Published online Mar 21, 2006. doi: 10.3748/wjg.v12.i11.1782
Revised: August 15, 2005
Accepted: August 26, 2005
Published online: March 21, 2006
Acute biliary pancreatitis (ABP) is rare in childhood and endoscopic sphincterotomy should be avoided in the child due to the risk of both early and late complications but, when necessary, the optimal timing between endoscopic procedure and cholecystectomy is still uncertain. A nine years old child with acute biliary pancreatitis underwent successfull laparo-endoscopic “Rendez-Vous” procedure in which endoscopic drainage of the common bile duct and laparoscopic cholecystectomy were performed simultaneously. This is the first case reported of laparo-endoscopic Rendez-Vous in a child. The excellent outcome of this patient and the review of the literature concerning other available options for the treatment of such cases suggest that this procedure offers great advantages, especially in children, of reducing the required number of treatments, the risk of ineffectiveness, the number of anaesthesia, the length of hospital stay and the risk of iatrogenic morbidity.
- Citation: Greca GL, Blasi MD, Barbagallo F, Stefano MD, Latteri S, Russello D. Acute biliary pancreatitis and cholecystolithiasis in a child: One time treatment with laparoendoscopic “Rendez-vous” procedure. World J Gastroenterol 2006; 12(11): 1782-1785
- URL: https://www.wjgnet.com/1007-9327/full/v12/i11/1782.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i11.1782
Acute biliary pancreatitis (ABP) is rare in childhood and endoscopic sphincterotomy should be avoided in the child due to the risk of both early and late complications but, when necessary, the optimal timing between endoscopic procedure and cholecystectomy is still uncertain. In the child the literature concerning therapeutic ERCP with ES for ABP is scarce, and ERCP, combined with ES or not, carries also the well known risk of iatrogenic acute pancreatitis. The optimal diagnostic and therapeutic approach and the timing of the procedures in children with cholecystolithiasis will often depend on the level of expertise of both the biliary endoscopist and laparoscopist. A nine years old child with acute biliary pancreatitis underwent the first successfull laparo-endoscopic “Rendez-Vous” procedure in which endoscopic drainage of the common bile duct and laparoscopic cholecystectomy were performed simultaneously. The favourable outcome of the reported case led us to deepen this issue.
A nine-year-old girl, weighing 52 kilograms, BMI of 27, was urgently admitted to our department because of pain in the right upper abdomen associated with vomiting. The only abnormal laboratory tests were the serum ALT 163 u/L (normal value 10-55), amylase 131 U/L (normal value < 110), lipase 482 U/L (normal value < 300), and ALP 168 U/L (normal value 38-126). Abdominal ultrasonography revealed multiple gallstones (3-5 millimeter) and sludge in the gallbladder and a normal common bile duct (CBD). The patient was kept NPO with intravenous fluids and analgesics and was discharged from the hospital after being asymptomatic for 24 h against medical advice, because her parents refused laparoscopic cholecystectomy (LC). The patient was followed in the paediatric outpatient clinic where metabolic or haematologic causes of cholecystolithiasis were excluded.
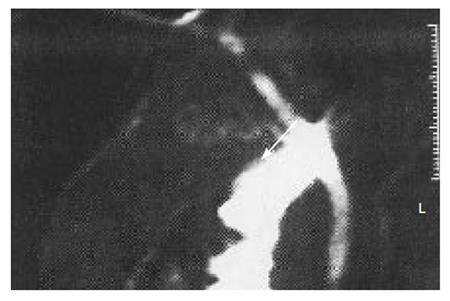
Three weeks later the patient was again urgently admitted because of a recurrence of abdominal pain, vomiting and a fever (38.6°C). Ultrasonography showed gallstones, a dilated CBD (8 mm) and pancreatic edema. Laboratory test showed a nine fold increased serum amylase of 998 U/L and of serum lipase 2430 U/L. Total and direct bilirubin were both increased to 2.81 mg/dl and 1.58 (normal value 1.3 and 0.5) respectively and other pathologic parameters were: gamma GT 479 U/L (normal value 78), ALT 1032 u/L, AST 584 U/L (normal value 10-45), LDH 1855 U/L (normal value 313-618), ALP 283 U/L and C reactive protein (CRP) 6.8 mg/d (normal value < l). White blood cell count (WBC) was 13 200 (normal value 6000-9000) with 91 % polymorphonucleates, and blood glucose was 132 mg/dL. According to the Atlanta classification and Ranson’s criteria[1] the diagnosis of mild acute biliary pancreatitis was given and a conservative treatment was started with fluids, analgesics and imipenem. The main symptoms disappeared after 12 h so that the conservative treatment was continued. After 48 h a CT scan showed a pancreatic and peripancreatic oedema that was classified as Balthasar stage B[2]. The bilirubin remained slightly abnormal (1.62 total and 0.74 direct) but serum amylase and lipase were increased to 1300 and 30560 U/L respectively, whereas CRP reduced to 4.4 mg/dL. A cholangio-MRI was performed (Figure 1) showing a filling defect in the upper portion of the CBD that was highly suspicious for a gallstone, sludge or mucinous aggregate.
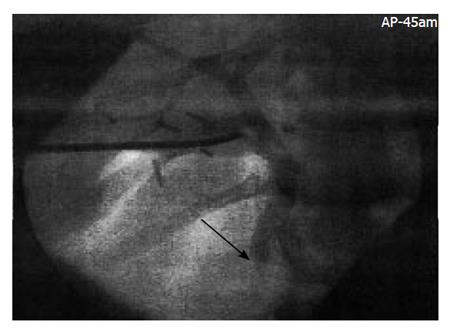
Based on increased experience in adults with cholecystocholedocolithiasis, we decided to perform a laparoendoscopic “Rendez-vous” for both the endoscopic drainage of the CBD and treatment of gallstones despite the fact that there was no evidence in the literature of this procedure being performed on a child that was considered suitable, without contraindication and useful. Laparo-endoscopic “Rendez-Vous” procedure was as follows: The whole laparo-endoscopic procedure was carried out to maintain the patient in the same supine “french” position used for the laparoscopic cholecystectomy. Three trocars (10-10-5 mm) were introduced with open technique. The first manoeuvre was the preparation, encircling and clipping of the cystic duct to avoid migration of stones in the CBD. An intra-operative cholangiography was performed to introduce a Pedinelli catheter (8 fr) in the cystic duct. This showed a dilated CBD and a delayed passage of the contrast medium in the duodenum (Figure 2), but could not confirm the filling defect. The X-ray picture of the whole biliary tree remained unmodified without any flow of the contrast medium in the duodenum, up to 30 minutes after the injection and despite intravenous administration of a dose of antispastic drug (cymetropio bromide). This led us to suspect an underlying sphincter of Oddi dysfunction but a manometry was considered unnecessary because the indication for retrograde exploration of the papilla was given. During the time waiting to control the passage of the contrast medium in the duodenum, the cholecystectomy was carried out. The endoscopist performed the procedure using an adult lateral view duodenoscope. The papilla appeared normal but without any flow of bile. A guide wire could be introduced through the papilla and its correct position inside the still contrasted CBD could be confirmed. In this way the standard and more dangerous unpreventable retrograde injection of the Wirsung duct could be avoided. A paediatric endoscopic balloon catheter Olympus Swift ® (4 mm diameter) was then introduced in the CBD, inflated, and retrieved trough the papilla. Some biliary sludge could be retrieved and immediately bile flowed. This procedure was repeated twice and a gentle dilatation of the papilla was also performed for 2 minutes. The endoscope was then extracted and the laparoscopic procedure ended after clipping of the cystic duct. The post-operative laboratory controls showed the normalization of amylase, lipase and bilirubin the day after. On day two after the procedure a control US showed a normal CBD. The patient was discharged three days after the procedure. Neither recurrence of symptoms, nor abnormality in laboratory tests or US controls occurred up to the last 24 mo follow-up.
Acute biliary pancreatitis in the child is rare and the main causes are congenital disorders or malformations of the pancreatic-biliary ductal system. In children, the main indication of diagnostic ERCP with or without endoscopic sphincterotomy (ES) are biliary atresia, intrahepatic cholestasis, anomalous arrangement of the pancreatic-biliary ductal system including the dilatation of the CBD.[3,4,5] In the adult, ES is a part of the treatment of ABP when this is caused by stones or sludge impacted in the papilla.[6,7] Concerning the timing of ERCP +/- ES, early approach is not more beneficial than conservative treatment in patients without jaundice.[8] In the child the literature concerning therapeutic ERCP with ES for ABP is scarce, especially because the pancreatitis, according to Hsu and Nowak[9,10] is often not “biliary” in the “adult” meaning of the term. In the reported case the pancreatitis was truly “biliary”, because related to micro-lithiasis and sludge and also combined with an underlying sphyncter of Oddi dysfunction which can often be related to recurrent pancreatitis also in children.[11] The treatment of ABP in childhood needs a multidisciplinary approach[12] to optimize laparoscopic treatment,[13,14] and intraoperative cholangiography is considered mandatory to minimize unnecessary ERCP.[15] In fact ERCP, combined with ES or not, carries the well known risk of iatrogenic acute pancreatitis because of papilla manipulation, pancreatic intraductal hyperpression and/or chemical damage all factors related to unpreventable retrograde injection of the pancreatic duct.[16,17] When ABP in children is related to gallstones there is a relevant risk of recurrence and therefore the standard treatment is endoscopic treatment sequentially combined days or weeks before or after cholecystectomy.[18,19] The sole case of urgent ERCP-ES in a 9-year-old patient with ABP due to a stone impacted in the papilla was reported recently[10] and was performed under anaesthesiological control of sedation. This patient was discharged after ES, with a planned laparoscopic cholecystectomy and was therefore still at risk of recurrent pancreatitis in the possible event of an incomplete sphincterotomy. There is the well known problem of the optimal timing between ERCP and LC, also considered “ The bilateral interface…” between the two procedures[20] but the optimal diagnostic and therapeutic approach in children will often depend on the level of expertise of both the biliary endoscopist and laparoscopist.[19,21,22] All these considerations and the favourable outcome of the case convinced us that simultaneous laparoendoscopic treatment carries great advantages especially in children. The literature shows that comparable good success rate of ERCP between adults and children (98 % vs 97.5 %) with a comparable low incidence of complications (2.5 % vs 3.4 %) are obtainable only by very experienced teams[22] but unfortunately complications can reach up to 33%.[18,21,23] Therefore ERCP in the paediatric population should be minimized because stones often pass spontaneously[19] and also because the only sure way to avoid post-ERCP complications is to avoid ERCP itself.[24] This is certainly possible with the combined laparo-endoscopic approach because ERCP is avoided and ES is limited only to those patients with stones or abnormal cholangiography that cannot be resolved la-paroscopically via the cystic duct or when a sphyncter of Oddi dysfunction can not be resolved through a simple dilatation. The balloon papilla dilatation carries comparable effectiveness but with a discordant incidence of relevant complications like pancreatitis that can be related to unnecessary retrograde injection of the pancreatic duct or manipulation, but anyway in children dilatation should be preferred to preserve the papilla.[25,26] The dilatation is also effective in early stone retrieval during the attack of ABP.[27]
Other favourable considerations concerning effectiveness of this combined approach can be found in the literature concerning the standard sequential approach. In a large prospective randomized study[28] the effectiveness of ERCP/ ES to clear CBD stones was only 84%, when performed prior to laparoscopic cholecystectomy and therefore 16 % can be ineffective. Unfortunately, these patients often also have to undergo urgent surgery, with exposure to a second X-Ray for the mandatory cholangiography and often the need for a surgical opening of the CBD. This carries the need of relevant surgical skill but carries also an increased risk of complications, often need of T tube or other biliary drain, and prolonged hospitalization[29,30]. In the child both open and laparoscopic surgery and especially suturing of the small duct requires a high degree of surgical expertise to avoid the risk of late stenosis of the CBD. On the other hand, laparoscopic clearance of CBD stones in a large prospective study28 of adults was impossible in 15 % of the cases, despite all being operated on by experienced surgeons, and conversion to open surgery or post-operative ERCP carried a relevant incidence of biliary complications, but the post-operative ERCP can itself be related to risk of ineffectiveness.
A recent analysis of management of suspected common bile duct stones in children[31] shows clearly the poor results and pitfalls of the two common pathways of the sequential treatment with ERCP-ES and laparoscopic cholecystectomy. If performed prior to cholecystectomy a total of 71 % of ERCP were unnecessary and 7 % failed, if performed after cholecystectomy 50 % of ERCP were unnecessary because stones were not found. Despite a reported incidence of 0 % complication rate, 9 of 12 ES (75 %) were unnecessary based on findings of an intraoperative cholangiography, some days prior. Therefore, a large number of unnecessary invasive procedures, all potentially related to morbidity and mortality, are often ineffective especially because they are out of synch with the evolving pathophysiology of gallstone disease.[19] On the other hand, the simultaneous approach of RV is tailored to a “real time” picture of the CBD and the compliance of the papilla, eliminating all previous and subsequent unnecessary procedures, and also minimizing the factors of ineffectiveness. Concerning ABP, endoscopy and laparoscopy, a recent review[32] pointed out that the sequential approach of ERCP-ES first followed by LC is the least efficient, and despite simultaneous treatment is theoretically the best option, the laparoscopic CBD clearance is considered difficult and time consuming.[32] The main experiences with the simultaneous laparoendoscopic approach[33,34] were always extremely positive, showing a high effectiveness in stone clearance of 97%-100 %, a low morbidity and hospital stay comparable to simple laparoscopic cholecystectomy.[35] It is also important to consider that for a child younger than 10 years of age the ERCP usually requires general anaesthesia[5,22] and an additional administration is certainly needed for the successive cholecystectomy. On the other hand, to perform the laparoendoscopic RV only one administration of anaesthesia and related psychological trauma is necessary for the child. The outcome of the case and the analysis of the literature, with a comparison of combined laparoendoscopic Rendez-Vous to the other available options convinced us that considering the technical aspects, the related risk of iatrogenic complications, optimization of the timing and the effectiveness of the procedure, the laparo-endoscopic Rendez-Vous in these cases is the best option for the child, perhaps also for the adult, the surgeon, the endoscopist and the hospital itself.
S- Editor Guo SY L- Editor Zhang JZ E- Editor Wu M
| 1. | Bradley EL 3rd. A clinically based classification system for acute pancreatitis. Summary of the International Symposium on Acute Pancreatitis, Atlanta, Ga, September 11 through 13, 1992. Arch Surg. 1993;128:586-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1929] [Cited by in RCA: 1735] [Article Influence: 54.2] [Reference Citation Analysis (1)] |
| 2. | Balthazar EJ, Robinson DL, Megibow AJ, Ranson JH. Acute pancreatitis: value of CT in establishing prognosis. Radiology. 1990;174:331-336. [PubMed] |
| 3. | Prasil P, Laberge JM, Barkun A, Flageole H. Endoscopic retrograde cholangiopancreatography in children: A surgeon's perspective. J Pediatr Surg. 2001;36:733-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 35] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Pfau PR, Chelimsky GG, Kinnard MF, Sivak MV Jr, Wong RC, Isenberg GA, Gurumurthy P, Chak A. Endoscopic retrograde cholangiopancreatography in children and adolescents. J Pediatr Gastroenterol Nutr. 2002;35:619-623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 42] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Teng R, Yokohata K, Utsunomiya N, Takahata S, Nabae T, Tanaka M. Endoscopic retrograde cholangiopancreatography in infants and children. J Gastroenterol. 2000;35:39-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 34] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Neoptolemos JP, Carr-Locke DL, London NJ, Bailey IA, James D, Fossard DP. Controlled trial of urgent endoscopic retrograde cholangiopancreatography and endoscopic sphincterotomy versus conservative treatment for acute pancreatitis due to gallstones. Lancet. 1988;2:979-983. [RCA] [DOI] [Full Text] [Cited by in Crossref: 572] [Cited by in RCA: 470] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 7. | Fan ST, Lai EC, Mok FP, Lo CM, Zheng SS, Wong J. Early treatment of acute biliary pancreatitis by endoscopic papillotomy. N Engl J Med. 1993;328:228-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 542] [Cited by in RCA: 439] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 8. | Fölsch UR, Nitsche R, Lüdtke R, Hilgers RA, Creutzfeldt W. Early ERCP and papillotomy compared with conservative treatment for acute biliary pancreatitis. The German Study Group on Acute Biliary Pancreatitis. N Engl J Med. 1997;336:237-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 414] [Cited by in RCA: 330] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 9. | Hsu RK, Draganov P, Leung JW, Tarnasky PR, Yu AS, Hawes RH, Cunningham JT, Cotton PB. Therapeutic ERCP in the management of pancreatitis in children. Gastrointest Endosc. 2000;51:396-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 64] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Nowak A, Kohut M, Nowakowska-Dulawa E, Romanczyk T, Granieski J. Acute biliary pancreatitis in a 9-year-old child treated with endoscopic sphincterotomy. Dig Liver Dis. 2003;35:656-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Guelrud M, Morera C, Rodriguez M, Jaen D, Pierre R. Sphincter of Oddi dysfunction in children with recurrent pancreatitis and anomalous pancreaticobiliary union: an etiologic concept. Gastrointest Endosc. 1999;50:194-199. [RCA] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 57] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 12. | Tagge EP, Tarnasky PR, Chandler J, Tagge DU, Smith C, Hebra A, Hawes RH, Cotton PB, Othersen HB Jr. Multidisciplinary approach to the treatment of pediatric pancreaticobiliary disorders. J Pediatr Surg. 1997;32:158-164; discussion 164-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Holcomb GW 3rd, Morgan WM 3rd, Neblett WW 3rd, Pietsch JB, O’Neill JA Jr, Shyr Y. Laparoscopic cholecystectomy in children: lessons learned from the first 100 patients. J Pediatr Surg. 1999;34:1236-1240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 32] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Shah RS, Blakely ML, Lobe TE. The role of laparoscopy in the management of common bile duct obstruction in children. Surg Endosc. 2001;15:1353-1355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Waldhausen JH, Graham DD, Tapper D. Routine intraoperative cholangiography during laparoscopic cholecystectomy minimizes unnecessary endoscopic retrograde cholangiopancreatography in children. J Pediatr Surg. 2001;36:881-884. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Pezzilli R, Romboli E, Campana D, Corinaldesi R. Mechanisms involved in the onset of post-ERCP pancreatitis. JOP. 2002;3:162-168. [PubMed] |
| 17. | Vandervoort J, Soetikno RM, Tham TC, Wong RC, Ferrari AP Jr, Montes H, Roston AD, Slivka A, Lichtenstein DR, Ruymann FW. Risk factors for complications after performance of ERCP. Gastrointest Endosc. 2002;56:652-656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 368] [Cited by in RCA: 348] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 18. | Rescorla FJ. Cholelithiasis, cholecystitis, and common bile duct stones. Curr Opin Pediatr. 1997;9:276-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 28] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Vrochides DV, Sorrells DL Jr, Kurkchubasche AG, Wesselhoeft CW Jr, Tracy TF Jr, Luks FI. Is there a role for routine preoperative endoscopic retrograde cholangiopancreatography for suspected choledocholithiasis in children. Arch Surg. 2005;140:359-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Esber EJ, Sherman S. The interface of endoscopic retrograde cholangiopancreatography and laparoscopic cholecystectomy. Gastrointest Endosc Clin N Am. 1996;6:57-80. [PubMed] |
| 21. | Zargar SA, Javid G, Khan BA, Yattoo GN, Shah AH, Gulzar GM, Singh J, Rehman BU, ud-din Z. Endoscopic sphincterotomy in the management of bile duct stones in children. Am J Gastroenterol. 2003;98:586-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Varadarajulu S, Wilcox CM, Hawes RH, Cotton PB. Technical outcomes and complications of ERCP in children. Gastrointest Endosc. 2004;60:367-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 77] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 23. | Lugo-Vicente HL. Trends in management of gallbladder disorders in children. Pediatr Surg Int. 1997;12:348-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 27] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Fogel EL. Endoscopic retrograde cholangiopancreatography topics. Endoscopy. 2003;35:913-919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Baron TH, Harewood GC. Endoscopic balloon dilation of the biliary sphincter compared to endoscopic biliary sphincterotomy for removal of common bile duct stones during ERCP: a metaanalysis of randomized, controlled trials. Am J Gastroenterol. 2004;99:1455-1460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 212] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 26. | Lin CK, Lai KH, Chan HH, Tsai WL, Wang EM, Wei MC, Fu MT, Lo CC, Hsu PI, Lo GH. Endoscopic balloon dilatation is a safe method in the management of common bile duct stones. Dig Liver Dis. 2004;36:68-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 56] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 27. | Toda N, Saito K, Wada R, Komatsu Y, Tada M, Kawabe T, Mitsushima T, Shiratori Y, Omata M. Early removal of bile duct stones in patients with acute biliary pancreatitis by endoscopic papillary balloon dilatation. Hepatogastroenterology. 2004;51:1263-1266. [PubMed] |
| 28. | Cuschieri A, Lezoche E, Morino M, Croce E, Lacy A, Toouli J, Faggioni A, Ribeiro VM, Jakimowicz J, Visa J. E.A.E.S. multicenter prospective randomized trial comparing two-stage vs single-stage management of patients with gallstone disease and ductal calculi. Surg Endosc. 1999;13:952-957. [RCA] [DOI] [Full Text] [Cited by in Crossref: 318] [Cited by in RCA: 291] [Article Influence: 11.2] [Reference Citation Analysis (1)] |
| 29. | Tranter SE, Thompson MH. Comparison of endoscopic sphincterotomy and laparoscopic exploration of the common bile duct. Br J Surg. 2002;89:1495-1504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 141] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 30. | Thompson MH, Tranter SE. All-comers policy for laparoscopic exploration of the common bile duct. Br J Surg. 2002;89:1608-1612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 77] [Article Influence: 3.3] [Reference Citation Analysis (1)] |
| 31. | Mah D, Wales P, Njere I, Kortan P, Masiakos P, Kim PC. Management of suspected common bile duct stones in children: role of selective intraoperative cholangiogram and endoscopic retrograde cholangiopancreatography. J Pediatr Surg. 2004;39:808-812; discussion 808-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 32. | Borie F, Fingerhut A, Millat B. Acute biliary pancreatitis, endoscopy, and laparoscopy. Surg Endosc. 2003;17:1175-1180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 33. | Wright BE, Freeman ML, Cumming JK, Quickel RR, Mandal AK. Current management of common bile duct stones: is there a role for laparoscopic cholecystectomy and intraoperative endoscopic retrograde cholangiopancreatography as a single-stage procedure. Surgery. 2002;132:729-35; discussion 735-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 32] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 34. | Meyer C, Le JV, Rohr S, Duclos B, Reimund JM, Baumann R. Management of common bile duct stones in a single operation combining laparoscopic cholecystectomy and peroperative endoscopic sphincterotomy. J Hepatobiliary Pancreat Surg. 2002;9:196-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 35. | Enochsson L, Lindberg B, Swahn F, Arnelo U. Intraoperative endoscopic retrograde cholangiopancreatography (ERCP) to remove common bile duct stones during routine laparoscopic cholecystectomy does not prolong hospitalization: a 2-year experience. Surg Endosc. 2004;18:367-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 72] [Article Influence: 3.4] [Reference Citation Analysis (0)] |