Published online Nov 7, 2005. doi: 10.3748/wjg.v11.i41.6560
Revised: May 9, 2005
Accepted: May 12, 2005
Published online: November 7, 2005
Primary splenic angiosarcoma is a very rare, aggressive neoplasm with a high metastatic rate and dismal prognosis. This neoplasm usually presents with abdominal pain, splenomegaly, anemia, and thrombocytopenia. Splenic angiosarcoma with bleeding gastrointestinal metastases is extremely rare. The literature contains only two case reports. This study reported a 44-year-old male patient with splenic angiosarcoma with sustained repeated gastrointestinal bleeding due to small bowel metastases. Salvage surgery was performed by splenectomy and resection of the metastatic small bowel tumors. The post-operative course was uneventful; the patient survived with the disease and had no GI bleeding, 7 mo after surgery.
- Citation: Hsu JT, Lin CY, Wu TJ, Chen HM, Hwang TL, Jan YY. Splenic angiosarcoma metastasis to small bowel presented with gastrointestinal bleeding. World J Gastroenterol 2005; 11(41): 6560-6562
- URL: https://www.wjgnet.com/1007-9327/full/v11/i41/6560.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i41.6560
Primary splenic angiosarcoma is a very rare neoplasm with a high metastatic rate and dismal prognosis. Langhans[1] first identified this disease in 1879. Presentations of splenic angiosarcoma are extremely variable and frequently cause diagnostic difficulties. The disease usually manifests with abdominal mass, abdominal pain, splenomegaly, and anemia. Distant metastases can occur in the liver, lung, lymph node, and bone, and soft tissue[2]. To our knowledge, splenic angiosarcoma with bleeding gastrointestinal (GI) metastases is extremely rare. The literature contains only two case reports[3,4]. The present case is the first report of splenic angiosarcoma metastasis to the small bowel. This work describes the experience of the authors in the management of the splenic angiosarcoma with bleeding GI metastases.
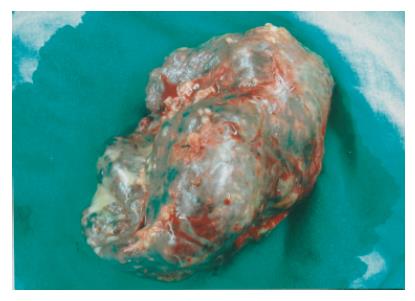
A 44-year-old male patient was admitted to Chang Gung Memorial Hospital on July 1, 2004, complaining of severe lower back pain and progressively weakness in his bilateral lower legs for 1 mo. Subconjunctiva hemorrhage and gingival bleedings were noted during initial examination mild pale conjunctiva, hepatomegaly, and splenomegaly. The hematogram measured hemoglobin at 108 g/L and platelet at 137 000/cm3. Prothrombin and activated partial thromboplastin times were normal. Magnetic resonance imaging of the spine identified abnormal enhancement at multiple bodies in the thoracic, lumbar, and sacral spines, which were assumed to be metastatic lesions. Unfortunately, the patient developed hematochezia 9 d after admission. Persistent passage of tarry stools resulted in severe anemia (the lowest hemoglobin level was 43 g/L) and an episode of syncope. The patient received transfusions of packed RBC to a total of 12 U, before surgery. Both endoscopy and colonscopy failed to detect the site of bleeding. Abdominal computed tomography showed a diffusely heterogeneous density infiltrating the whole spleen (Figure 1) and did not detect any GI tumors. The scan of Tc-99m RBC revealed evidence of active bleeding in the left mid-abdominal region. The patient then underwent an exploratory laparotomy on July 17, 2004. During surgery, the spleen was enlarged with multiple dark-red nodules on its surface (Figure 2). Intra-operative endoscopy failed to identify any site of bleeding. The serosa of the small intestine was intact and multiple small hemorrhagic patches (number >5) were observed at the jejunum and ileum (Figure 3). Splenectomy and resection of the small intestine containing hemorrhagic patches were then performed.
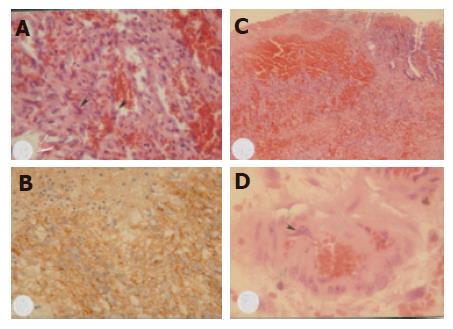
Macroscopically, the surgical specimen of the spleen measured 14 cm×10 cm×9 cm with a weight of 400 g, and the splenic parenchyma was diffusely scattered with multiple, irregular sized and dark-red color nodules. Mucosal tumors (size <1 cm) were identified at the resected small intestine. Microscopically, the spleen revealed neoplastic sinusoidal endothelial cells with marked cytological atypia lining the congested sinusoid spaces (Figure 4A). The tumor cells were immunoreactive to factor XIII associated antigen (polyclonal, 1:500, Calbiochem Novabiochem, CA, USA, Figure 4B). The neoplastic cells of the small intestine only involved the mucosal and submucosal layers (Figure 4C); the muscular layer and serosa were intact and free of malignancy. They formed anastomosing network of sinusoids lined by pleomorphic endothelial cells, similar to those seen in the spleen. In addition, individual tumor cells were identified within the small vessels (Figure 4D). The diagnosis of primary splenic angiosarcoma with metastases of bones and small intestine was confirmed.
The patient had an uneventful post-operative course. He received external beam radiation therapy for his bone pain postoperatively. He did not experience GI bleeding again and survived with the disease 7 mo after surgery.
PATIENTS WITH splenic angiosarcoma may occur at any age[2,5-7]. The mean age of the reported patients was 50-60 years[2,5,6]. The pathogenesis of splenic angiosarcoma remains unknown. Reported causes are exposed to ionizing radiation[8] or chemotherapy for lymphoma[9]. However, some authors believed that splenic angiosarcoma develops from a previously existing benign counterparts of the splenic tumors such as hemangioma or hemangioendothelioma[7,8]. In this case, no such risk factors were noted.
Splenomegaly with left-side upper abdominal pain occurs in over 70% of patients with splenic angiosarcoma[2,5]. Anemia and thrombocytopenia are the frequent findings of hematogram and are reported in more than 70% of cases[5,6]. Spontaneous splenic rupture presenting with acute abdominal pain has been reported in 13%-32% of patients[2,5,10]. Other systemic symptoms such as body weight loss, gum bleeding, fatigue, weakness, fever, chest pain, and GI bleeding have also been observed[2,5].
Metastases of the splenic angiosarcoma are frequent, occurring in 69-100% of cases[2,5]. The most common metastasis sites are the liver, lung, lymph node, bone, bone marrow, and soft tissue. To the best of our knowledge, the present patient is the first case report of splenic angiosarcoma metastasis to the small bowel.
Malignancies of the small bowel can be either primary or metastatic. Primary small bowel malignant tumors are rare with the incidence of about 1 per 100000 and a prevalence of 0.6%[11]. Secondary neoplastic involvement of the small bowel is more frequent than primary small bowel neoplasm by hematogenous spread, direct invasion or intraperitoneal seeding[12]. Metastatic malignant tumors from the colon, ovary, uterus, and stomach generally invade the small bowel via direct invasion or intraperitoneal spread. The breast cancer, lung cancer, and melanoma usually metastasize to the small bowel hematogenously. Based on the operative and histopathologic findings, this case is the first report of small bowel metastases from the splenic angiosarcoma via hematogenous route.
The prognosis for splenic angiosarcoma is typically very dismal with a 6-mo survival for only 20% of cases[2,4]. Notably, survival of pediatric patients was reported as extremely poor ranging from less than 1 mo to 2 years[13]. However, Falk et al[5] had reported that two adults survived at the last follow-up, 1 with disease at 8 years and the other disease-free at 10 years. Survival is favorable for early diagnosis with splenectomy before rupture[4,10]. Montemayor and Caggiano[14] also found that patients with splenic angiosarcoma had longer survival, if splenectomy was performed prior to rupture compared to after rupture (14.4 vs 4.4 mo).
Table 1 shows only three cases including this case that have experienced GI bleeding due to GI metastasis from the splenic angiosarcoma (Table 1). In patients with either primary or metastatic GI angiosarcoma, repeated GI bleeding and the need for blood transfusion made them hospitalization-dependent and debilitated. These patients frequently die of uncontrolled GI bleeding[15]. The survival of these patients in Allison’s study ranges from 1 wk to 3 years after resection of the foci[15]. No consensus yet exists regarding the need to treat patients with disseminated metastases aggressively. Nevertheless, salvage surgery (resection of small bowel metastases) combined with splenectomy to control bleeding and confirm diagnosis was justified in the present case. The patient survived with the disease, 7 mo after surgery without evidence of GI bleeding.
| Author/yr | Age/sex | Site of GI metastasis | Treatment | Status and time of follow-up |
| Chung[3] 1999 | 54/M | ND | Splenectomy | DOD, 10 mo |
| Jimenez-Heffernan[4] 1999 | 71/F | Colon (splenic flexure) | Splenectomy, left | DOD, 9 mo |
| hemicolectomy, radiation | ||||
| Hsu, present | 45/M | Small bowel | Splenectomy, resection of small | AWD, 7 mo |
| bowel metastases, radiation |
In conclusion, splenic angiosarcoma with bleeding GI metastases is extremely rare. This case is the first report of metastatic small bowel malignancy from the splenic angiosarcoma. Salvage surgery to control bleeding due to the GI metastases is justified in this case.
Science Editor Guo SY Language Editor Elsevier HK
| 1. | Langhans T. Pulsating cavernous neoplasm of the spleen with metastatic nodules to the liver. Vichows Arch Pathol Anat. 1879;75:273-291. [RCA] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 47] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Neuhauser TS, Derringer GA, Thompson LD, Fanburg-Smith JC, Miettinen M, Saaristo A, Abbondanzo SL. Splenic angiosarcoma: a clinicopathologic and immunophenotypic study of 28 cases. Mod Pathol. 2000;13:978-987. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 128] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 3. | Chung YF, Busmanis I, Hong GS, Soo KC. Splenic angiosarcoma--an unusual cause of bleeding gastrointestinal tract. Singapore Med J. 1999;40:106-108. [PubMed] |
| 4. | Jiménez-Heffernan JA, Hardisson D, Prieto-Nieto MI, Burgos E. Ruptured primary splenic angiosarcoma into the colon. Presentation as anal bleeding. Acta Gastroenterol Belg. 1999;62:248-251. [PubMed] |
| 5. | Falk S, Krishnan J, Meis JM. Primary angiosarcoma of the spleen. A clinicopathologic study of 40 cases. Am J Surg Pathol. 1993;17:959-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 142] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 6. | Chen KT, Bolles JC, Gilbert EF. Angiosarcoma of the spleen: a report of two cases and review of the literature. Arch Pathol Lab Med. 1979;103:122-124. [PubMed] |
| 7. | Alt B, Hafez GR, Trigg M, Shahidi NT, Gilbert EF. Angiosarcoma of the liver and spleen in an infant. Pediatr Pathol. 1985;4:331-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 37] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Sordillo EM, Sordillo PP, Hajdu SI. Primary hemangiosarcoma of the spleen: report of four cases. Med Pediatr Oncol. 1981;9:319-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Zwi LJ, Evans DJ, Wechsler AL, Catovsky D. Splenic angiosarcoma following chemotherapy for follicular lymphoma. Hum Pathol. 1986;17:528-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Autry JR, Weitzner S. Hemangiosarcoma of spleen with spontaneous rupture. Cancer. 1975;35:534-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 11. | Attanoos R, Williams GT. Epithelial and neuroendocrine tumors of the duodenum. Semin Diagn Pathol. 1991;8:149-162. [PubMed] |
| 12. | Gill SS, Heuman DM, Mihas AA. Small intestinal neoplasms. J Clin Gastroenterol. 2001;33:267-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 146] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 13. | Kren L, Kaur P, Goncharuk VN, Dolezel Z, Krenova Z. Primary angiosarcoma of the spleen in a child. Med Pediatr Oncol. 2003;40:411-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Montemayor P, Caggiano V. Primary hemangiosarcoma of the spleen associated with leukocytosis and abnormal spleen scan. Int Surg. 1980;65:369-373. [PubMed] |
| 15. | Allison KH, Yoder BJ, Bronner MP, Goldblum JR, Rubin BP. Angiosarcoma involving the gastrointestinal tract: a series of primary and metastatic cases. Am J Surg Pathol. 2004;28:298-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 87] [Article Influence: 4.1] [Reference Citation Analysis (0)] |