Published online Jan 14, 2005. doi: 10.3748/wjg.v11.i2.200
Revised: April 21, 2004
Accepted: May 9, 2004
Published online: January 14, 2005
AIM: The purpose of this study was to compare the diagnostic accuracy of biphasic multi-detector row helical computed tomography (MDCT), digital subtraction angiography (DSA) and Lipiodol computed tomography (CT) in detection of hypervascular hepatocellular carcinoma (HCC).
METHODS: Twenty-eight patients with nodular HCC underwent biphasic MDCT examination: hepatic arterial phase (HAP) 25 s and portal venous phase (PVP) 70 s after injection of the contrast medium (1.5 mL/kg). They also underwent hepatic angiography and intra-arterial infusion of iodized oil. Lipiodol CT was performed 3-4 wk after infusion. MDCT images were compared with DSA and Lipiodol CT images for detection of hepatic nodules.
RESULTS: The three imaging techniques had the same sensitivity in detecting nodules >20 mm in diameter. There was no significant difference in the sensitivity among HAP-MDCT, Lipiodol CT and DSA for nodules of 10-20 mm in diameter. For the nodules <10 mm in diameter, HAP-MDCT identified 47, Lipiodol CT detected 27 (χ2 = 11.3, P = 0.005<0.01, HAP-MDCT vs Lipiodol CT) and DSA detected 16 (χ2 = 9.09, P = 0.005<0.01 vs Lipiodol CT and χ2 = 29.03, P = 0.005<0.01vs HAP-MDCT). However, six nodules <10 mm in diameter were detected only by Lipiodol CT.
CONCLUSION: MDCT and Lipiodol CT are two complementary modalities. At present, MDCT does not obviate the need for DSA and subsequent Lipiodol CT as a preoperative examination for HCC.
- Citation: Zheng XH, Guan YS, Zhou XP, Huang J, Sun L, Li X, Liu Y. Detection of hypervascular hepatocellular carcinoma: Comparison of multi-detector CT with digital subtraction angiography and Lipiodol CT. World J Gastroenterol 2005; 11(2): 200-203
- URL: https://www.wjgnet.com/1007-9327/full/v11/i2/200.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i2.200
Hepatocellular carcinoma (HCC) is one of the most common malignancies in the world, causing an estimated one million deaths annually. In China, HCC has ranked second in cancer mortality since 1 990s[1]. It has a poor prognosis due to its rapid infiltrating growth and complicating liver cirrhosis. Surgical resection, liver transplantation and cryosurgery are considered the best curative options, achieving a high rate of complete response, especially in patients with small HCC and good residual liver function. Moreover, nonsurgical, regional interventional therapies have led to a major breakthrough in the management of unresectable HCC, which include transarterial chemoembolization (TACE), percutaneous ethanol injection (PEI), radiofrequency ablation (RFA), microwave coagulation therapy (MCT), laser-induced thermotherapy (LITT) and other biotherapies.
Liver resection remains a good treatment for HCC in patients with cirrhosis. Satisfactory results have been obtained in patients with small, non-invasive tumors[2]. However, only a small number of patients are suitable for curative resection due to many factors such as multicentric tumors, intrahepatic metastases, early vascular invasion, coexisting advanced liver cirrhosis and comorbidities[3]. Liver transplantation seems to be the choice for monofocal HCC less than 5 cm in diameter and in selected cases of plurifocal HCC[4]. Therefore, accurate evaluation of intrahepatic metastases, or daughter nodules, is important to determine appropriate treatment for the disease. Because the prognosis after surgical treatment depends on the initial staging, performance of the most accurate preoperative evaluation is crucial. The main difficulty for diagnosis and staging of HCC resides in the detection of small nodular lesions (including intrahepatic metastases and multicentric tumors). Underestimation of these lesions may lead to inappropriate surgical resection. Therefore, accurate preoperative imaging evaluation of HCC nodules is essential for selecting appropriate patients for surgical intervention and for determining the extent of hepatoectomy.
It has been recognized that the majority of HCCs are hypervascular. During the hepatic arterial phase (HAP), hypervascular lesions are greatly enhanced, and become iso- or hypodense in the portal venous phase (PVP), which is a sensitive and specific feature for diagnosing HCC. A biphasic hepatic acquisition helical CT scanning technique has become a standard method for clinical diagnosis of HCC[5-10]. Meanwhile, hepatic angiography is widely used as an imaging technique for HCC. Moreover, Lipiodol CT, which involves CT after intrahepatic arterial injection of iodized oil, has been reported to be the most sensitive preoperative imaging modality for HCC, especially in detecting intrahepatic metastastic nodules[11-13].
Recently, a new generation of multi-detector row helical CT (MDCT) has been used in clinical practice. It is a technologic advance that allows the simultaneous acquisition of multiple images during a single rotation of the X-ray tube. The scanning time can be shortened to 0.5 s. If the 16-detector array CT scanner is used, the entire hepatic acquisition can be accomplished in a very short period of time (4-8 s). Reformations provide a unique perspective to view the liver, and may improve diagnostic capacity[14]. However, consensus has not been reached as to whether biphasic MDCT obviates the need for other invasive imaging modalities such as digital subtraction angiography (DSA) and Lipiodol CT.
The purpose of this study was to compare the diagnostic accuracy of biphasic MDCT, DSA and Lipiodol CT in detection of hypervascular HCC.
From January 2003 to February 2004, 28 patients (24 men, 4 women, mean age 49 years) with nodular HCC were enrolled in this study. The diagnosis was based on the results of percutaneous needle biopsy (n = 12) and operation (n = 2) or test of the serum alpha-fetoprotein levels in combination with imaging appearance and follow-up images (n = 14) according to the diagnostic criteria for HCC formulated by Chinese National Association of Anticancer Committee (1999).
MDCT scans of liver were performed with Sensation16 CT scanner (Siemens Medical System, Germany) using the following parameters: 0.5 s scanning time, 5-μm-thick section, 24 mm/s table speed, 120 KVP and 140 mA .
Before examination, 800-1000 mL water was taken as an oral contrast. The patients underwent unenhanced and biphasic helical CT scanning as follows. First, patients were imaged with a helical MDCT scanner in a cranial-caudal direction beginning at top of the liver. Then, nonionic contrast medium (Ultravist 300, Schering Pharmaceutical Lt., Guangzhou, China) was administered at a dose of 1.5 mL/kg and an injection rate of 3 mL/s via the antecubital vein. Biphase acquisition was performed with a scanning delay set for HAP and PVP at 25 s and 70 s, respectively. Each of the whole liver scanning by cephalad-caudal orientation was completed in 4-8 s with breath held.
The DSA procedure was obtained with a digital angiographic system (AXIOM Artis FA, Siemens Medical System, Germany). Under local anesthesia, the focal segmental or sub-segmental artery was detected carefully by celiac arteriography, and variants were excluded by superior mesenteric arteriography and phrenic arteriography. When the tip of the catheter arrived at the appropriate focal artery, 30-40 mL of the contrast medium (Ultravist 300, Schering Pharmaceutical Lt., Guangzhou, China) was injected at about 6-8 mL/s. After angiography was performed, 8-15 mL iodized oil (Huaihai Pharmaceutical Factory, Shanghai, China) was dripped through the 5-Fr catheter under fluoroscopic monitoring. CT examination of the liver was performed within 3 to 4 wk after intra-arterial injection of iodized oil to evaluate areas of Lipiodol retention.
The images for each radiological method were interpreted in conference by at least two attending radiologists who were unaware of the results of previously performed imaging studies. The HAP and PVP of MDCT images were evaluated in separate sessions, thus keeping the readers unaware of the results of the other phase. Images of each phase were compared at the same hepatic window settings throughout the liver. Images were evaluated to determine lesion size, number, and detectability. Because detectability represents a subjective determination of the ease of visualization of a nodule, detectability depends on the attenuation of the tumor and the liver and the presence of a tumor capsule. Biphasic MDCT scans were compared with DSA and Lipiodol CT scans.
To compare the various techniques, Chi-square test was performed, and P values less than 0.05 were considered statistically significant.
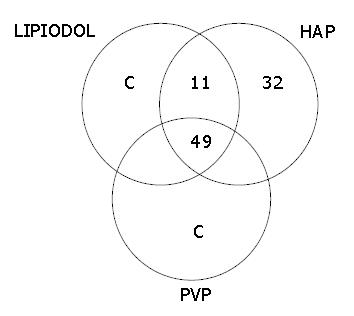
The results are summarized in Table 1 and Figure 1. A total of 98 nodules were detected in 28 patients by at least one modality. Two patients had one nodule, four had two nodules, 10 had three nodules, and 12 had four or more nodules. The mean number of HCC nodules per patient was 3.5.
| Tumor Size (mm) | MDCT | Lipiodol CT | DSA | |
| HAP | PVP | |||
| <10 mm | 47 | 11 | 27 | 16 |
| 10-20 mm | 19 | 14 | 13 | 11 |
| >20 mm | 26 | 24 | 26 | 26 |
| Total | 92 | 49 | 66 | 53 |
Lipiodol CT detected one or more hepatic nodules in 26 of 28 patients for a total 66 nodules. In the remaining 2 patients with negative Lipiodol CT, HAP-MDCT detected 2 nodules. MDCT identified 92 hepatic nodules, HAP-MDCT detected all while PVP-MDCT detected only 49 of these nodules (Table 1). None of the 53 nodules detected by DSA was missed using either Lipiodol CT or HAP-MDCT. When data obtained with Lipiodol CT were compared with those of MDCT, 60 nodules were detected by both techniques, 6 were detected only by Lipiodol CT, and 32 were detected only by HAP-MDCT (Figure 1).
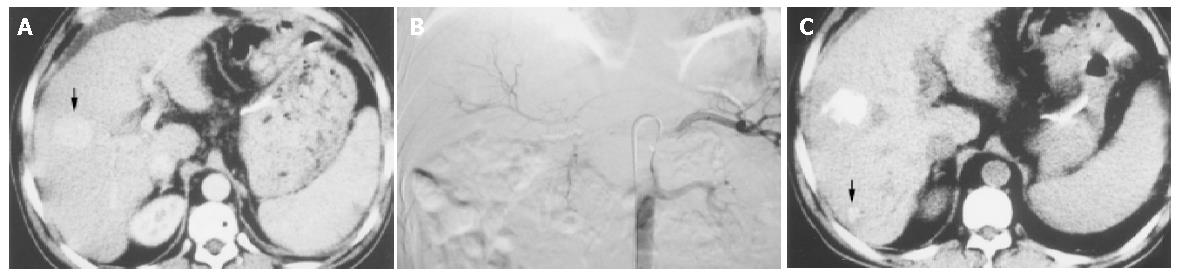
The three imaging techniques used in this study (MDCT, DSA, Lipiodol CT) had the same sensitivity in detecting nodules >20 mm in diameter since the 26 nodules >20 mm in diameter were detected by DSA as well as HAP-MDCT and Lipiodol CT. MDCT and Lipiodol CT were also comparable in detection of nodules with diameters of 10-20 mm in diameter. In fact, 19 of these nodules were seen by HAP-MDCT (14 by PVP-MDCT), and 13 by Lipiodol CT. For nodules < 10 mm in diameter, HAP-MDCT identified 47 nodules, Lipiodol CT showed 27 including the six nodules not detected by MDCT (HAP-MDCT vs Lipiodol CT: χ2 = 11.3, P = 0.005<0.01), DSA showed 16 (χ2 = 9.09, P = 0.005<0.01, vs Lipiodol CT and χ2 = 29.03, P = 0.005<0.01,vs HAP-MDCT) and PVP showed 11 ( Figures 2, 3).
In preoperative evaluation of hepatic tumors, the imaging studies used must be highly sensitive and specific for the detection of malignant neoplasms to enable the selection of appropriate surgical candidates and avoid unnecessary surgery. Several authors have evaluated the accuracy of Lipiodol CT imaging in detecting HCC nodules. They used histologic assessment of liver biopsy specimens, liver parenchyma taken by partial liver resection, or explanted liver at the time of liver transplantation as references and have reported a wide variety of sensitivities (40% to >90%)[12,15-21]. Still, the question of whether Lipiodol CT provides information beyond that obtained with other noninvasive modalities, as preoperative evaluation in the era of MDCT, remains to be addressed. In recent years, a few studies[14,22-25] have evaluated the role of multiphasic scanning by MDCT in detecting small hypervascular HCC. They have drawn a conclusion that the utility of faster speed and thinner slice (6 mm) MDCT can improve the detectability of hypervascular small HCC, and additional early arterial phase imaging does not improve the detection of HCC compared with biphasic CT images. With these in mind, we reviewed the experience with DSA, Lipiodol CT and biphasic MDCT performed at our institution.
It has been known that the imaging techniques for detection and staging of HCC take advantages of two basic events: 1) the disappearance of portal vessels, which are substituted with arterial vessels; and 2) a progressive disappearance of the reticuloendothelial system (RES)[26]. The latter has been exploited by Lipiodol CT: the iodized oil that reaches the hepatic parenchyma via the hepatic artery is eliminated within 3-4 wk by Kuppfer cells, but not by neoplastic nodules, which can be easily detected by performing a second CT scan 3-4 wk later. Unfortunately, this technique gives both false positive and false negative results. False positive results are due to the persistence of Lipiodol in non-neoplastic areas of the liver due to an altered RES, within angiomas, or at the site of a previous liver biopsy[27]. False negative results are due to the presence of neoplastic foci not reached by Lipiodol and/or tracer eliminated from the foci. In the current investigation, false negative results were more frequent in the case of small neoplastic nodules (<2 cm)[15,17]. The phenomenon may attribute to a greater degree of differentiation of these small HCC nodules, with persistence of some reticuloendothelial cells, less developed arterial vascularization, or both.
MDCT focuses on the other main characteristic of HCC, which is the development of new arterial vascularization, probably an earlier phenomenon than the disappearance of RES. The results of this study clearly indicate that MDCT has a remarkably greater sensitivity than DSA and Lipiodol CT in detecting small neoplastic nodules (<20 mm). The advantage of MDCT scan is mainly due to the possibility of imaging the liver in the arterial phase, as demonstrated by the comparison between HAP and PVP.
In this study, all 28 patients had at least one overt HCC. We defined the largest lesions as the main lesions, while called the other lesions as small nodular lesions (including intrahepatic metastases and multicentric tumors). It is not possible to discriminate completely between daughters (i.e., intrahepatic metastatic) and multicentric tumors based solely on imaging or pathologic findings. However, it is generally accepted that a tumor becomes less differentiated (i.e., well to moderately or poorly) as its size increases, whereas daughter nodules are small but their grade of differentiation is moderate to poor[12]. In light of these considerations, the present results strongly suggest that MDCT is superior to Lipiodol CT in delineating early HCC nodules, but the latter method is superior for detecting intrahepatic metastatic lesions.
This study has limitations. Firstly, histologic confirmation of each nodule was not obtained, not allowing a precise CT-histopathologic correlation of each nodule, although we performed biopsy on the main lesion in some patients. Specificity was not confirmed, but a combination of the clinical course, laboratory values, and imaging appearance is believed to be sufficient for a presumptive diagnosis of hypervascular HCC nodules. On the other hand, ultrasound or CT-guided needle biopsy is less sensitive than imaging in the detection of this kind of malignancy (75% of needle biopsy vs 97% of imaging), as needle sampling involves only a small part of the lesion, and this may not include the area of neoplastic degeneration. Secondly, some lesions might be missed by all three imaging techniques used in this study since there is a possibility that the three techniques do not have 100% sensitivity for the detection of nodular HCC. Consequently, we could not obtain the true sensitivity, specificity, and accuracy of the three techniques. However, Torzilli et al reported that the respective accuracy, sensitivity, specificity, and positive and negative predictive values were 99.6%, 100%, 98.9%, 99.3%, and 100% for diagnosis of HCC using a combination of ultrasonography, spiral CT, angiography, magnetic resonance imaging (MRI), and Lipiodol CT. Thirdly, hypovascular HCC cases were excluded because of the difficult verification of these tumors by the methods we used. Although this type of HCC is not common, the overall detectability of nodular HCC cannot be estimated.
Further studies based on accurate follow-up of patients with HCC or a pathologic correlation with livers studied at surgery or autopsy are needed to clarify the nature of hepatic nodules detected with the three techniques.
From the present study, we conclude that biphasic MDCT and Lipiodol CT appear to be complementary, although the overall ability of biphasic MDCT scan to detect hypervascular HCC nodules is superior to that of Lipiodol CT. At present, MDCT does not obviate the need for DSA and subsequent Lipiodol CT as a preoperative examination for HCC. In addition, intra-arterial infusion of iodized oil can be also used for therapy.
Edited by Xia HHX and Wang XL Proofread by Ma JY
| 1. | Tang ZY. Hepatocellular carcinoma--cause, treatment and metastasis. World J Gastroenterol. 2001;7:445-454. [PubMed] |
| 2. | Franco D, Usatoff V. Resection of hepatocellular carcinoma. Hepatogastroenterology. 2001;48:33-36. [PubMed] |
| 3. | Alsowmely AM, Hodgson HJ. Non-surgical treatment of hepatocellular carcinoma. Aliment Pharmacol Ther. 2002;16:1-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Colella G, Bottelli R, De Carlis L, Sansalone CV, Rondinara GF, Alberti A, Belli LS, Gelosa F, Iamoni GM, Rampoldi A. Hepatocellular carcinoma: comparison between liver transplantation, resective surgery, ethanol injection, and chemoembolization. Transpl Int. 1998;11 Suppl 1:S193-S196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 49] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Baron RL, Oliver JH, Dodd GD, Nalesnik M, Holbert BL, Carr B. Hepatocellular carcinoma: evaluation with biphasic, contrast-enhanced, helical CT. Radiology. 1996;199:505-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 285] [Cited by in RCA: 258] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 6. | Oliver JH, Baron RL, Federle MP, Rockette HE. Detecting hepatocellular carcinoma: value of unenhanced or arterial phase CT imaging or both used in conjunction with conventional portal venous phase contrast-enhanced CT imaging. AJR Am J Roentgenol. 1996;167:71-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 103] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 7. | Oliver JH, Baron RL. Helical biphasic contrast-enhanced CT of the liver: technique, indications, interpretation, and pitfalls. Radiology. 1996;201:1-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 161] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 8. | Oliver JH, Baron RL, Federle MP, Jones BC, Sheng R. Hypervascular liver metastases: do unenhanced and hepatic arterial phase CT images affect tumor detection? Radiology. 1997;205:709-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 81] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 9. | Paulson EK, McDermott VG, Keogan MT, DeLong DM, Frederick MG, Nelson RC. Carcinoid metastases to the liver: role of triple-phase helical CT. Radiology. 1998;206:143-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 118] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 10. | Mitsuzaki K, Yamashita Y, Ogata I, Nishiharu T, Urata J, Takahashi M. Multiple-phase helical CT of the liver for detecting small hepatomas in patients with liver cirrhosis: contrast-injection protocol and optimal timing. AJR Am J Roentgenol. 1996;167:753-757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 113] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 11. | Bartolozzi C, Lencioni R, Caramella D, Palla A, Bassi AM, Di Candio G. Small hepatocellular carcinoma. Detection with US, CT, MR imaging, DSA, and Lipiodol-CT. Acta Radiol. 1996;37:69-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Lencioni R, Pinto F, Armillotta N, Di Giulio M, Gaeta P, Di Candio G, Marchi S, Bartolozzi C. Intrahepatic metastatic nodules of hepatocellular carcinoma detected at lipiodol-CT: imaging-pathologic correlation. Abdom Imaging. 1997;22:253-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 50] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Itai Y. Lipiodol-CT for hepatocellular carcinoma. Abdom Imaging. 1997;22:259-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Wong K, Paulson EK, Nelson RC. Breath-hold three-dimensional CT of the liver with multi-detector row helical CT. Radiology. 2001;219:75-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 49] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Veltri A, Robba T, Anselmetti GC, Martina MC, Regge D, Grosso M, Fava C. Computerized tomography with lipiodol in hepatocarcinoma. Assessment of its diagnostic accuracy with anatomo-pathological control. Radiol Med. 1998;96:81-86. |
| 16. | Bizollon T, Rode A, Bancel B, Gueripel V, Ducerf C, Baulieux J, Trepo C. Diagnostic value and tolerance of Lipiodol-computed tomography for the detection of small hepatocellular carcinoma: correlation with pathologic examination of explanted livers. J Hepatol. 1998;28:491-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 38] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Spreafico C, Marchianò A, Mazzaferro V, Frigerio LF, Regalia E, Lanocita R, Patelli G, Andreola S, Garbagnati F, Damascelli B. Hepatocellular carcinoma in patients who undergo liver transplantation: sensitivity of CT with iodized oil. Radiology. 1997;203:457-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 37] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Valls C, Figueras J, Jaurrieta E, Sancho C, Dominguez J, Benasco C, Moreno P, Rafecas A, Virgili J, Castellsagué X. Hepatocellular carcinoma: iodized-oil CT TNM classification. AJR Am J Roentgenol. 1996;167:477-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Taourel PG, Pageaux GP, Coste V, Fabre JM, Pradel JA, Ramos J, Larrey D, Domergue J, Michel H, Bruel JM. Small hepatocellular carcinoma in patients undergoing liver transplantation: detection with CT after injection of iodized oil. Radiology. 1995;197:377-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 41] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Bhattacharya S, Dhillon AP, Rees J, Savage K, Saada J, Burroughs A, Rolles K, Davidson B. Small hepatocellular carcinomas in cirrhotic explant livers: identification by macroscopic examination and lipiodol localization. Hepatology. 1997;25:613-618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Saada J, Bhattacharya S, Dhillon AP, Dick R, Burroughs AK, Rolles K, Davidson BR. Detection of small hepatocellular carcinomas in cirrhotic livers using iodised oil computed tomography. Gut. 1997;41:404-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 22. | Laghi A, Iannaccone R, Rossi P, Carbone I, Ferrari R, Mangiapane F, Nofroni I, Passariello R. Hepatocellular carcinoma: detection with triple-phase multi-detector row helical CT in patients with chronic hepatitis. Radiology. 2003;226:543-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 90] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 23. | Ichikawa T, Kitamura T, Nakajima H, Sou H, Tsukamoto T, Ikenaga S, Araki T. Hypervascular hepatocellular carcinoma: can double arterial phase imaging with multidetector CT improve tumor depiction in the cirrhotic liver? AJR Am J Roentgenol. 2002;179:751-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 61] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 24. | Kawata S, Murakami T, Kim T, Hori M, Federle MP, Kumano S, Sugihara E, Makino S, Nakamura H, Kudo M. Multidetector CT: diagnostic impact of slice thickness on detection of hypervascular hepatocellular carcinoma. AJR Am J Roentgenol. 2002;179:61-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 55] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 25. | Kim SK, Lim JH, Lee WJ, Kim SH, Choi D, Lee SJ, Lim HK, Kim H. Detection of hepatocellular carcinoma: comparison of dynamic three-phase computed tomography images and four-phase computed tomography images using multidetector row helical computed tomography. J Comput Assist Tomogr. 2002;26:691-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 26. | Choi BI, Takayasu K, Han MC. Small hepatocellular carcinomas and associated nodular lesions of the liver: pathology, pathogenesis, and imaging findings. AJR Am J Roentgenol. 1993;160:1177-1187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 115] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 27. | Veltri A, Robba T, Anselmetti GC, Martina MC, Regge D, Grosso M, Fava C. Computerized tomography with lipiodol in hepatocarcinoma. Assessment of its diagnostic accuracy with anatomo-pathological control. Radiol Med. 1998;96:81-86. [PubMed] |