Published online Jul 14, 2005. doi: 10.3748/wjg.v11.i26.4040
Revised: November 10, 2003
Accepted: November 12, 2003
Published online: July 14, 2005
AIM: Irritable bowel syndrome (IBS) is a common disorder and many patients fail to find adequate relief from conventional therapies for their symptoms. This study tests the claim that acupuncture is effective for a majority of these patients.
METHODS: A prospective, blinded, sham acupuncture-controlled trial of traditional Chinese acupuncture was performed at a single postgraduate teaching hospital in Europe. Sixty patients with well-established IBS were recruited. The blinded comparator was sham acupuncture administered by the second of two acupuncturists who alone was aware of the randomization, and who otherwise followed the prescription of the first. The primary end-point was a defined fall in the symptom score at 13 wk (by intention to treat). The prior expectation was a 30% placebo response, and a response rate of 70% from acupuncture, for which the study was adequately powered.
RESULTS: Patients in treated and sham groups improved significantly during the study-mean improvement in scores being equal (minus 1.9) and significant for both (P < 0.05; one-tailed t test). There was a small numeric but non-significant difference between the response rate in patients receiving acupuncture (40.7%) and sham treatment (31.2%). Several secondary end-points marginally favored active treatment, but an improved symptom score of any degree of magnitude occurred more often with sham therapy (65.6% vs 59.2%). For no criterion was statistical significance approached.
CONCLUSION: Traditional Chinese acupuncture is relatively ineffective in IBS in the European hospital setting, and the magnitude of any effect appears insufficient to warrant investment in acupuncture services.
- Citation: Forbes A, Jackson S, Walter C, Quraishi S, Jacyna M, Pitcher M. Acupuncture for irritable bowel syndrome: A blinded placebo-controlled trial. World J Gastroenterol 2005; 11(26): 4040-4044
- URL: https://www.wjgnet.com/1007-9327/full/v11/i26/4040.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i26.4040
Acupuncture has been utilized for a variety of conditions, by up to 19% of the European population, and with as many as 12 million treatments per year in the USA[1]. Gastrointestinal problems are addressed[2], and in addition to publications in the traditional Chinese medicine (TCM) literature there has been support in more mainstream journals[3,4]. Not all reviewers have been so positive however[5]. Irritable bowel syndrome (IBS) is common, and many patients fail to find adequate relief from conventional therapies. It is claimed that acupuncture is effective for a majority of patients with IBS, but there are few data to support this. Case reports do not adequately address the large placebo response in this condition, the often substantial inter-subject variability in response, nor the differing systems of nomenclature in acupuncture. The US NIH consensus did not include IBS amongst 12 conditions for which it found evidence favoring acupuncture[4]. The only paper specific to acupuncture in IBS that we have found is a pilot study of seven patients, which recorded improvements in bloating and general well-being[6]. A complex Austrian study in which acupuncture or sham acupuncture (inter alia) was used for irritable colon demonstrated benefit at 1 mo (43.7% vs 26.7% relief; P < 0.01)[7]. However, the definition of response, the nature of the randomization, and the mechanism of blinding are unclear. Evidence in favor of acupuncture for IBS cannot be considered definite.
Previous attempts to assess the placebo response in acupuncture therapy have been criticized. Orthodox clinician-scientists object to poor blinding, while acupuncturists argue that attempts to blind therapy negate the diagnostic and therapeutic process, and confound the individualization of the chosen regime necessary for the TCM paradigm. The present study addresses a single hypothesis and tackles the issues of methodology in a novel and creative fashion.
Patients were selected by personal approach in the St Mark’s Hospital clinics. Eligibility required a confident clinical diagnosis of IBS and age of over 16 years. Patients were to satisfy the Rome criteria[8] and the Manning criteria[9]. The Rome II criteria[10] became available during the study; their fulfillment was noted but not required. Patients were to have had symptoms for at least 3 mo and to have failed to respond to standard therapies including: increased dietary fiber, reduction of lactose-containing foods, antispasmodics, simple laxatives (in those with predominant constipation), and opioids (in those with predominant diarrhea). Other physical disease was required to be absent or inactive. Formal psychiatric disease was an exclusion criterion. Patients were not permitted to use psychotropic drugs during the study period unless these had been commenced at least 3 mo before recruitment and were maintained at static dose throughout. Potentially fertile women were required to use effective contraception.
Normality of routine hematology, renal, hepatic and thyroid biochemistry, and of inflammatory markers was required. All subjects had a normal sigmoidoscopic examination within 3 mo of entry. Those over 40 years of age were required to have had colonoscopy, or flexible sigmoidoscopy and barium enema within 2 years of entry. All were given an information leaflet and were required to provide written informed consent.
The study was a double blind, sham-controlled trial of TCM acupuncture therapy. Two acupuncturists, fully trained in traditional Chinese acupuncture and accredited to the British Acupuncture Council, were responsible for the active and sham interventions. Recruited patients were allocated according to computer-generated random numbers concealed in sealed envelopes. Ten treatments were administered, at approximately 1-wk intervals.
The first acupuncturist was the “diagnosing acupuncturist” (DA), whom the patient saw for the initial consultation, and before and after each treatment. A full case history was taken by the DA, together with tongue and pulse examination, to arrive at an individual diagnosis in accordance with the principles of TCM, with an additional lesser emphasis on Five Element Acupuncture[11-14]. Although all patients in the study had IBS, this corresponded to a wide range of TCM patterns, making individual diagnosis essential. Dietary and lifestyle advice (important in treatment according to TCM principles) was given to all patients by the DA, who then selected acupuncture points.
The second “treating acupuncturist” (TA) opened the randomization envelope, and for the duration of the study remained the only individual aware of treatment allocation. The TA carried out the treatment-either according to instructions issued by the DA or using sham points, depending on the randomization.
In TCM meridian-based acupuncture the aim is to manipulate or remove blocking of the “Qi”. A variety of needling techniques is necessary, both to achieve requisite ‘deqi’ or ‘needling sensation’, and, subsequently, a range of therapeutic effects. Eight to sixteen needles were inserted at 4-8 specified acupuncture sites, bilaterally, in each session. Needles were left in place momentarily, or for up to 25 min, depending on the desired effect. For active patients the TA implemented the instructions of the DA, including the needle technique, and the length of time of their retention.
‘Sham’ acupuncture points were chosen from three different areas on the body (the anterior thigh distally, the posterior thigh, and the lateral aspect of the lower back), which do not correspond to recognized acupuncture points and are deemed to have no therapeutic value. These were varied to some degree each week as in genuine treatment, including variation in needle technique and length of time of retention. No deqi needling sensation was sought or obtained at sham points.
Sterile single-use ‘Carbo’ brand needles were used (mostly 0.22 mm × 25 mm, some 0.25 mm × 40 mm). Insertion may be uncomfortable but is not normally painful (less discomfort than venepuncture). Needles were generally well tolerated, and were gently stimulated, as required, by the acupuncturist during treatment.
Moxibustion (therapeutic burning of the herb Artemisia vulgaris) is integral to the practice of traditional Chinese acupuncture, but was not used during the study, although there were a number of patients for whom it was considered indicated. This reflected hospital fire regulations and added difficulties with blinding.
The DA re-examined the patients’ pulses at the end of every session, as pulse changes during treatment are considered important indicators of efficacy. On the basis of these, and the verbal, pulse and tongue feedback at the start of the next session, the DA varied the emphasis on different treatment principles and the choice of acupuncture points prescribed for the next treatment.
Patients completed weekly symptom diaries, supplemented by psychological and quality of life scales at entry and at 12th wk (or prior exit). Therapeutic effects were judged from the diaries and questionnaires, and by physician assessment. The symptom diary is based on the Bristol scale[15] and has been previously validated[16]. It employs eight Likert scales relating to abdominal symptomatology and their interference with activities (Appendix), and permits the compilation of a numerical (non-linear) global “symptom score” between 0 and 30. Patients also completed the Hospital Anxiety and Depression (HAD) scale[17], and the EuroQol[18] quality of life questionnaire.
The principal outcome measure was a change in the symptom score. A reduction of four is considered indicative of a clinically useful response, and was expected from sham or placebo therapy in approximately 30% of eligible patients. Acupuncturists expect to obtain a useful response in around 70% of patients with IBS (informal enquiries of several practitioners), with the proviso that limitations imposed by the experimental protocol might reduce this a little.
Secondary outcome measures included assessment by one of the blinded investigators at the end of the study period, which made a simple categorization of patient status as “improved”, “unchanged” or “worse”. Secondary outcomes also included changes on the HAD and EuroQol instruments. As the principal objective is to reduce symptomatology and to improve quality of life, the patients’ perceptions of these are the outcomes of critical interest to them. The end-points recorded are comparable to those utilized in respected studies of this condition.
Statistical calculations for 60 subjects provided for a study with 60% power to demonstrate a 30% numerical (not relative) difference between the two groups, if a placebo response of 30% is assumed. Results were analyzed by intention to treat.
Apart from the hospital notes all data were retained anonymously. The study complied with the requirements of the Declaration of Helsinki (1996 modification), the British Data Protection Act (1984), the International Conference on Harmonization Tripartite Guideline for Good Clinical Practice, and had approval from the Harrow Research Ethics Committee.
Sixty patients (40 female) were recruited; one female withdrew after recruitment but before randomization. Results are therefore recorded for 59 individuals (Table 1). Twenty-eight patients were allocated to acupuncturist A as the DA and to acupuncturist B as the TA, with the converse in the other 31. There was a good balancing of the two groups: for no parameter was there a statistically significant difference at study entry (Table 1).
| Acupuncture group | Sham group | |
| Number | 27 | 32 |
| Number female | 16 | 23 |
| Mean age (yr) | 43.0 | 44.4 |
| Age range (yr) | 19-67 | 17-79 |
| Predominant symptom | ||
| Pain | 11 | 10 |
| Bloating | 7 | 11 |
| Diarrhea | 7 | 9 |
| Constipation | 2 | 2 |
| Mean symptom score | 13.5 | 13.1 |
| Mean anxiety score (HAD) | 10.2 | 11.2 |
| Mean depression score (HAD) | 5.8 | 6.8 |
| Mean EuroQol LAS score (%) | 59 | 64 |
Role of sponsors: None in either design of the study or in the writing of the report.
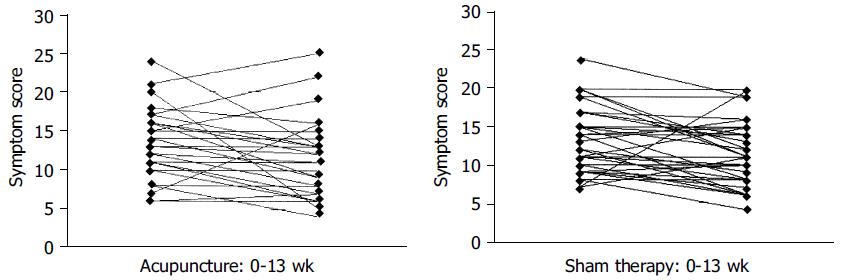
The mean global symptom score in the acupuncture-treated patients fell from 13.5 ± 4.51 to 11.6 ± 5.13, and in the sham group from 13.1 ± 4.30 to 11.2 ± 4.17 (P < 0.05 for one-tailed t test for the improvements in both study groups) (Figure 1). A reduction in symptom score was observed in 16 acupuncture subjects (59.2%), and by at least four points in 11 (40.7%). The equivalent figures for the sham group were 21 (65.6%) and 10 (31.2%). The differences between sham and actively treated groups did not approach statistical significance.
The blinded clinician considered 13 of the acupuncture group (48.1%) improved, compared to 10 of the sham group (31.2%) (NS). These were predominantly the same patients who considered themselves improved (reduction in symptom score of four or more). Similar proportions in the two groups were considered to have deteriorated or had withdrawn (18.5% vs 21.9%; NS).
For those with pain predominance at enrollment the median score of 13 remained at 13 in the actively treated group, and fell from 15 to 10 in the sham group; for bloating the equivalent figures were 14 to 9, and 14 to 11; for diarrhea 11 to 8 compared to 11 to 10.5; and for constipation 16 to 15 vs 11 to 8.
There were no significant differences between the HAD scores for the sham and active groups, but a slightly higher proportion of the sham-treated group had anxiety scores in the “probable” (≥ 12) range (47% vs 41%). The response rate (drop of ≥ 4 symptom points) was 27% in the subset of anxious patients receiving sham treatment and 54% in those on active therapy (NS).
The EuroQol score rose slightly (improvement) in the actively treated (59.4-64.6%) and the sham treated (64.6-65.6%); neither change was significant. There was no correlation between initial EuroQol score and the likelihood of a response.
Acupuncturist A (as TA) treated 31 patients, of whom 19 were allocated to sham therapy. Their mean score of 13.6 ± 4.84 fell to 12.3 ± 4.56; the score fell by ≥ 4 in 7 (36.8%). In the 12 patients who received active acupuncture the mean score fell from 14.3 ± 4.68 to 11.6 ± 6.69, with a fall of ≥ 4 in 6 (50%). Acupuncturist B (as TA) treated 28 patients of whom 13 were allocated to sham; the score fell by ≥ 4 in 3 (23.1%) of these. In the 15 patients randomized to active acupuncture a “qualifying” fall in score occurred in 5 (33.3%). Overall 41.9% of patients “diagnosed” by acupuncturist B and “treated” by acupuncturist A responded with a qualifying fall in score, compared to 28.6% of those with the acupuncturists filling the alternative roles (NS).
No direct adverse events were elicited. One patient was commenced on antidepressants after psychiatric consultation, and another on beta-blockers for anxiety. Six other patients failed to complete the study period. Of these eight withdrawals, five belonged to the acupuncture group and three to sham. These patients have been included in the above analyses by intention to treat. If the principal outcome measure is applied only to those completing the intended therapy the results are unchanged: the mean symptom score at completion of the acupuncture course was 11.4 compared to 10.9 in the sham group (NS).
As expected there was a response to TCM acupuncture and to sham treatment. The number of responding patients in the sham group and the magnitude of the responses were in line with our prior expectations (31.2% good responders compared to an anticipated 30% placebo response). The study group is therefore likely to be generally representative. Formal acupuncture failed to elicit significant advantage (40.7% responders). There were several areas in which numeric advantage lay with acupuncture, including the clinician’s assessment and the proportion achieving at least a four point reduction in symptom score, but sham therapy had the numeric advantage if responses of any degree of magnitude are included (65.6% vs 59.2%). There was no obvious trend according to predominant symptom at study entry, but initial anxiety possibly predicts a better response.
The inference that TCM acupuncture is of very limited value in IBS is supported by the absence of positive data in the literature, its absence from the conclusions of the NIH consensus[4], and from a small study which showed no effect on colonic motility in constipation[19]. We are confident that our sham technique was performed with retention of complete blinding of the DA, the gastroenterologist and the patient. This necessarily unblinded nature of the treating acupuncturist clearly had important effects on the two practitioners concerned, who felt uncomfortable “deliberately denying” the patient, a therapy in which they had confidence. It is possible that this proved a confounding factor. The close similarity of the outcome from sham therapy to that expected from placebo suggests that neither positive nor negative effects predominate. In consequence, it is not clear that anything would have been gained by the use of sham needles, as has been advocated[20], since while this strategy has the potential to conceal sham administration from the TA it may unblind the patient. It is acknowledged that the use of sham needling probably elicits important physiological effects (such as increased endorphin activation), but the absence of an obvious difference in response rate in our sham group from that anticipated from “other” placebos indicates that the effect is not one of lasting clinical consequence.
The combination of acupuncturist B as diagnostician with acupuncturist A as acupuncturist appeared “better” than the converse. This was probably a direct consequence of the individualization of therapy (by the TA as well as that planned by the DA), but represents a post hoc and non-significant observation. We deliberately chose to permit both acupuncturists to engage in therapy so as to increase the generalizability of the study, hence avoiding results dependent on the consequences of a unique pairing of practitioners.
The outcome may have included systematic bias against acupuncture. The specific dietary and lifestyle advice considered important to TCM was given to all patients regardless of randomization. It is unlikely that this was a major influence as the sham response was closely similar to that expected for placebo. The proscription of moxibustion would be expected to have placed the actively treated group at a disadvantage compared to those treated outside the study context. However, this technique cannot easily be a practical proposition in health service premises in which fire regulations and the presence of smoke detectors are ubiquitous. The third factor potentially disadvantageous to acupuncture therapy was the impossibility of completely individualized therapy in a formal trial, and perhaps adverse influences from other constraints of the hospital environment. This drawback was considered carefully during the devising of the study and felt to be an acceptable compromise between Western scientific method and traditional Chinese practice. The possibility that simplified acupuncture as delivered by Western-medicine-trained acupuncturists might have given a different result is intriguing and may warrant further study.
The study was underpowered to demonstrate a small benefit, but it was of sufficient size to confirm the large difference that was anticipated. If such an effect has been missed by the present study it is our opinion that it is of insufficient clinical relevance to justify de novo investment in provision of acupuncture services to hospital patients with IBS.
We are also grateful for the support of our research nurses, to the clinicians who referred patients to us, and to the patients themselves. We greatly appreciate the very useful comments of Dr. Andrew Thillainayagam, MD, FRCP (medically trained acupuncturist), on an earlier draft of the manuscript.
Science Editor Wang XL and Guo SY Language Editor Elsevier HK
| 1. | Fisher P, Ward A. Complementary medicine in Europe. BMJ. 1994;309:107-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 501] [Cited by in RCA: 463] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 2. | Eskinazi DP, Jobst KA. National Institutes of Health Office of Alternative Medicine-Food and Drug Administration Workshop on Acupuncture. J Altern Complement Med. 1996;2:3-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Li Y, Tougas G, Chiverton SG, Hunt RH. The effect of acupuncture on gastrointestinal function and disorders. Am J Gastroenterol. 1992;87:1372-1381. [PubMed] |
| 4. | NIH Consensus Conference. Acupuncture. JAMA. 1998;280:1518-1524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 708] [Cited by in RCA: 626] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 5. | Mayer DJ. Acupuncture: an evidence-based review of the clinical literature. Annu Rev Med. 2000;51:49-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 104] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 6. | Chan J, Carr I, Mayberry JF. The role of acupuncture in the treatment of irritable bowel syndrome: a pilot study. Hepatogastroenterology. 1997;44:1328-1330. [PubMed] |
| 7. | Kunze M, Seidel HJ, Stübe G. [Comparative studies of the effectiveness of brief psychotherapy, acupuncture and papaverin therapy in patients with irritable bowel syndrome]. Z Gesamte Inn Med. 1990;45:625-627. [PubMed] |
| 8. | Thompson WG, Dotevall G, Drossman DA, Heaton KW, Kruis W. Irritable bowel syndrome: guidelines for the diagnosis. Gastroenterol Int. 1989;2:92-95. |
| 9. | Manning AP, Thompson WG, Heaton KW, Morris AF. Towards positive diagnosis of the irritable bowel. Br Med J. 1978;2:653-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 966] [Cited by in RCA: 963] [Article Influence: 20.5] [Reference Citation Analysis (3)] |
| 10. | Drossman DA, Li Z, Andruzzi E, Temple RD, Talley NJ, Thompson WG, Whitehead WE, Janssens J, Funch-Jensen P, Corazziari E. U.S. householder survey of functional gastrointestinal disorders. Prevalence, sociodemography, and health impact. Dig Dis Sci. 1993;38:1569-1580. [PubMed] |
| 11. | Deadman P. A Manual of Acupuncture. J Chinese Med Publications. 1998;. |
| 12. | Maciocia G. The Foundations of Chinese Medicine. Churchill Livingstone. 1989;. |
| 13. | Maciocia G. The Practice of Chinese Medicine. Churchill Livingstone. 1994;. |
| 14. | Mole P; Energy Balancing for Body, Mind & Spirit. . |
| 15. | Heaton KW, Ghosh S, Braddon FE. How bad are the symptoms and bowel dysfunction of patients with the irritable bowel syndrome? A prospective, controlled study with emphasis on stool form. Gut. 1991;32:73-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 174] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 16. | Forbes A, MacAuley S, Chiotakakou-Faliakou E. Hypnotherapy and therapeutic audiotape: effective in previously unsuccessfully treated irritable bowel syndrome? Int J Colorectal Dis. 2000;15:328-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 43] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28548] [Cited by in RCA: 31825] [Article Influence: 757.7] [Reference Citation Analysis (0)] |
| 18. | Johnson JA, Coons SJ. Comparison of the EQ-5D and SF-12 in an adult US sample. Qual Life Res. 1998;7:155-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 244] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 19. | Klauser AG, Rubach A, Bertsche O, Müller-Lissner SA. Body acupuncture: effect on colonic function in chronic constipation. Z Gastroenterol. 1993;31:605-608. [PubMed] |
| 20. | Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet. 1998;352:364-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 658] [Cited by in RCA: 643] [Article Influence: 23.8] [Reference Citation Analysis (0)] |