Published online Jan 28, 2006. doi: 10.3748/wjg.v12.i4.553
Revised: July 19, 2005
Accepted: August 26, 2005
Published online: January 28, 2006
AIM: To determine the distance between the branching point of the left colic artery (LCA) and the inferior mesenteric artery (IMA) by computed tomography (CT) scanning, for preoperative evaluation before laparoscopic colorectal operation.
METHODS: From February 2004 to May 2005, 100 patients (63 men, 37 women) underwent angiography performed with a 16-scanner multi-detector row CT unit (Toshiba, Aquilion 16). All images were analyzed on a workstation (AZE Ltd, Virtual Place Advance 300). The distance from the root of the IMA to the bifurcation of the LCA was measured by curved multi-planar reconstruction on a workstation.
RESULTS: The IMA could be visualized in all the cases, but the LCA was missing in two patients. The mean distance from the root of the IMA to the root of the LCA was 42.0 mm (range, 23.2-75.0 mm). There were no differences in gender, arterial branching types, body weight, height, and body mass index.
CONCLUSION: Volume-rendered 3D-CT is helpful to assess the vascular branching anatomy for laparoscopic surgery.
- Citation: Kobayashi M, Morishita S, Okabayashi T, Miyatake K, Okamoto K, Namikawa T, Ogawa Y, Araki K. Preoperative assessment of vascular anatomy of inferior mesenteric artery by volume-rendered 3D-CT for laparoscopic lymph node dissection with left colic artery preservation in lower sigmoid and rectal cancer. World J Gastroenterol 2006; 12(4): 553-555
- URL: https://www.wjgnet.com/1007-9327/full/v12/i4/553.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i4.553
Laparoscopy-assisted colorectal surgery is now an important surgical modality for colorectal neoplasms. For left side colon cancer, the root of the inferior mesenteric artery (IMA) is usually cut for D3 lymph node dissection. We keep the left colic artery (LCA) intact even in D3 dissection, to maintain the blood supply of the preserved proximal sigmoid colon (manuscript submitted for publication). However, it is at times difficult to locate the root of the LCA when dissecting around the IMA.
Helical computed tomography (CT) and multi-detector CT produce an image of the mesenteric vasculature with faster scanning and narrower collimation[1] than that previously obtained by conventional angiography. Recently, three-dimensional (3D) angiography was shown to help the preoperative assessment of vascular anatomy for laparoscopic lymph node dissection. In this study, we have used preoperative 3D-CT to investigate the vascular anatomy of the IMA for laparoscopic lymph node dissection around IMA with the preservation of LCA, for rectal cancer.
One hundred patients (63 men, 37 women) who underwent contrast-enhanced CT from February 2004 to May 2005 were included (Table 1).
| Medical conditions | n |
| Aortic aneurysm | 32 |
| Arteriosclerosis | 26 |
| Varicose veins | 5 |
| Takayasu’s arteritis | 3 |
| Angina pectoris | 1 |
| Myocardial infarction | 1 |
| Cerebral infarction | 1 |
| Hypertension | 1 |
| Thrombosis | 4 |
| Total cardiovascular disease | 74 |
| Colon cancer | 9 |
| Hepatocellular carcinoma | 5 |
| Pancreatic cancer | 3 |
| Malignant lymphoma | 2 |
| Esophageal cancer | 1 |
| Total neoplasm | 20 |
| Myoma uteri | 3 |
| Pancreatic cyst | 2 |
| Cholecystolithiasis | 1 |
| Total others | 6 |
Multi-detector row CT angiography was performed in all the patients with 16-detector row scanners (Toshiba, Aquilion 16). Patients received 2 mL/kg (not exceeding 150 mL in total) of nonionic contrast medium (300 g/L) injected at a rate of 3 mL/s through a cubital vein, using an 18-22-gauge catheter and a power injector. Scanning was initiated by an automatic bolus-tracking system. The circular region of interest was placed in the abdominal aorta. The threshold level was 100 Hounsfield units. The CT scan parameters were collimation 16 mm×1 mm, helical pitch 23. Images were reconstructed at 1-2 mm thickness. All images were analyzed on a workstation (AZE Ltd, Virtual Place Advance 300). The 3D-volume rendering and curved multi-planar reconstruction were done on a workstation by two radiologists. The length from the root of IMA to bifurcation of LCA was measured by curved multi-planar reconstruction.
Chi-square test was applied to analyze the differences in incidence of the types of branching of LCA, sigmoidal artery (SA), and SRA. Pearson’s product moment test was used to estimate correlation between the distance from the root of IMA to LCA and body weight, height, and body mass index (BMI), respectively.
There was no age difference between male (mean, 68.7 years; range, 30-89 years) and female (mean 67.5 years; range, 20-90 years) patients; the mean overall age was 68.3 years (range, 20-90 years). The IMA was observed on 3D-CT in all the patients analyzed. In two patients, 3D-CT demonstrated that the LCA was missing. The mean distance from the root of IMA to the root of LCA for all cases was 42.0 (range, 23.2-75.0) mm; gender differences were not observed [41.8 (range, 25.3-73.5) mm for male patients vs 42.3 (range, 23.2-75.0) mm for female patients].
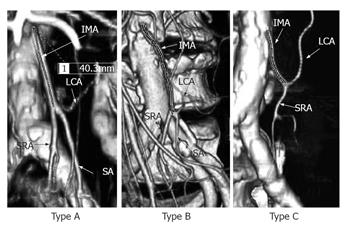
The branching of LCA, SA, and SRA could be determined in 82 cases (Table 2). Three types of branching were seen (Figure 1): Type A, where the three arteries branch off from the same point (10 cases: 6 males, 4 females); Type B, where SA branches off from LCA (45 cases: 28 males, 17 females); and Type C, where SA branches off from SRA (27 cases: 21 males; 6 females). There was no significant difference in the type of branching between male and female patients (P = 0.293; Table 2). The distances from IMA root to LCA root (43.1 ± 9.2 mm, n = 82) in Types A, B, and C were 44.1 ± 7.4 mm, 42.2 ± 10.2 mm, and 38.7 ± 7.4 mm, respectively. The distance in Type C was apparently shorter than in Type A, (P = 0.07), and there was no significant difference between the three types (Table 3).
| Sex | n | Age (range)/yr | Distance(range)/min | 98 patients withbranching type | |||
| A | B | C | D | ||||
| Male | 63 | 68.7 (30-89) | 41.8 (25.3–73.5) | 6 | 28 | 21 | 7 |
| Female | 37 | 67.5 (20-90) | 42.3 (23.2–75.0) | 4 | 17 | 6 | 9 |
| Total | 100 | 68.3 (20-90) | 42.0 (23.2–75.0) | 10 | 45 | 27 | 16 |
| Branching type | Mean distance (mm) (SD) |
| Type A | 44.1 (7.36) |
| Type B | 42.2 (10.2) |
| Type C | 38.3 (7.41) |
| All (n = 82) | 41.3 (9.15) |
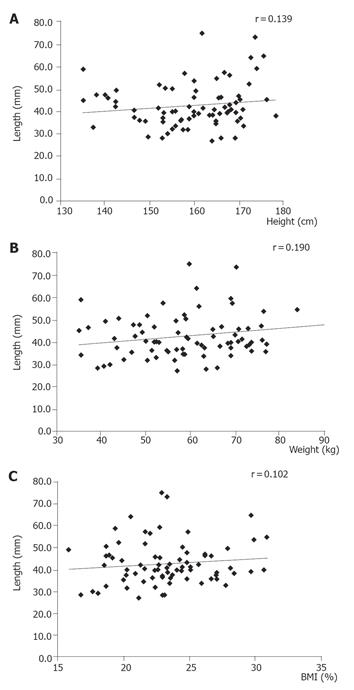
The distance from IMA root to LCA root was examined in relation with height and body weight measured in 76 and 77 patients, respectively. There was no correlation between this distance and height (r = 0.139, Figure 2A), body weight (r = 0.190, Figure 2B), or BMI (r = 0.102, Figure 2C).
Recent advances in multi-detector row CT combined with rapid intravenous administration of contrast material have allowed excellent opacification of the mesenteric vessels. Attempts have been made to use this modality to obtain preoperative information on mesenteric vasculatures[2-4]. The blood supply and lymphatic system of the colon are simple compared with those of the stomach. Accordingly, D3 lymph node dissection for sigmoid and rectal cancer is performed by cutting the root of the IMA. In contrast, for gastric cancer, the lymph nodes around the common hepatic artery, celiac axis, and splenic artery, most of which are group 2 lymph nodes, should be dissected while preserving these major vessels. We have reported a D3 lymph node dissection technique around IMA for lower sigmoid colon or rectal cancer cases, whereby the LCA is kept intact to maintain the blood supply of the preserved proximal sigmoid colon (manuscript submitted for publication). LCA is absent in 12% of individuals, in whom the colosigmoid artery performs its function[5,6]. In some cases, the length from the root of IMA to that of LCA is fairly long and lymph node dissection around the IMA can be a stressful procedure until the LCA is located, particularly in laparoscopic surgery. To help in locating the LCA during laparoscopic surgery, we have conducted a preoperative 3D-CT investigation to examine the branching of LCA, SA, and SRA, and evaluate the distance from the root of IMA to that of LCA.
In our study, there were no gender differences in mean distance and distance ranges. There was also no correlation between body weight, height, or BMI and the distance from IMA root to LCA root. In branching Type C, the distance from IMA root to LCA root tended to be shorter, but this was not statistically significant. Thus, the distance between IMA root and LCA root is independent of the type of branching or the patient’s constitution. However, volume-rendered 3D-CT helped identify vascular branching types for laparoscopic surgery and indicated that the distance of the branching point of the LCA from the IMA root may range from as short as 20 mm to sometimes longer than 70 mm.
S- Editor Guo SY and Pan BR L- Editor Elsevier HK E- Editor Bi L
| 1. | Horton KM, Fishman EK. Volume-rendered 3D CT of the mesenteric vasculature: normal anatomy, anatomic variants, and pathologic conditions. Radiographics. 2002;22:161-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 77] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 2. | Winter TC 3rd, Freeny PC, Nghiem HV, Hommeyer SC, Barr D, Croghan AM, Coldwell DM, Althaus SJ, Mack LA. Hepatic arterial anatomy in transplantation candidates: evaluation with three-dimensional CT arteriography. Radiology. 1995;195:363-370. [PubMed] |
| 3. | Smith PA, Klein AS, Heath DG, Chavin K, Fishman EK. Dual-phase spiral CT angiography with volumetric 3D rendering for preoperative liver transplant evaluation: preliminary observations. J Comput Assist Tomogr. 1998;22:868-874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Ohtani H, Kawajiri H, Arimoto Y, Ohno K, Fujimoto Y, Oba H, Adachi K, Hirano M, Terakawa S, Tsubakimoto M. Efficacy of multislice computed tomography for gastroenteric and hepatic surgeries. World J Gastroenterol. 2005;11:1532-1534. [PubMed] |
| 5. | Kornblith PL, Boley SJ, Whitehouse BS. Anatomy of the splanchnic circulation. Surg Clin North Am. 1992;72:1-30. [PubMed] |
| 6. | Rosenblum JD, Boyle CM, Schwartz LB. The mesenteric circulation. Anatomy and physiology. Surg Clin North Am. 1997;77:289-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 120] [Article Influence: 4.3] [Reference Citation Analysis (0)] |