Published online Nov 28, 2005. doi: 10.3748/wjg.v11.i44.7048
Revised: June 6, 2005
Accepted: June 9, 2005
Published online: November 28, 2005
Plummer-Vinson syndrome (sideropenic dysphagia) is characterized by dysphagia due to an upper esophageal or hypopharyngeal web in patients with chronic iron deficiency anemia. The main cause of dysphagia is the presence of the web in the cervical esophagus, and abnormal motility of the pharynx or esophagus is also found to play a significant role in this condition. This syndrome is thought to be precancerous because squamous cell carcinoma of hypopharynx, oral cavity or esophagus takes place in 10% of those patients suffering from this malady, but it is even more unusual that Plummer-Vinson syndrome should be accompanied by gastric cancer. We have reported here a case of a 43-year-old woman with Plummer-Vinson syndrome who developed stomach cancer and recovered after a radical total gastrectomy with D2 nodal dissection.
- Citation: Kim KH, Kim MC, Jung GJ. Gastric cancer occurring in a patient with Plummer-Vinson syndrome: A case report. World J Gastroenterol 2005; 11(44): 7048-7050
- URL: https://www.wjgnet.com/1007-9327/full/v11/i44/7048.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i44.7048
Plummer-Vinson syndrome is characterized by dysphagia due to upper esophageal or hypopharyngeal web in patients with chronic iron deficiency anemia[1,2]. It is also combined with iron deficiency anemia, mucosal lesion of oral cavity or pharynx. This syndrome has been reported since 1893 in various literatures describing its specific symptoms. In 1926, Sir Arthur Hurst designated this symptom complex as Plummer-Vinson syndrome[1]. This syndrome is also referred to as Paterson-Kelly syndrome or sideropenic dysphagia. The main cause of dysphagia is the presence of a web in the cervical esophagus, and the abnormal motility of pharynx or esophagus is also found to play a significant role in the above causes[1,2]. It is well known that this syndrome is associated with an increased incidence of hypopharyngeal or cervical esophageal cancer. However, it is even more unusual that this syndrome is combined with gastric cancer[3]. So, we have reported a case of a 43-year-old woman who was initially diagnosed as Plummer-Vinson syndrome 2 years ago, and recently developed stomach cancer, which was managed successfully by surgery.
A 43-year-old woman was admitted to our hospital with symptoms of nausea, dysphagia and general weakness. She was diagnosed as Plummer-Vinson syndrome in April 2002, and has been managed conservatively on routine follow-ups. In August 2003, her nausea and dysphagia were aggravated. Her past history and family history were not specific. On admission, she complained about general weakness, mild abdominal pain and vomiting. The blood pressure was 0.247 kPa, pulse rate 90 bpm and body temperature 36.4 °C. The laboratory findings were consistent with microcystic, hypochronic iron deficiency anemia with 62 g/L hemoglobin, 22.2% hematocrit, 76.8 fL MCV, 21.5 pg MCH, 279 g/L MCHC, 325 000/μL platelet, 46 μg/dL serum iron, 271 μg/dL total iron binding capacity (TIBC), and 11.33 ng/mL serum ferritin. Urine analysis, serum liver function test (LFT), and serum electrolytes were unremarkable.
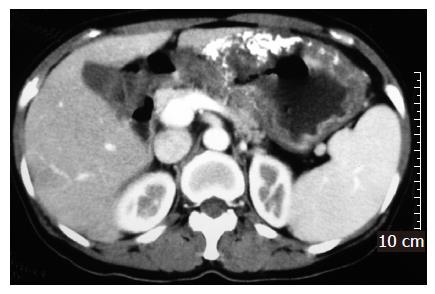
A gastrointestinal radiographic series indicated a linear filling defect (1.5 cm length) in the upper esophagus, which suggested an esophageal web (Figure 1). Contrast-enhanced abdominal CT scan showed diffuse irregular wall thickening with multiple calcifications at the body and antrum of the stomach. The CT scan also showed lymph node enlargement in the perigastric area and a mild enlargement of the spleen (Figure 2).
Esophagogastroduodenoscopic findings showed a web at 16 cm from the incisors. Upon endoscopic procedure for esophageal bougienage, we found a lesion at the cardia suspecting gastric cancer involving the upper body and the esophagogastric junction. Endoscopic biopsy proved to be a poorly differentiated adenocarcinoma. On surgical exploration, the serosa of the stomach was not invaded macroscopically by cancer, but hilar lymph nodes of the spleen were grossly enlarged, suspecting tumor metastasis. The patient underwent a radical total gastrectomy with D2 nodal dissection. The spleen was taken out along with lymph node #10 and lymph node #11 d. No transfusion was required during and after the surgery. Excised surgical specimen demonstrated that the tumor size was 22 cm×18 cm, and both resection margins were tumor-free. The lesion was histologically confirmed as mucinous adenocarcinoma, Borrmann type IV, and it had infiltrated into the serosa with nodal metastasis of 33 out of 62 nodes. The TMN stage was T3N3M0 (Stage IV) (Figure 3). Iron supplemented soft diet was commenced on the 6th postoperative day. Peripheral blood findings improved within 2 wk after the surgery: 87 g/L hemoglobin, 28.5% hematocrit, 81.9 fL MCV, 25.0 pg MCH, 30.5 g/dL MCHC, and 1 186 000/μL platelets. The patient was discharged on the 19th postoperative day with no remarkable surgical complications except a mild nausea and surgical wound discomfort.
Plummer-Vinson syndrome, also known as Paterson-Kelly syndrome or sideropenic dysphagia[1], is characterized by dysphagia, iron deficiency anemia, and mucosal lesion of the oral cavity or pharynx. In 1893, Blackenstein reported a case with anemia, spasmodic stenosis of cervical esophagus and dysphagia[1]. The patient’s symptoms were improved by endoscopic bougienage. In 1911, an another case with dysphagia due to upper esophageal web was reported, which was also alleviated by endoscopic bougienage. In 1912, Plummer[2] also reported cases with upper esophageal rigidity that the patients had iron deficiency anemia and splenomegaly. In 1922, Vinson named a series of patients with dysphagia, anemia, and splenomegaly as hysterical dysphagia[1]. In 1926, Sir Arthur Hurst designated similar cases of the syndrome as Plummer-Vinson syndrome[1].
The incidence of the Plummer-Vinson syndrome has recently decreased because of nutritional improvement, advanced health care, a decreased incidence of pregnancy and improved care programs for pregnant women. Moreover, this syndrome is now thought to be associated with the deficient intake of vitamins and iron[1,3,4]. Most patients are women aged over 40 years, and this group accounts for 75% in number[5,6]. The syndrome is usually asymptomatic, but the patients sometimes develop dysphagia, weight loss, and weakness. Other symptoms may include nail deformation of the hand and foot, cheilosis, atrophic glossitis, early loss of teeth, conjunctivitis, dermatitis seborrheica, hyperkeratosis, keratitis, blepharitis, visual disturbances and 30% of cases accompany splenomegaly[1]. The diagnosis of upper esophageal web is confirmed by radiologic methods or endoscopy. The radiologic method, however, is more suitable because endoscopy can sometimes miss the point of benign stricture, and does not verify most of the motility disorders[7]. On esophagography, the web is usually detected at the upper esophagus below the cricoid by showing a thin membrane across esophagus[8]. Pathologic finding of upper esophageal web shows hypertrophy or atrophy of squamous cells and it is sometimes combined with chronic inflammation[1].
Plummer-Vinson syndrome is known to be associated with an increased risk of upper alimentary tract cancers, and the incidence rate of upper esophageal cancer in this syndrome is 3-15%[6]. In Sweden, the incidence of upper alimentary tract cancer and hypopharyngeal cancer in Plummer-Vinson syndrome is decreasing along with that of the syndrome itself[3]. However, it is more unusual for this syndrome to be accompanied by gastric cancer. Only two cases were reported in the literature, in which gastric cancer developed in the lower portion of the stomach[9,10]. In our case, the gastric cancer developed in the upper portion of the stomach involving esophagogastric junction.
It is not clear why Plummer-Vinson syndrome can exceptionally be associated with stomach cancer. However, it is widely accepted that atrophic mucosal change of alimentary tract due to iron deficiency anemia may lead to cancer development of the upper esophagus or hypopharynx. Therefore, careful examinations of hypopharynx, upper esophagus and stomach are of crucial importance for early detection of cancer development in this syndrome.
Science Editor Kumar M and Guo SY Language Editor Elsevier HK
| 1. | Lichtenstein GR. Esophageal rings, webs, and diverticula. Bockus gastroenterology. Volume 1.5th ed. Philadelphia: WB Saunders Company 1994; 518-523. |
| 2. | Plummer HS. Diffuse dilatation of the esophagus without anatomic stenosis (cardiospasm): Report of 91 cases. JAMA. 1912;58:2013-2015. [RCA] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 53] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Larsson LG, Sandström A, Westling P. Relationship of Plummer-Vinson disease to cancer of the upper alimentary tract in Sweden. Cancer Res. 1975;35:3308-3316. [PubMed] |
| 4. | Chen TS, Chen PS. Rise and fall of the Plummer-Vinson syndrome. J Gastroenterol Hepatol. 1994;9:654-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 30] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Rosof BM, Nagler RW. Plummer-Vinson syndrome. Revisited. N Y State J Med. 1975;75:414-415. [PubMed] |
| 6. | Chisholm M. The association between webs, iron and post-cricoid carcinoma. Postgrad Med J. 1974;50:215-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 48] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Halpert RD, Feczko PJ, Spickler EM, Ackerman LV. Radiological assessment of dysphagia with endoscopic correlation. Radiology. 1985;157:599-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 36] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | SHAMMA'A MH, BENEDICT EB. Esophageal webs; a report of 58 cases & amp; an attempt at classification. N Engl J Med. 1958;259:378-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 83] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Nagai T, Susami E, Ebihara T. Plummer-Vinson syndrome complicated by gastric cancer: a case report. Keio J Med. 1990;39:106-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Kitabayashi K, Akiyama T, Tomita F, Saitoh H, Kosaka T, Kita I, Takashima S. Gastric cancer occurring in a patient with Plummer-Vinson syndrome: report of a case. Surg Today. 1998;28:1051-1055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |