Published online Dec 14, 2006. doi: 10.3748/wjg.v12.i46.7547
Revised: September 21, 2006
Accepted: September 28, 2006
Published online: December 14, 2006
A 67-year-old woman underwent an orthotopic liver transplantation for end stage liver disease secondary to chronic autoimmune hepatitis. She developed sudden massive hematochezia on post-operative day 23 with hemodynamic compromise. The source of hemorrhage was found at colonoscopy after careful irrigation and inspection to be a dieulafoy lesion situated just proximal to the anorectal junction. Hemostasis was achieved with epinephrine injection and thermal coagulation.
- Citation: Apiratpracha W, Ho JK, Powell JJ, Yoshida EM. Acute lower gastrointestinal bleeding from a dieulafoy lesion proximal to the anorectal junction post-orthotopic liver transplant. World J Gastroenterol 2006; 12(46): 7547-7548
- URL: https://www.wjgnet.com/1007-9327/full/v12/i46/7547.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i46.7547
A dieulafoy lesion is a submucosal ectatic arterial lesion associated with a tiny mucosal defect. It is a rare cause of profuse, but intermittent upper or lower gastrointestinal bleeding. The bleeding is often unresponsive to conservative treatment and is associated with a high mortality rate. The exact process that results in the tortuousity of the superficial artery which erodes through the mucosa and which then may bleed is unknown. Most cases have occurred in the proximal stomach. Less commonly, lesions are encountered in the small intestine, colon and rectum. Cases of rectal dieulafoy-like lesion have been reported in literature. We report a case of massive lower gastrointestinal bleeding from a dieulafoy lesion of the rectum, immediately proximal to the anorectal junction post liver transplantation that was successfully treated with injection of 1:10 000 epinephrine followed by thermal coagulation. Without careful endoscopic examination, this lesion may have been mistaken as bleeding from hemorrhoids.
A 67-year-old woman underwent a cadaveric orthotopic liver transplant for end stage liver disease secondary to chronic autoimmune hepatitis. Immunosuppression consisted of induction with basiliximab (Simulect, Novartis-Canada, Dorval QC) on post operative day 0 and day 4, delayed tacrolimus (Prograf, Astellas-Canada, Markham, ON) started on post operative day 6, mycophenolate mofetil (Cellcept, Hoffman LaRoche, Mississauga ON) and tapering doses of corticosteroids. Her post operative course was complicated and prolonged due to enterococcus faecalis septicemia, requiring intravenous vancomycin for 2 wk and disseminated varicella zoster virus reactivation which was treated with intravenous acyclovir for 10 d followed by oral valacyclovir for 3 mo to prevent recurrence.
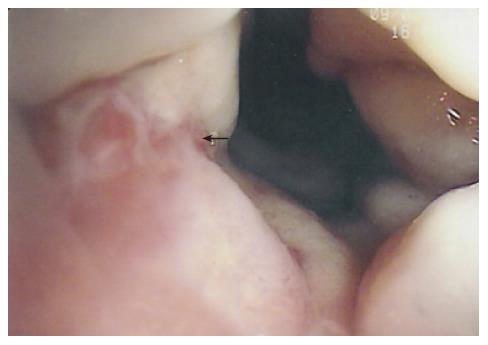
On post-operative day 23, she developed sudden massive painless lower gastrointestinal bleeding with hemodynamic compromise. Her hemoglobin level dropped from 97 g/L to 72 g/L within several hours and she required a 2 unit transfusion of packed red blood cells which raised the hemoglobin level to 99 g/L. Her liver allograft was functioning well with a normal coagulogram and her liver blood tests remained stable. She also had normal serum urea and creatinine. There was no history of constipation, abdominal pain or previous gastrointestinal bleeding but occasional diarrhea while she was in the intensive care unit. There was no history of rectal enemas use, rectal digitation, rectal tube or foreign body insertion. On examination, she was not septic, but tachycardic with heart rate of 110/min and blood pressure of 115/70 mmHg and her abdominal examination was unremarkable except for mild tenderness around the incision site. A digital rectal examination revealed the presence of fresh blood with clot and no palpable masses. An urgent colonoscopy to the terminal ileum was performed on the same day and revealed the presence of blood throughout the colon but with abundant fresh clots in the rectum. No obvious source of hemorrhage could be identified initially. After careful irrigation and inspection, a pulsatile active bleeding site was identified < 0.5 cm proximal to the anorectal junction, just above the dentate line (Figure 1). There was no obvious erosion or ulceration around the vessel and the surrounding mucosa appeared normal. Its appearance was consistent with that of a dieulafoy lesion. Hemostasis was achieved by injection with a total of 4 mL of 1:10 000 epinephrine around the bleeding lesion followed by bipolar electrocoagulation (BICAP). No further episodes of fresh bleeding were noted post-procedure. Passage of a normal brown stool was noted the following day with no further bleeding after a follow-up of 4 mo.
Dieulafoy’s lesions are uncommon but well recognized life threatening sources of gastrointestinal bleeding. The majority of lesions occur in the stomach, and most lie in the lesser curvature within 6 cm of the gastroesophageal junction[1]. The lesion ruptures spontaneously and bleeds massively for reasons that are unclear. The typical endoscopic appearance of this lesion is a single, round mucosal defect with an artery protruding from its base in the absence of surrounding ulceration. The diagnosis now primarily depends on the endoscopic visual criteria that include active arterial spurting or micropulsatile streaming from minute (< 3 mm) mucosal defects or through normal surrounding mucosa, visualization of a protruding vessel with or without active bleeding within a minute mucosal defect or through normal appearing mucosa, and fresh, densely adherent clot with a narrow point of attachment to a minute mucosal defect or to normal appearing mucosa[2,3]. Microscopic examination of the lesion reveals a small mucosal defect with minimal inflammation and a large, tortuous, thick-walled artery at the base of the defect with rupture of the artery into the lumen with fibrin thrombus in the necrotic artery loop[4,5]. Although the original descriptions and early reports were of lesions in the proximal stomach, similar lesions have subsequently been reported in the esophagus, duodenum, jejunum, colon and rectum[4,6-10]. The unique aspect of this case was the fact that the dieulafoy lesion was immediately adjacent to the anorectal junction and without careful endoscopic lavage, could have been misdiagnosed as a hemorrhoidal bleeding with potentially disastrous sequelae. Since the colonoscopic diagnosis of rectal dieulafoy-like lesion may be difficult in the presence of large amount of luminal blood and clots, we would recommend rapid colonic lavage with a polyethyleneglycol solution either orally or via nasogastric tube if oral intake is not tolerated to enable adequate visualization which is crucial in making a diagnosis. A thorough and patient endoscopic examination with lavage is also necessary.
In terms of therapy, historically surgery had been the traditional treatment of dieulafoy lesions. However, the surgical approach has been superceded by endoscopic therapy. Several endoscopic methods have been successfully used including injection of epinephrine in conjunction with coagulation therapy or the application of a Hemoclip.
In summary, rectal dieulafoy lesions are unusual sources of rectal bleeding but must be included in the differential diagnosis of profuse painless rectal bleeding, especially when other definitive lesions are not found. Endoscopic therapy is safe and effective in the treatment of rectal dieulafoy lesions.
S- Editor Wang GP L- Editor Zhu LH E- Editor Bi L
| 1. | Veldhuyzen van Zanten SJ, Bartelsman JF, Schipper ME, Tytgat GN. Recurrent massive haematemesis from Dieulafoy vascular malformations--a review of 101 cases. Gut. 1986;27:213-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 163] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 2. | Dy NM, Gostout CJ, Balm RK. Bleeding from the endoscopically-identified Dieulafoy lesion of the proximal small intestine and colon. Am J Gastroenterol. 1995;90:108-111. [PubMed] |
| 3. | Stark ME, Gostout CJ, Balm RK. Clinical features and endoscopic management of Dieulafoy's disease. Gastrointest Endosc. 1992;38:545-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 94] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Franko E, Chardavoyne R, Wise L. Massive rectal bleeding from a Dieulafoy's type ulcer of the rectum: a review of this unusual disease. Am J Gastroenterol. 1991;86:1545-1547. [PubMed] |
| 5. | Mortensen NJ, Mountford RA, Davies JD, Jeans WD. Dieulafoy's disease: a distinctive arteriovenous malformation causing massive gastric haemorrhage. Br J Surg. 1983;70:76-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 44] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Bozkurt T, Lederer PC, Lux G. Esophageal visible vessel as a cause of massive upper gastrointestinal hemorrhage. Endoscopy. 1991;23:16-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Pollack R, Lipsky H, Goldberg RI. Duodenal Dieulafoy's lesion. Gastrointest Endosc. 1993;39:820-822. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Matuchansky C, Babin P, Abadie JC, Payen J, Gasquet C, Barbier J. Jejunal bleeding from a solitary large submucosal artery. Report of two cases. Gastroenterology. 1978;75:110-113. [PubMed] |
| 9. | Richards WO, Grove-Mahoney D, Williams LF. Hemorrhage from a Dieulafoy type ulcer of the colon: a new cause of lower gastrointestinal bleeding. Am Surg. 1988;54:121-124. [PubMed] |
| 10. | Kayali Z, Sangchantr W, Matsumoto B. Lower gastrointestinal bleeding secondary to Dieulafoy-like lesion of the rectum. J Clin Gastroenterol. 2000;30:328-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |