Published online Jul 14, 2005. doi: 10.3748/wjg.v11.i26.4120
Revised: October 2, 2004
Accepted: October 6, 2004
Published online: July 14, 2005
Diagnosis of hepatocellular carcinoma (HCC), a common digestive malignancy, remains a challenge. The aim of this study was to evaluate the feasibility of performing laparoscopy and laparoscopic ultrasound with local anesthesia as a diagnostic procedure in HCC. Laparoscopy and laparoscopic ultrasound with local anesthesia was performed in the gastrointestinal endoscopy unit in three patients diagnosed of HCC. Endoscopy staged diffuse liver disease. Laparoscopic ultrasonography identified all liver tumors not visible during endoscopy and guided needle biopsy in one case. No complications happened. In conclusion, laparoscopy and laparoscopic ultrasound, performed as a minimally invasive diagnostic procedure can be a safe and very promising tool in planning therapy of HCC.
- Citation: Gómez-Rubio M, Moya-Valdés M, García J. Diagnostic laparoscopy and laparoscopic ultrasonography with local anesthesia in hepatocellular carcinoma. World J Gastroenterol 2005; 11(26): 4120-4123
- URL: https://www.wjgnet.com/1007-9327/full/v11/i26/4120.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i26.4120
Hepatocellular carcinoma (HCC) is the most common primary liver cancer[1]. Nevertheless, less than a third of patients are candidate to radical treatments[2]. Besides the low hepatic reserve of usual underlying cirrhosis, one of the explanations of these poor results are the limited accuracy and discrepancies between the imaging techniques in the discovering and staging of neoplasm[3,4]. There is a common agreement that the most accurate diagnostic method is operative assessment with ultrasound[5,6]. But this approach bears an unacceptable morbidity and mortality precluding its general use.
Laparoscopy, initially introduced in gastroenterology, affords an excellent view of the intra-abdominal organs, although the inner part is not accessible to inspection[7]. In the mid-1980’s pilot studies described laparoscopic ultrasound that combined the advantages of a visual assessment of peritoneal cavity and all the organs, specifically the liver, with the high resolution of intraoperative ultrasound examination[8-10]. More recently, with the incorporation of laparoscopic surgery into the practice of general surgery, it has been shown that this procedure optimizes staging in hepatic malignancy[1-4]. However, surgical laparoscopic ultrasound typically performed under general anesthesia exposes patients to certain risks and increases costs. So, laparoscopy with ultrasound scanning, performed under local anesthesia could be a safer procedure providing meaningful information.
Our initial experience using diagnostic laparoscopy and laparoscopic ultrasound with local anesthesia is shown.
Laparoscopy with laparoscopic ultrasound procedures was performed in three consecutive patients diagnosed of HCC. The procedures were performed with local anesthesia in the gastrointestinal endoscopy unit. Oxygen saturation and heart rate were automatically monitored. After puncturing in the left upper quadrant of the abdomen, near the umbilicus, with a multihole 21-gauge needle, pneumope-ritoneum with oxygen insufflation was established. Then, two 11-mm laparoscopic trocars were inserted. The first one was inserted through the pneumoperitoneum puncture site. Then, a frontal high-resolution video laparoscope (Olympus GTV-S6, Olympus Optical Co., Ltd, Japan) was introduced into the cannula, performing an initial endoscopic exploration of the peritoneal cavity. Another trocar was positioned to introduce the ultrasonic probe making a choice between the right paraumbilical region and the right inferior quadrant in accordance with abdominal characteristics. The laparoscopic ultrasonography was performed using ultrasonographic equipment (Olympus IU-E1, Olympus Optical Co., Ltd, Japan) that included a linear 7.5 MHz, 9.9 mm in diameter, orientable-tip probe (Olympus MH-300, Olympus Optical Co., Ltd, Japan) placed in contact with liver capsule. All probe manipulations during ultrasound scanning were guided by direct eye vision. The liver was systematically scanned at its front, upper (diaphragmatic), and lateral surfaces by moving the probe. For the left lobe exploration of the liver, the probe was transferred to the epigastric port. The parenquima, hepatic and portal veins were then carefully scanned, by using advancement-withdrawal maneuvers, lateral movements, sweeping and rotating the probe over the liver surface, in an attempt to identify the segmental anatomy. Duration of procedure ranged between 60 and 90 min. Recovery monitoring was performed for 15 min in gastrointestinal suite. Patients were then admitted for 22-h observation and later discharged.
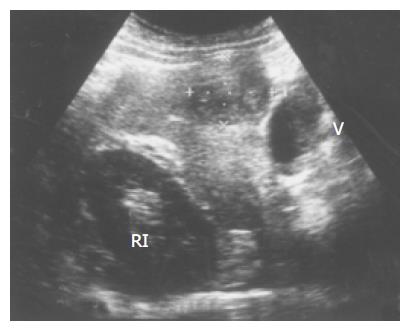
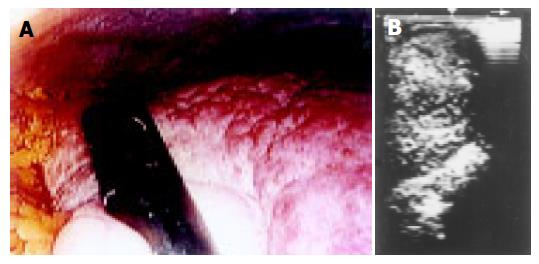
A 69-year-old male patient with previous chronic C hepatitis was diagnosed after abdominal ultrasonography and biopsy of HCC. Ultrasonography and abdominal computed tomography showed one tumor, 36 mm in diameter, located in the right lobe (segment V) (Figure 1). Laparoscopic examination demonstrated liver cirrhosis without tumor in surface (Figure 2A). Laparoscopic sonogram described the neoplastic deposit that was impossible to endoscopically visualize (Figure 2B). No other tumors were discovered inside the liver. Two grams of magnesium metamizole were intravenously administered at the end of procedure. Some days later, laparotomy with intraoperative ultrasonography was carried out with no additional findings, and then a surgical atypical hepatectomy was performed. Postoperatory was unremarkable and patient has remained without recurrence for 21 mo.
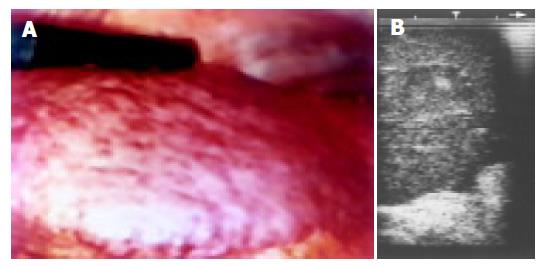
A 51-year-old male diagnosed of alcoholic and viral C liver cirrhosis with portal hypertension developed ascites. He had a history of a hemangioma in both liver lobes. Former abdominal ultrasonography and computed tomography discovered a new 16-mm nodule whose biopsy diagnosed a HCC (Figure 3). Laparoscopy showed liver cirrhosis with portal hypertension and ascites (Figure 4A), whereas laparoscopic ultrasonography confirmed previous conventional radiological findings (Figure 4B). No analgesic drugs were required. Although the patient was selected for resection at that moment, during laparotomy unresectability was determined after discovering malignant diaphragm implant, and then radio-frequency treatment was carried out. The patient, in Child-Pugh B functional stage, refused liver transplantation and no antitumoral therapy was given.
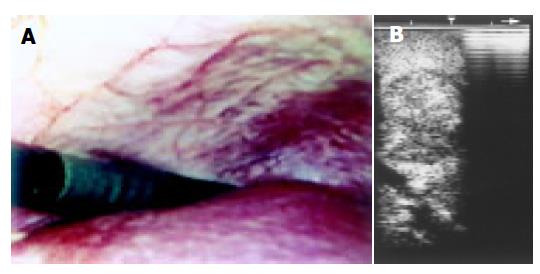
A 59-year-old male with prior history of 140 g/d of ethanol intake started with right hypocondrium pain. After abdominal sonogram, computed tomography scans and abnormal serum α-fetoprotein (2 440 ng/mL) a diagnosis of HCC was made (Figure 5). There were 4 tumors in right lobe, ranging from 1 to 7 cm in diameter. On laparoscopy chronic non-cirrhotic liver disease without neoplasm on surface was discovered (Figure 6A). Laparoscopic ultrasonography showed all the lesions. Sonographically guided biopsy gave a confirmatory result of HCC (Figure 6B). Non-neoplastic tissue obtained at laparoscopy revealed an alcoholic hepatitis with fibrosis but without cirrhosis. Magnesium metamizole (2 g) combined with atropine (1 mg) were intravenously given during the procedure. Twenty moths later the patient is alive in a consumptive state.
Staging surgical laparoscopy with laparoscopic ultrasound, has been reported in the last several years as an important tool in the diagnostic approach to hepatobiliary and pancreatic malignancy, avoiding unnecessary laparotomy in up to 46% of patients[11-14]. In HCC, surgical laparoscopy with laparoscopic ultrasound also optimizes patient selection for curative hepatic resection, discovering unresectable disease in as much as 63% of cases[15-17].
Some years ago, Ido et al[18] reported in Japan that laparoscopic ultrasound performed with local anesthesia diagnosed new nodular lesions in 64 out of 186 patients (34%). Twenty-eight nodules in 23 of the 186 patients (12%) were identified as HCC after biopsy. During the follow-up other 10 lesions, which had initially described as noncarcinomatous nodules, were diagnosed as HCC. So, laparoscopic ultrasonography discovered new HCC nodules in 17% of patients, defining multicentric neoplasm and avoiding unnecessary open surgery.
In our patients, laparoscopy with laparoscopic ultrasound was successfully performed in the gastrointestinal endoscopy unit. There were no complications related to procedure that was done just under local anesthesia with non-narcotic analgesic drugs. So, this type of diagnostic laparoscopy seems as safe as standard laparoscopy[7]. Endoscopic findings were liver cirrhosis in two cases (one with portal hypertension and ascites) and chronic liver disease without cirrhosis in the other one. There were no tumors on the liver surface. Extrahepatic, including peritoneal, spread was not detected.
Laparoscopic ultrasonography confirmed location and number of lesions diagnosed by conventional imaging. In particular, ultrasonographic pictures had similar characteristics to those of transparietal sonography, but with higher quality and definition. In the patient lacking previous histologic diagnosis, the tumor was biopsied with laparoscopic ultrasound guidance, achieving a definitive confirmation of hepatocellular carcinoma.
In conclusion, our preliminary experience suggests that laparoscopy with laparoscopic ultrasonography carried out with local anesthesia in a nearly ambulatory setting could be a safe, effective and relatively simple procedure in staging of HCC and optimizing patient selection for liver resection or transplantation. The procedure, that is well tolerated and carried out with minimal drug therapy, may be cost-effective for HCC diagnostic assessment. Ultrasonography, providing the image of interior of the liver and guiding puncture, increased sensitivity to laparoscopic procedure. On the other hand, endoscopic examination diagnosed in one case a non-cirrhotic liver, later confirmed after biopsy, finding that is associated with a better chance of hepatectomy and survival. Staging was correct in all cases except one wherein diaphragm infiltration was not detected at endoscopic study. The visual assessment of some areas, as dorsal surface of the right lobe, is still difficult and led to this false negative result. This problem could probably be overcome employing an orientable-tip device. Besides, this technique could be also useful in detection and ultrasonography-guided biopsy of lesions not accessible to conventional diagnostic approach. Consequently, this procedure, which may be a powerful tool in the management of HCC, must be extensively evaluated.
The authors thank Olympus España (Medical Europa) for the ultrasonographic equipment used in this study.
Science Editor Li WZ Language Editor Elsevier HK
| 1. | Bosch FX, Ribes J, Borràs J. Epidemiology of primary liver cancer. Semin Liver Dis. 1999;19:271-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 671] [Cited by in RCA: 671] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 2. | Llovet JM, Burroughs A, Bruix J. Hepatocellular carcinoma. Lancet. 2003;362:1907-1917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3241] [Cited by in RCA: 3282] [Article Influence: 149.2] [Reference Citation Analysis (0)] |
| 3. | Wernecke K, Rummeny E, Bongartz G, Vassallo P, Kivelitz D, Wiesmann W, Peters PE, Reers B, Reiser M, Pircher W. Detection of hepatic masses in patients with carcinoma: comparative sensitivities of sonography, CT, and MR imaging. AJR Am J Roentgenol. 1991;157:731-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 160] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 4. | Murakami T, Mochizuki K, Nakamura H. Imaging evaluation of the cirrhotic liver. Semin Liver Dis. 2001;21:213-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 34] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Makuuchi M, Takayama T, Kosuge T, Yamazaki S, Yamamoto J, Hasegawa H, Takayasu K. The value of ultrasonography for hepatic surgery. Hepatogastroenterology. 1991;38:64-70. [PubMed] |
| 6. | Luck AJ, Maddern GJ. Intraoperative abdominal ultrasonography. Br J Surg. 1999;86:5-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Schneider AR, Eickhoff A, Arnold JC, Riemann JF. Diagnostic laparoscopy. Endoscopy. 2001;33:55-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Fukuda M, Mima S, Tanabe T, Haniu T, Suzuki Y, Hirata K, Terada S. Endoscopic sonography of the liver--diagnostic application of the echolaparoscope to localize intrahepatic lesions. Scand J Gastroenterol Suppl. 1984;102:24-38. [PubMed] |
| 9. | Okita K, Kodama T, Oda M, Takemoto T. Laparoscopic ultrasonography. Diagnosis of liver and pancreatic cancer. Scand J Gastroenterol Suppl. 1984;94:91-100. [PubMed] |
| 10. | Frank K, Bliesze H, Bönhof JA, Beck K, Hammes P, Linhart P. Laparoscopic sonography: a new approach to intraabdominal disease. J Clin Ultrasound. 1985;13:60-65. [PubMed] [DOI] [Full Text] |
| 11. | John TG, Greig JD, Crosbie JL, Miles WF, Garden OJ. Superior staging of liver tumors with laparoscopy and laparoscopic ultrasound. Ann Surg. 1994;220:711-719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 252] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 12. | Callery MP, Strasberg SM, Doherty GM, Soper NJ, Norton JA. Staging laparoscopy with laparoscopic ultrasonography: optimizing resectability in hepatobiliary and pancreatic malignancy. J Am Coll Surg. 1997;185:33-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 29] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | de Castro SM, Tilleman EH, Busch OR, van Delden OM, Laméris JS, van Gulik TM, Obertop H, Gouma DJ. Diagnostic laparoscopy for primary and secondary liver malignancies: impact of improved imaging and changed criteria for resection. Ann Surg Oncol. 2004;11:522-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Berber E, Garland AM, Engle KL, Rogers SJ, Siperstein AE. Laparoscopic ultrasonography and biopsy of hepatic tumors in 310 patients. Am J Surg. 2004;187:213-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Lo CM, Lai EC, Liu CL, Fan ST, Wong J. Laparoscopy and laparoscopic ultrasonography avoid exploratory laparotomy in patients with hepatocellular carcinoma. Ann Surg. 1998;227:527-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 81] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 16. | Montorsi M, Santambrogio R, Bianchi P, Opocher E, Cornalba GP, Dapri G, Bonavina L, Zuin M, Podda M. Laparoscopy with laparoscopic ultrasound for pretreatment staging of hepatocellular carcinoma: a prospective study. J Gastrointest Surg. 2001;5:312-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Awad SS, Fagan S, Abudayyeh S, Karim N, Berger DH, Ayub K. Preoperative evaluation of hepatic lesions for the staging of hepatocellular and metastatic liver carcinoma using endoscopic ultrasonography. Am J Surg. 2002;184:601-64; discussion 601-64;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 68] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 18. | Ido K, Nakazawa Y, Isoda N, Kawamoto C, Nagamine N, Ono K, Hozumi M, Sato Y, Kimura K, Sugano K. The role of laparoscopic US and laparoscopic US-guided aspiration biopsy in the diagnosis of multicentric hepatocellular carcinoma. Gastrointest Endosc. 1999;50:523-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |