Published online Jul 14, 2006. doi: 10.3748/wjg.v12.i26.4250
Revised: February 21, 2006
Accepted: February 28, 2006
Published online: July 14, 2006
Von Meyenburg complexes are benign liver lesions consisting of adenomatous bile duct proliferates. We present two patients suffering from esophageal cancer accompanied by the occurrence of von Meyenburg complexes. Preoperative computerized tomography (CT) of the liver had not shown these lesions. In one of the patients, diffuse nodular manifestation was found in both liver lobes, mimicking diffuse hepatic metastases. Intraoperative frozen section revealed the benign nature of the lesions in both cases. The patients underwent esophageal resection without complications. To the best of our knowledge, the coincidence of von Meyenburg complexes and esophageal cancer has never been reported before. This uncommon entity should be taken into consideration as a differential diagnosis of liver lesions in malignancies. It underlines the importance of intraoperative frozen section for liver lesions of unknown origin.
- Citation: Fritz S, Hackert T, Blaker H, Hartwig W, Schneider L, Buchler MW, Werner J. Multiple von Meyenburg complexes mimicking diffuse liver metastases from esophageal squamous cell carcinoma. World J Gastroenterol 2006; 12(26): 4250-4252
- URL: https://www.wjgnet.com/1007-9327/full/v12/i26/4250.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i26.4250
Von Meyenburg complexes are benign liver lesions consisting of dilated bile duct structures with a surrounding fibrous stroma. Their incidence is age-dependent and they are observed about 1% in children and 5%-6% in adults[1]. Usually, these lesions do not have any pathological value and are incidental findings in asymptomatic patients[1]. However, a malignant transformation and association with cholangiocarcinomas have been discussed, but not yet proven[2,3]. As von Meyenburg complexes are small lesions, they are usually not detected on radiological examinations, including ultrasound, CT and magnetic resonance imaging (MRI)[4-7].
We present herein two cases of preoperatively undetected von Meyenburg complexes associated with primary esophageal cancer and review the present literature concerning these lesions.
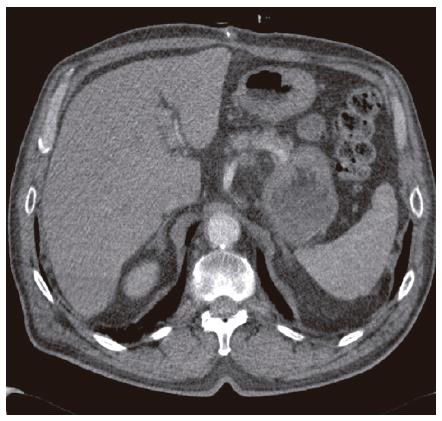
Patient 1 is a 66-year-old male suffering from an esophageal squamous cell carcinoma. Preoperatively, distant metastases were excluded by abdominal ultrasound, chest X-ray and high resolution CT-imaging of the thorax and liver (Figure 1). Surgical therapy with abdomino-thoracic resection of the esophagus was indicated.
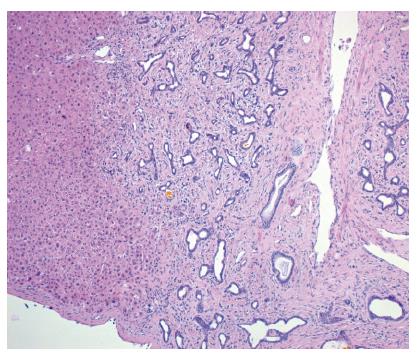
Intraoperatively, abdominal exploration revealed multiple white nodular lesions in both lobes of the liver. With a diameter of 2-3 mm, they had the macroscopic aspect of diffuse liver metastases (Figure 2). To confirm the diagnosis of metastases, which would have excluded the patient from further curative resection of the primary esophageal carcinoma, a frozen section was performed. Surprisingly, histology showed benign microhamartomas, so-called von Meyenburg complexes (Figure 3). Because of the benign nature of the lesions, esophageal resection was performed as planned. The postoperative course was uneventful, liver function was normal and the patient recovered quickly.
Patient 2 is a 47-year-old male also suffering from an esophageal squamous cell carcinoma. Comparable to patient 1, the preoperative liver CT scan showed no pathological findings except for liver steatosis and a small cyst in segment IV/VIII.
Intraoperatively, we additionally found a suspicious liver lesion of 5 mm size in segment III. In contrast to the case described above, this was a solitary lesion, with the macroscopic aspect of a metastasis. However, frozen section revealed a sclerotic von Meyenburg complex. Consequently, the operation was performed as planned. No further complications occurred in the postoperative course.
Esophageal cancer is an important cause of cancer death, with an incidence of about 8-10/100 000 and 13 300 deaths in the United States in 2004[8]. About 35% of all patients already suffer from liver metastasis by the time of diagnosis of the primary tumor. Since patients are excluded from potentially curative resection of the tumor when metastases are present, the diagnosis of liver metastases plays a crucial role for further treatment. The prognosis of these patients is also highly dependant on the respectability of the tumor.
Distant metastases, especially liver metastasis, can be diagnosed by CT scan or MRI with high sensitivity and specificity[6]. Sensitivities of these diagnostic means range between 74% and 85%[9]. In these series, almost all false-negative results occurred when lesions were less than 1.5 cm in diameter. Therefore, non-invasive detection of small metastases can be difficult or even impossible.
When suspicious lesions are found by CT scan, further differentiation is possible by additional MRI imaging[5]. Differential diagnosis of liver metastases includes benign liver lesions, including hemangiomas, adenomas, von Meyenburg complexes or infectious lesions e.g. miliary tuberculosis[5].
Bile duct hamartomas (von Meyenburg complexes) of the liver are usually detected during laparotomy or autopsy as an incidental finding. Multilocular occurrence is possible although they are rarely spread throughout the whole liver, as it was observed in our first patient. They may be found in normal liver tissue, but also in association with Caroli’s syndrome, congenital hepatic fibrosis (CHF) or autosomal dominant polycystic kindney disease (ADPKD)[10]. Histology of von Meyenburg complexes consists of a variable number of dilated small bile ducts, embedded in a fibrous, sometimes hyalinizing stroma (Figure 3).
If detected by CT scan or MRI, von Meyenburg complexes appear as small intrahepatic cystoid lesions. The lesions are frequently located adjacent to the portal veins, although the lesions can also be located everywhere else[5]. However, it remains difficult to differentiate between metastases and benign liver lesions. Moreover, small liver lesions with a diameter of less than 1.5 cm are often not detected by CT or MRI[9].
Since the treatment of metastatic disease is completely different from resectable esophageal cancer, liver lesions need to be identified and characterized as early as possible. In our presented patients, the preoperative staging did not reveal any liver metastases. This underlines the importance of exact diagnostic measures in cases of unexpected intraoperative findings. Besides intraoperative ultrasound of the liver, frozen section is the gold standard for further differentiation of liver lesions of unknown origin.
Von Meyenburg complexes are defined as innocuous lesions. However, there are about 10 reported cases of neoplastic transformation of von Meyenburg complexes resulting in cholangiocarcinomas[2,3].
In conclusion, von Meyenburg complexes are an important differential diagnosis of hepatic metastases. As the existence of liver metastases is crucial for therapeutic decision making in malignant diseases, this differential diagnosis must be carefully clarified. Since von Meyenburg complexes are usually less than 5 mm in size, they can escape preoperative radiologic diagnostics. The macroscopic appearance of von Meyenburg complexes can mimic liver metastasis as demonstrated in our reported patients. This underlines the importance of intraoperative frozen sections to make the correct diagnosis.
S- Editor Wang J L- Editor Kumar M E- Editor Liu Y
| 1. | Redston MS, Wanless IR. The hepatic von Meyenburg complex: prevalence and association with hepatic and renal cysts among 2843 autopsies [corrected]. Mod Pathol. 1996;9:233-237. [PubMed] |
| 2. | Röcken C, Pross M, Brucks U, Ridwelski K, Roessner A. Cholangiocarcinoma occurring in a liver with multiple bile duct hamartomas (von Meyenburg complexes). Arch Pathol Lab Med. 2000;124:1704-1706. [PubMed] |
| 3. | Jain D, Sarode VR, Abdul-Karim FW, Homer R, Robert ME. Evidence for the neoplastic transformation of Von-Meyenburg complexes. Am J Surg Pathol. 2000;24:1131-1139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 67] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Mortelé B, Mortelé K, Seynaeve P, Vandevelde D, Kunnen M, Ros PR. Hepatic bile duct hamartomas (von Meyenburg Complexes): MR and MR cholangiography findings. J Comput Assist Tomogr. 2002;26:438-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 58] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Luo TY, Itai Y, Eguchi N, Kurosaki Y, Onaya H, Ahmadi Y, Niitsu M, Tsunoda HS. Von Meyenburg complexes of the liver: imaging findings. J Comput Assist Tomogr. 1998;22:372-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 27] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 6. | Pokieser P, Memarsadeghi M, Danzer M, Prokesch R, Partik B, Wenzl E. [Staging of carcinomas of the upper gastrointestinal tract. The current status of diagnostic imaging]. Radiologe. 1999;39:555-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Maher MM, Dervan P, Keogh B, Murray JG. Bile duct hamartomas (von Meyenburg complexes): value of MR imaging in diagnosis. Abdom Imaging. 1999;24:171-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Jemal A, Tiwari RC, Murray T, Ghafoor A, Samuels A, Ward E, Feuer EJ, Thun MJ. Cancer statistics, 2004. CA Cancer J Clin. 2004;54:8-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3094] [Cited by in RCA: 2973] [Article Influence: 141.6] [Reference Citation Analysis (0)] |
| 9. | Haider MA, Amitai MM, Rappaport DC, O'Malley ME, Hanbidge AE, Redston M, Lockwood GA, Gallinger S. Multi-detector row helical CT in preoperative assessment of small (< or = 1.5 cm) liver metastases: is thinner collimation better. Radiology. 2002;225:137-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 89] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 10. | Leuven KU, Desmet VJ. Pathogenesis of ductal plate malformation. J Gastroenterol Hepatol. 2004;19:356-360. [DOI] [Full Text] |