Published online Dec 14, 2006. doi: 10.3748/wjg.v12.i46.7549
Revised: November 6, 2006
Accepted: November 14, 2006
Published online: December 14, 2006
Primary aorto-colic fistula is rarely reported in the literature. Although infrequently encountered, it is an important complication since it is usually fatal unless detected. Primary aorto-colic fistula is a spontaneous rupture of abdominal aortic aneurysm into the lumen of the adjacent colon loop. Here we report a case of primary aorto-colic fistula in a 54-year old male. The fistulated sigmoid colon was repaired by end-to-end anastomosis. Despite inotropic support, the patient died of sepsis and multiorgan failure on the first postoperative day.
- Citation: Aksoy M, Yanar H, Taviloglu K, Ertekin C, Ayalp K, Yanar F, Guloglu R, Kurtoglu M. Rupture of abdominal aortic aneurysm into sigmoid colon: A case report. World J Gastroenterol 2006; 12(46): 7549-7550
- URL: https://www.wjgnet.com/1007-9327/full/v12/i46/7549.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i46.7549
Primary aortocolic fistula is a very rare and catastrophic complication of infrarenal abdominal aortic aneurysms. The incidence of secondary aorto-enteric fistulae has increased to 1.5%-4.0% due to the increase in the frequency of aorto-iliac fistula reconstruction techniques[1]. However, the incidence of primary aorto-colic fistulae is reported to be as low as 0.69%-2.36%[2].
The most common etiology of aorto-colic fistulae is a previous aorto-iliac fistula reconstruction with a synthetic graft for abdominal aortic pathology. An abrasion of the graft or erosion of the wall of the adjacent bowel loop by the suture line may cause a connection between the lumen of both organs[2,3]. Primary aorto-colic fistula is a spontaneous rupture of abdominal aortic aneurysm into the lumen of the adjacent colon loop. Here we report a case of primary aorto-colic fistula.
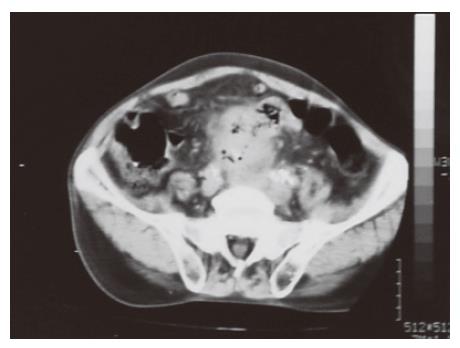
A 54-year old male was admitted to the Emergency Surgery Department of the Medical Faculty of Istanbul, Istanbul University, Turkey, with a diagnosis of an abdominal pulsatile mass. The patient suffered from hematochezia 4 d prior to admission. His past medical history did not reveal any abnormality besides heavy-smoking. During the physical examination he did not have any abdominal pain or tenderness. However, there was a pulsatile mass in the abdomen. There was blood upon rectal examination. The femoral pulses and lower extremity pulses were bilaterally palpable. The blood pressure was 90/70 mmHg, pulse rate was 112 beats/min, respiratory rate was 24 breaths/min, and the body temperature was 37.3°C. A laboratory investigation indicated hemoglobin of 7.4g/dL, hematocrit of 27%, white blood cells of 14 000/mm3, and a normal platelet count. The blood glucose was 160 mg/dL. Computed tomography (CT) scanning showed a 7 cm × 7 cm abdominal aortic aneurysm located infra-renal with gaseous images within the lumen of the aneurysm (Figure 1). Upon CT scanning, a loop of sigmoid colon was in close contact with the aorta at the level of the gaseous images. Emergency laparotomy showed a fistula between the aneurysm and the distal sigmoid colon. The aneurysm was resected and an axillo-bi-femoral bypass with ePTFE graft was carried out. In spite of inotropic support with dopamine and dobutamine, blood pressure was below 90 mmHg and a cardiac arrest (which responded to cardiopulmonary resuscitation) occurred during the operation. The fistulated sigmoid colon was repaired by end-to-end anastomosis. The patient was monitored at the Intensive Care Unit postoperatively. Despite inotropic support, the patient died of sepsis and multiorgan failure on the first postoperative day.
Primary aorto-colic fistula is seldom reported in the literature. Although rarely encountered, it is an important complication since it is usually fatal unless detected. Fistulization may occur in the jejunum, ileum, esophagus, stomach as well as colon[4-7]. Although the most frequent site of fistula is the third portion of the duodenum, a classic triad of symptoms including abdominal pain, gastrointestinal bleeding and a pulsatile abdominal mass may present in some cases regardless of the site affected[5,6]. The bleeding may be abundant or intermittent “herald” with hypotension and syncope. Our patient had a history of bleeding four days before he was admitted. However, it did not recur until the day he presented with shock at the Emergency Department. Despite the fact that certain definition of the pathogenesis of primary aorto-enteric fistulae is beyond our knowledge for the time being, mechanical erosion by aneurysms and inflammations such as diverticulitis is generally suggested to be the cause[8,9]. CT scanning and angiographies rarely demonstrate the fistula tract. However, CT scanning is of utmost importance in patients with an initial diagnosis of aorto-colic fistula. CT scanning may reveal an aortic aneurysm, deletion of the plane between the aorta and the adjacent organ, and gas in the wall or even within the lumen of the aorta as it was in this case (Figure 1).
The appropriate treatment of the entity consists of aneurysmectomy, repair of the fistula, and aortic reconstruction with synthetic grafts and omental wrapping or an extra-anatomical bypass. Aggressive antibiotic treatment is required as well to prevent an in-situ graft infection, which may be fatal[8]. The mortality rate still remains high and ranges from 30% to 75% depending on the time of surgery. The high mortality is mainly due to the sequelae of hemorrhagic shock and massive blood transfusion and sepsis. It has been stated that early death due to multisystem failure is to be expected and sepsis is an inevitable consequence of aorto-colic fistula[10].
This report emphasizes that rupture of aorto-iliac aneurysm into the sigmoid colon should be included in the differential diagnosis of lower gastrointestinal bleeding, and the high mortality of aorto-colic fistulae may be overcome with prompt diagnosis, immediate surgical intervention, and measures against sepsis. However, it may still cause death of patients in spite of all measures.
The authors express their thanks to Rebecca Plevin MS II for grammatical corrections.
S- Editor Wang GP L- Editor Wang XL E- Editor Liu WF
| 1. | Bruns C, Kristen F, Walter M. [Aortocolic fistula as a rare complication of aorto-iliac aneurysms]. Vasa. 1995;24:354-361. [PubMed] |
| 2. | Brown PW, Sailors DM, Headrick JR, Burns RP. Primary aortojejunal fistula: a case report. Am Surg. 1999;65:139-141. [PubMed] |
| 3. | Kleinman LH, Towne JB, Bernhard VM. A diagnostic and therapeutic approach to aortoenteric fistulas: clinical experience with twenty patients. Surgery. 1979;86:868-880. [PubMed] |
| 4. | Elliott JP Jr, Smith RF, Szilagyi DE. Proceedings: Aortoenteric and paraprosthetic-enteric fistulas. Problems of diagnosis and management. Arch Surg. 1974;108:479-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 139] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 5. | Berry SM, Fischer JE. Classification and pathophysiology of enterocutaneous fistulas. Surg Clin North Am. 1996;76:1009-1018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 137] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 6. | Bernhard V. Aortoenteric fistula. In Rutherford RS, editor. Vascular Surgery. 4th ed. Philadelphia: Saunders 1995; 611-618. |
| 7. | Genc FA, Taviloglu K, Dilege S, Kurtoglu M, Yilmazbayhan D. Primary aortogastric fistula. Eur J Vasc Endovasc Surg. 2000;19:669-670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Kang SJ, Kim DI, Huh SH, Lee BB, Kim DK, Do YS. Coexisting aortocolic and aortovesical fistulae in an abdominal aortic aneurysm: report of a case. Surg Today. 2003;33:441-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Kaushik SP, Cowlishaw JL. Primary aortoenteric fistula. Aust N Z J Med. 1998;28:471-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Kassum D, Kim S, Shojania AM, Kirkpatrick JR. Aortocolic fistula: a rare cause of profuse rectal bleeding. Can J Surg. 1983;26:293-295. [PubMed] |