Published online Aug 21, 2006. doi: 10.3748/wjg.v12.i31.5094
Revised: May 16, 2006
Accepted: May 22, 2006
Published online: August 21, 2006
Oxidized low density lipoprotein (ox-LDL) molecule is one of the most important modified lipoproteins produced during the oxidative stress. Modified lipoproteins have been defined as being part of the immune inflammatory mechanisms in association with oxidant stress. We have reported the accumulation of ox-LDL in Balb/c mice liver after bile duct ligation previously. Here, we investigated this finding in human beings with obstructive jaundice. Our study demonstrates that obstructive jaundice results in tremendous accumulation of ox-LDL in the liver tissue of patients.
- Citation: Comert M, Ustundag Y, Tekin IO, Gun BD, Barut F. Obstructive jaundice leads to accumulation of oxidized low density lipoprotein in human liver tissue. World J Gastroenterol 2006; 12(31): 5094-5095
- URL: https://www.wjgnet.com/1007-9327/full/v12/i31/5094.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i31.5094
Oxidized low density lipoprotein (ox-LDL) molecule is one of the most important modified lipoproteins. Its popularity has arisen after our understanding about its key role in the pathogenesis of atherosclerosis[1]. These molecules have been defined as being part of the immune inflammatory mechanisms in association with oxidant stress[2]. Hepatocyte injury during obstructive jaundice is involved in such pathways associated with oxidant stress. This association has been testified also by us in Balb/c mice. Moreover, our study demonstrated that tremendous ox-LDL is accumulated in the liver after bile duct ligation in mice[3]. Furthermore, we have investigated this finding in human beings with obstructive jaundice.
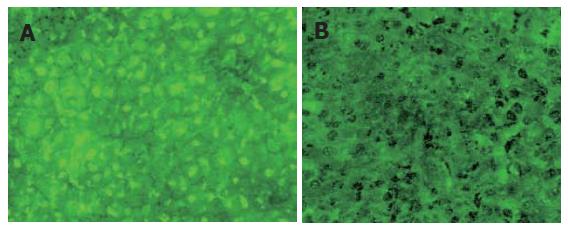
The study was composed of two groups. One group enrolled 11 patients with various causes of obstructive jaundice, 5 percutaneous and 6 intraoperative wedge-resection liver biopsies were taken from these patients. The other group included 7 patients undergoing elective abdominal operations without primary hepatobiliary pathologies. Wedge-resection type liver biopsies were taken from all these patients. Routine liver biochemical parameters including cholestatic liver enzymes were studied. In liver biopsies stained with hematoxylin and eosin, we investigated cholestatic findings. Moreover, a special immunofluorescent staining was done for investigation of ox-LDL in the liver tissue by fluorescent microscopy. All patients in group 1 demonstrated various degrees of cholestasis. The patients in group 2 showed neither cholestasis nor any histopathologic abnormality in the liver biopsy samples. First anti-ox-LDL antibody and fluorescence - stained anti-anti ox-LDL antibody were applied on liver tissue samples as previously described[3]. The patients in group 1 were found to have enormous accumulation of ox-LDL in the liver (Figure 1A). No patient in group 2 demonstrated ox-LDL deposition (Figure 1B).
In this investigation, we clearly demonstrated retention of ox-LDL molecules in the liver tissue of human beings with obstructive jaundice, which was also found in our mice study. As demonstrated in our mice study, enhanced lipid peroxidation in the liver due to oxidative stress in association with obstructive jaundice has been clearly notified by many authors[4,5]. A major and early lipid peroxidation product is ox-LDL which is mainly filtered by liver macrophages and Kupffer cells[6]. During the jaundice period after biliary obstruction, ox-LDL accumulates in the liver either because of its decreased secretion into the bile or because of enhanced production due to lipid peroxidation as the filtration capacity of Kupffer cells becomes insufficient. It is well known that ox-LDL molecules have specific receptors on hepatocytes, Kupffer and stellate cells[2,7]. The interaction of ox-LDL with these cells can lead to apoptosis of hepatocytes, enhancement of tumor necrosis factor-alpha and secretion of transforming growth factor-beta by Kupffer cells, as well as transformation of stellate cells into collagen secreting myofibroblasts[2,7,8]. Thus, it seems theoretically possible that the main lipid peroxidation byproduct, ox-LDL, may have important roles in liver consequences of biliary jaundice. Our study results indicate a concrete fact that ox-LDL accumulates in human liver tissue during obstructive jaundice. Nevertheless, further investigation should be done for more detailed analysis of such accumulation and its role in liver outcomes of obstructive jaundice.
S- Editor Pan BR L- Editor Wang XL E- Editor Bi L
| 1. | Tsimikas S, Witztum JL. The oxidative modification hypothesis of atherosclerosis. Oxidative stress and vascular disease. Boston: Kluwer Acad Pub 2000; 49-74. [RCA] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Hsu HY, Chiu SL, Wen MH, Chen KY, Hua KF. Ligands of macrophage scavenger receptor induce cytokine expression via differential modulation of protein kinase signaling pathways. J Biol Chem. 2001;276:28719-28730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 137] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 3. | Cömert M, Tekin IO, Acikgöz S, Ustündağ Y, Uçan BH, Acun Z, Barut F, Sümbüloğlu V. Experimental bile-duct ligation resulted in accumulation of oxidized low-density lipoproteins in BALB/c mice liver. J Gastroenterol Hepatol. 2004;19:1052-1057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | López PM, Fiñana IT, De Agueda MC, Sánchez EC, Muñoz MC, Alvarez JP, De La Torre Lozano EJ. Protective effect of melatonin against oxidative stress induced by ligature of extra-hepatic biliary duct in rats: comparison with the effect of S-adenosyl-L-methionine. J Pineal Res. 2000;28:143-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Nakano H, Fujiwara Y, Kitamura N, Kumada K, Matsumiya A, Sakai H, Hatakeyama T, Yamaguchi M, Jaeck D. Susceptibility to lipopolysaccharide of cholestatic rat liver produced with bile duct ligation: assessments of the mitochondrial glutathione pool and the effects of N-acetylcysteine. Eur Surg Res. 2000;32:148-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Pieters MN, Esbach S, Schouten D, Brouwer A, Knook DL, Van Berkel TJ. Cholesteryl esters from oxidized low-density lipoproteins are in vivo rapidly hydrolyzed in rat Kupffer cells and transported to liver parenchymal cells and bile. Hepatology. 1994;19:1459-1467. [PubMed] |
| 7. | Schneiderhan W, Schmid-Kotsas A, Zhao J, Grünert A, Nüssler A, Weidenbach H, Menke A, Schmid RM, Adler G, Bachem MG. Oxidized low-density lipoproteins bind to the scavenger receptor, CD36, of hepatic stellate cells and stimulate extracellular matrix synthesis. Hepatology. 2001;34:729-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 67] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Feng Y, Schreiner GF, Chakravarty S, Liu DY, Joly AH. Inhibition of the mitogen activated protein kinase, p38 alpha, prevents proinflammatory cytokine induction by human adherent mononuclear leukocytes in response to lipid loading. Atherosclerosis. 2001;158:331-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |