1979, the preoperative imaging of the biliary tract was limited to oral or intravenous cholecystograms, fat meal studies, conventional tomography and postoperative T-tube cholangiography. In the current practice, biliary imaging is performed with high resolution imaging techniques, such as US, spiral or multislice CT, MRCP (magnetic resonance cholangiopancreatography) and ERCP. Even in the era of modern imaging, most of the recent cases with triple gallbladder were failed to be diagnosed preoperatively[4-6]. In the relevant literature, only one case was diagnosed before surgery[2]. The lack of definitive diagnosis was probably caused by the misinterpretation of the third lumen as a tortuosity of one of the cystic ducts or a gallbladder variation such as a partial transverse septa. US and CT may demonstrate wall thickness, lumen pathology and the number of the gallbladders but are unable to define the exact anatomy of the biliary tree. These techniques should be supplemented with MRCP or ERCP to detail biliary tract anatomy and its variations. Still, even most rigorous imaging combinations may fail to reach a correct diagnosis. This case, in whom the inflamed cystic ducts were obstructed and ERCP failed to demonstrate the lumens, is a typical example to aforementioned situation.
Radiological diagnosis of biliary anomalies is an important part of abdominal imaging. At daily practice, biliary anatomy may be demonstrated with widespread techniques, such as high resolution US, multislice CT and MRCP. Preoperative awareness of any variation may minimize the chance of an unexpected course during cholecystectomy, and helps to avoid any unwanted damage to the biliary tract. It also has a paramount importance in preventing the postcholecystectomy syndrome due to a retained accessory gallbladder.
I would like to express my gratitude to Ozlem Karagozler and Hakki Muammer Karakas for proof reading the article in English.
S- Editor Wang J L- Editor Kumar M E- Editor Ma WH
| 1. | Kurzweg FT, Cole PA. Triplication of the gallbladder: review of literature and report of a case. Am Surg. 1979;45:410-412. [PubMed] |
| 2. | Barnes S, Nagar H, Levine C, Santo M, Sold A, Mercer D, Kessler A. Triple gallbladder: preoperative sonographic diagnosis. J Ultrasound Med. 2004;23:1399-1402. [PubMed] |
| 3. | Roeder WJ, Mersheimer WL, Kazarian KK. Triplication of the gallbladder with cholecystitis, cholelithiasis, and papillary adenocarcinoma. Am J Surg. 1971;121:746-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 23] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Ross RJ, Sachs MD. Triplication of the gallbladder. Am J Roentgenol Radium Ther Nucl Med. 1968;104:656-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Schroeder C, Draper KR. Laparoscopic cholecystectomy for triple gallbladder. Surg Endosc. 2003;17:1322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Nanthakumaran S, King PM, Sinclair TS. Laparoscopic excision of a triple gallbladder. Surg Endosc. 2003;17:1323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |