Published online Nov 7, 2005. doi: 10.3748/wjg.v11.i41.6554
Revised: January 23, 2005
Accepted: January 26, 2005
Published online: November 7, 2005
Papillary carcinoma arising from the extrahepatic bile duct often shows superficial ductal spread. We report herein the case of a patient with extensive superficial spread of non-invasive papillary cholangiocarcinoma, which was depicted with peroral cholangioscopy. A 65-year-old woman presented with the sudden-onset of severe epigastric pain. Ultrasonography revealed acute acalculous cholecystitis. Endoscopic retrograde cholangiography found small protruding lesions around the confluence of the cystic duct, suggestive of a cholangiocarcinoma. As the contour of the middle and upper bile ducts it was slightly irregular on the cholangiogram, the presence of superficial ductal spread was suspected. Peroral cholangioscopy revealed small papillary lesions around the confluence of the cystic duct and fine granular mucosal lesions in the middle and upper bile ducts and the right hepatic duct, suggesting a superficially spreading tumor. A right hepatectomy with bile duct resection was performed and no residual tumor was found. Histological examination revealed a non-invasive papillary carcinoma arising from the cystic duct with extensive superficial spread. Our experience of this case and a review of the literature suggest that a fine granular or fine papillary appearance of the ductal mucosae on cholangioscopy indicates superficial spread of papillary cholangiocarcinoma, for which peroral cholangioscopy is an efficient diagnostic option.
- Citation: Wakai T, Shirai Y, Hatakeyama K. Peroral cholangioscopy for non-invasive papillary cholangiocarcinoma with extensive superficial ductal spread. World J Gastroenterol 2005; 11(41): 6554-6556
- URL: https://www.wjgnet.com/1007-9327/full/v11/i41/6554.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i41.6554
Papillary carcinoma arising from the extrahepatic bile duct often shows superficial ductal spread[1]. Peroral cholangioscopy, introduced in the 1970s by Rosch et al[2] and Nakajima et al[3], provides direct visualization of the biliary ducts. We report herein the case of a patient with extensive superficial ductal spread of non-invasive papillary cholangiocarcinoma, which was depicted with peroral cholangioscopy.
A 65-year-old woman presented with the sudden-onset of severe epigastric pain. No jaundice was observed on physical examination, and the serum total bilirubin level was 0.6 mg/dL (reference range: 0.3-0.9 mg/dL). The serum levels of carcinoembryonic antigen and carbohydrate antigen 19-9 were 0.7 ng/mL (reference range: 0-6 ng/mL) and 6 U/mL (reference range: 0-37 U/mL), respectively.
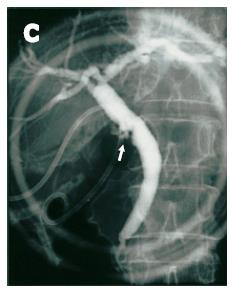
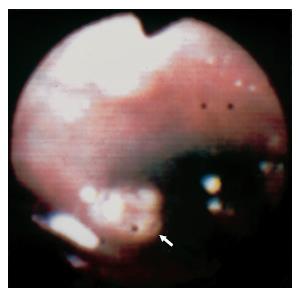
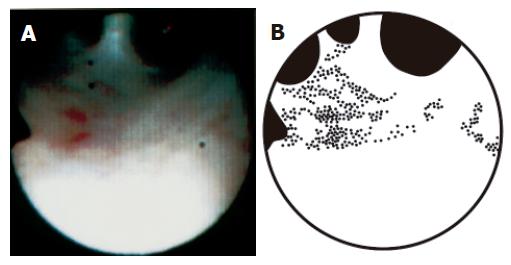
Ultrasonography revealed acute acalculous cholecystitis, for which percutaneous cholecystostomy was performed. Endoscopic retrograde cholangiography found small protruding lesions around the confluence of the cystic duct, suggestive of a cholangiocarcinoma (Figure 1). Smear cytology of the ductal bile aspirated during endoscopic retrograde cholangiography revealed that exfoliated cells were categorized into Papanicolaou class II. As the contour of the middle and upper bile ducts was slightly irregular on the cholangiogram, the presence of superficial ductal spread was suspected. In order to confirm this, peroral cholangioscopy using a fiberoptic endoscope (CHF-B20QY, Olympus, Tokyo, Japan) was performed, and both small papillary lesions around the confluence of the cystic duct (Figure 2) and fine granular mucosal lesions, brownish in color, in the middle and upper bile ducts were revealed, suggesting a superficially spreading tumor. Such mucosal lesions were also seen in the right hepatic duct (Figure 3).
After laparotomy, a bile duct resection with regional lymphadenectomy was performed. As the resection margin at the right hepatic duct was positive for in situ carcinoma on frozen-section examination, a right hepatectomy was additionally performed and no residual tumor was found. Histological examination of the resected specimen revealed a non-invasive papillary carcinoma arising from the cystic duct, with superficial spread extending up to the right anterior sectoral duct (pathologic T1N0M0, Stage IA, according to the tumor-node-metastasis staging system[4]). Fine granular mucosal lesions on peroral cholangioscopy (Figure 3) corresponded to papillary in situ carcinoma histologically, whereas the flat mucosae between the fine granular mucosal lesions, which appeared normal on cholangioscopy (Figure 3), corresponded to non-papillary in situ carcinoma. The patient remains healthy, with no evidence of recurrence 7 years after the resection.
Nimura and Kamiya[5,6] demonstrated, by means of percutaneous transhepatic cholangioscopy, that a fine granular or fine papillary appearance of the ductal mucosae indicates superficial spread of cholangiocarcinoma. In the current case, the fine granular mucosal appearance on cholangioscopy corresponded to papillary in situ carcinoma histologically. It is very likely that a fine granular or fine papillary mucosal appearance on cholangioscopy is pathognomonic of superficial ductal spread of papillary cholangiocarcinoma.
The ductal resection margin status is an established prognostic factor in patients with extrahepatic cholangio-carcinoma[7,8]. Although intraductal ultrasonography is helpful in discerning T category of biliary malignancies[9], the extent of the superficial spread of cholangiocarcinoma is difficult to determine preoperatively on imaging studies[5,10,11]. In the current case, although peroral cholangioscopy detected papillary in situ carcinoma in the form of fine granular lesions, it did not detect the non-papillary in situ carcinoma between the lesions, suggesting that cholangioscopy is incapable of detecting flat ductal spread of in situ carcinoma. Intraoperative frozen-section examination is indispensable in assessing the ductal resection margin status.
In conclusion, a fine granular or fine papillary appeara-nce of the ductal mucosae on cholangioscopy suggests superficial spread of papillary cholangiocarcinoma, for which peroral cholangioscopy is an efficient diagnostic option, unless the superficial lesions are flat.
Science Editor Wang XL and Guo SY Language Editor Elsevier HK
| 1. | Sakamoto E, Nimura Y, Hayakawa N, Kamiya J, Kondo S, Nagino M, Kanai M, Miyachi M, Uesaka K. The pattern of infiltration at the proximal border of hilar bile duct carcinoma: a histologic analysis of 62 resected cases. Ann Surg. 1998;227:405-411. [RCA] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 213] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 2. | Rosch W, Koch H, Demling L. Peroral cholangioscopy. Endoscopy. 1976;8:172-175. [RCA] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 39] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Nakajima M, Akasaka Y, Fukumoto K, Mitsuyoshi Y, Kawai K. Peroral cholangiopancreatosocopy (PCPS) under duodenoscopic guidance. Am J Gastroenterol. 1976;66:241-247. [PubMed] |
| 4. | Greene FL, Page DL, Fleming ID, Fritz AG, Balch CM, Haller DG, Morrow M. American Joint Committee on Cancer Staging Manual (6th edition). New York: Springer-Verlag 2002; 131-138. [DOI] [Full Text] |
| 5. | Nimura Y. Staging of biliary carcinoma: cholangiography and cholangioscopy. Endoscopy. 1993;25:76-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 105] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | Nimura Y, Kamiya J. Cholangioscopy. Endoscopy. 1996;28:138-146. [RCA] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Wakai T, Shirai Y, Moroda T, Yokoyama N, Hatakeyama K. Impact of ductal resection margin status on long-term survival in patients undergoing resection for extrahepatic cholangiocarcinoma. Cancer. 2005;103:1210-1216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 180] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 8. | Burke EC, Jarnagin WR, Hochwald SN, Pisters PW, Fong Y, Blumgart LH. Hilar Cholangiocarcinoma: patterns of spread, the importance of hepatic resection for curative operation, and a presurgical clinical staging system. Ann Surg. 1998;228:385-394. [RCA] [DOI] [Full Text] [Cited by in Crossref: 348] [Cited by in RCA: 312] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 9. | Menzel J, Poremba C, Dietl KH, Domschke W. Preoperative diagnosis of bile duct strictures--comparison of intraductal ultrasonography with conventional endosonography. Scand J Gastroenterol. 2000;35:77-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 99] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 10. | Barish MA, Yucel EK, Ferrucci JT. Magnetic resonance cholangiopancreatography. N Engl J Med. 1999;341:258-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 140] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 11. | Tamada K, Ido K, Ueno N, Kimura K, Ichiyama M, Tomiyama T. Preoperative staging of extrahepatic bile duct cancer with intraductal ultrasonography. Am J Gastroenterol. 1995;90:239-246. [PubMed] |