INTRODUCTION
Primary biliary cirrhosis (PBC) is a chronic cholestatic liver disease associated with a variety of other conditions, including Sjögren’s syndrome, Hashimoto’s thyroiditis, scleroderma or other components of CREST syndrome, and inflammatory arthritis [1,2], but its association with Behçet’s disease (BD) is very rare, and so is its association with palmoplantar pustulosis (PPP) [3]. We report the first case of PBC associated with BD and PPP, and discuss the relationship among these three diseases in terms of the environmental factors, such as infectious agents, described in the literature.
CASE REPORT
A 37-year-old woman suffered from uveitis in 1991. In 2000, she was diagnosed with palmoplantar pustulosis (PPP) at the Department of Dermatology, Fukushima Medical University Hospital, and was treated with ointment. However, liver dysfunction developed, and she was referred to our department in March 2003 at the age of 49 years.
At our first medical examination, she complained of no symptoms involving the oral mucosa or extremities except the lesion of pustulosis. Blood pressure was normal, and there was no history of diabetes mellitus or hyperlipidemia. Laboratory data showed liver dysfunction with elevated levels of AST (149 IU/L), ALT (340 IU/L), ALP (428 IU/L; normal, 125-335 IU/l), GGT (228 IU/L; normal, 6-30 IU/l), T-Bil (0.7 mg/dL) and IgM (130 mg/dL; normal, 52-270 mg/dL). The titer of anti-mitochondrial autoantibodies (AMA) was 1:20, and the index of AMA-M2 antibody was 32 (normal, <7). Results of hepatitis B and C serologic tests were negative. After one month, subarachnoid hemorrhage occurred owing to the bursting of a cerebral artery aneurysm. An emergency brain operation was performed, revealing four cerebral artery aneurysms including the ruptured one (Figure 1), which were clipped successfully. Her hospital course was otherwise uneventful, and her slight cerebral signs resolved within days of the operation, and she was discharged from the hospital, neurologically intact. Liver biopsy was, therefore, postponed. PBC associated with PPP was diagnosed on the basis of clinical findings based on ‘Criteria for Diagnosis of PBC in Japan’ by the Study Group for Autoimmune Hepatitis, a subdivision of the Research Group for Intractable Hepatitis, sponsored by the Ministry of Health and Welfare of Japan [4]. Liver function normalized within three months of the start of treatment with ursodesoxycholic acid (UDCA) (600 mg/d).
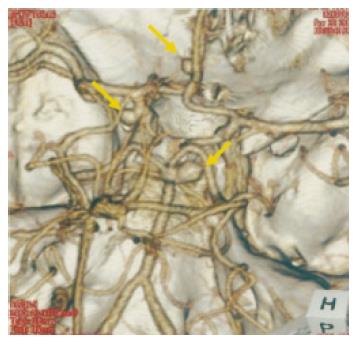
Figure 1 Computed tomographic angiography shows aneurysms of the left.
internal carotid-posterior communicating artery, left. anterior communicating artery, and right. posterior cerebral artery (arrows).
Erythema appeared in the lower extremities in July 2004 (Figure 2). Oral aphthous ulcers were sometimes noted, too. Lymphadenopathy was not recognized. No abnormal findings were noted in the chest or abdomen. Laboratory data at the time were as follows: increased level of CRP, 3.1mg/dL (normal, <0.3) and ESR, 73mm/h (normal, 3-15); WBC, 9 400/mm3, (normal, 2800-8800). Liver function and renal function were normal. HLA typing was positive for A2, A30 (19), B54 (22), B51 (5), Cw1 and DR9. Because HLA B51 was positive, a skin biopsy of the erythema was performed. Histological examination showed erythema nodosum characterized by a neutrophilic inflammatory infiltrate involving the septa of the subcutaneous tissue. Incomplete type Behçet’s disease (BD) was diagnosed on the basis of recurrent oral aphthous ulcers, erythema nodosum, and past history of uveitis according to the diagnostic criteria from the Behçet’s Disease Research Committee of Japan (1987 revision)[4]. A non-steroidal anti-inflammatory drug was administered orally as palliative treatment, and erythema nodosum resolved.
Figure 2 Typical eruption of erythema nodosum shows erythematous nodules on the anterior aspect of the leg.
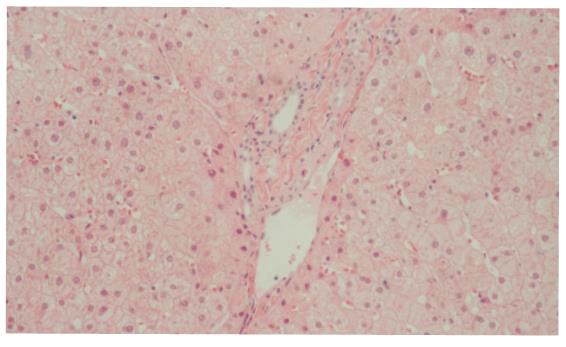
Liver biopsy was performed in January 2005, but histological examination did not show typical chronic nonsuppurative destructive cholangitis (CNSDC) (Figure 3) because liver function was improved by 2-year UDCA treatment.
Figure 3 Liver biopsy specimen shows slightly enlarged portal tracts with no evidence of chronic nonsuppurative destructive cholangitis.
Hematoxylin and eosin, original magnification ×100.
DISCUSSION
BD is a well-known multisystem inflammatory disorder of unknown etiology that is characterized by oral and genital ulcers, uveitis, and a variety of other manifestations, such as erythema nodosum, polyarthritis, thrombophebitis, and ulceration of the intestinal mucosa [6]. Involvement of the liver is less common; however, systemic amyloidosis and Budd-Chiari syndrome have been documented [7,8]. Susceptibility to BD is associated with the HLA B51 allele.
There have been only a few cases of PBC associated with BD [9]. In the present case, the clinical manifestations of BD were oral aphtha, erythema nodosum and uveitis, and there was no genital ulcer or intestinal involvement. However, it is possible that the intracranial aneurysms were related to BD. Cerebral artery aneurysms in patients with BD are uncommon, but there are 14 cases reported in the literature [10]. These cases are quite similar to ours in which the aneurysms are multiple. Furthermore, in our case there was no risk factor that would produce a cerebral vessel event: hypertension, hyperlipidemia, or diabetes mellitus. Some BD case reports describe the efficacy of steroid therapy for multiple nonruptured cerebral artery aneurysms [11-13]. Kerr et al, however, report a patient with BD who developed multiple aneurysms and subarachnoid hemorrahge in rapid succession under steroid therapy [14]. In our patient, follow-up brain computed tomographic angiography was performed after surgical treatment, but no aneurysms were detected.
PBC is an autoimmune liver disease characterized by the occurrence of AMA. Clinically, PBC is associated with a large variety of other diseases, such as arthropathy, CREST syndrome, and autoimmune thyroiditis [15]. To our knowledge, however, no report has ever described the simultaneous development of three autoimmunological diseases, PBC, BD, and PPP.
This is the first case report of PBC complicated by BD and PPP, which is a localized type of psoriasis. Although psoriasis is characterized by proliferation of the epidermis, the immune system plays a prominent role in its development [16]. Interaction between keratinocytes and T cells is involved in the pathogenesis, just as interaction between biliary epithelial cells and T cells is in the pathogenesis of PBC. In BD, lymphocytic infiltration is observed around the arteries. Moreover, some workers suggested that some microbial antigen is closely associated with the development of these three diseases [17-19].
Memory T cells specific to these bacterial antigens may be activated by antigens on the arteries, skin or liver. We believe that patients with PBC associated with BD and PPP hold the key to clarifying the nature of these diseases.
S- Editor Wang J L- Editor Zhang JZ E- Editor Zhang Y