Published online Mar 15, 2004. doi: 10.3748/wjg.v10.i6.847
Revised: October 23, 2003
Accepted: December 16, 2003
Published online: March 15, 2004
AIM: Quasispecies of hepatitis C virus (HCV) are the foundation for rapid sequence evolution of HCV to evade immune surveillance of hosts. The consensus sequence evolution of a segment of HCV NS3 region, which encompasses putative cytotoxic T cell epitopes, was evaluated.
METHODS: Three male patients, infected with HCV through multiple transfusions, were identified from clinical symptoms and monitored by aminotransferase for 60 months. Blood samples taken at months 0, 32, and 60 were used for viral RNA extraction. A segment of HCV NS3 region was amplified from the RNA extraction by RT-PCR and subjected to subcloning and sequencing. HLA types of these three patients were determined using complement-dependent microlymphocytotoxic assay. CTL epitopes were predicted using MHC binding motifs.
RESULTS: No patient had clinical symptoms or elevation of aspartate/alanine aminotransferase. Two patients showed positive HCV PCR results at all 3 time points. The other one showed a positive HCV PCR result only at month 0. A reported HLA-A2-restricted CTL epitope had no alteration in the HLA-A2-negative carrier over 60 months. In the HLA-A2-positive individuals, all the sequences from 0 month 0 showed an amber mutation on the initial codon of the epitope. Most changes of consensus sequences in the same patient occurred on predicted cytotoxic T cell epitopes.
CONCLUSION: Amber mutation and changes of consensus sequence in HCV NS3 region may be related to viral immune escape.
- Citation: Guo HZ, Yin Y, Wang WL, Zhang CS, Wang T, Wang Z, Zhang J, Cheng H, Wang HT. Sequence evolution of putative cytotoxic T cell epitopes in NS3 region of hepatitis C virus. World J Gastroenterol 2004; 10(6): 847-851
- URL: https://www.wjgnet.com/1007-9327/full/v10/i6/847.htm
- DOI: https://dx.doi.org/10.3748/wjg.v10.i6.847
Hepatitis C virus (HCV) is one of the main pathogens of transfusion-associated hepatitis. After acute transfusion-associated HCV infection, about 70-80% of the patients may progress to chronicity. Although many patients with chronic hepatitis C have no symptoms, cirrhosis may develop in 20% within 10 to 20 years after acute infection. The risk for hepatocellular carcinoma is increased in patients with chronic hepatitis C and almost exclusively in patients with cirrhosis[1-15].
HCV is a linear, single-stranded positive-sense, 9400-nucleotide RNA virus. HCV constitutes its own genus in the family Flaviviridae. The HCV genome contains a single large open reading frame that codes for a virus polyprotein of approximately 3000 amino acids. Due to the high mutation rate of RNA dependent RNA polymerase, there are genotype and quasispecies diversity of HCV[16-19]. The high mutation rate may interfere with effective immunity and cause the progression to chronicity[20,21].
Of the components of adaptive immunity, cytotoxic T cells play an important role in eliminating intracellular infections[22]. They recognize body cells infected with viruses by detecting peptide fragments derived from viruses bound to MHC class I molecules on the infected body cells. Then, they kill the infected cells before viral replications complete. In this study, 3 patients with transfusion-associated hepatitis C were followed-up for 60 mo to evaluate the evolution of cytotoxic T cell epitopes in the HCV NS3 region.
Patients C, Z and W, being 43, 48 and 49 years old Chinese males, were infected with HCV through multiple transfusions. They were followed-up for 60 mo after identification. During the follow-up period, no elevation of aspartate/alanine aminotransferase was found. Their peripheral blood was collected at mo 0 (the time of identification), 32 and 60, and stored at -70 °C. Patients C and Z were positive for HCV RNA. Patient W was positive for HCV RNA only in the blood sample taken at mo 0 and consistently negative after that.
HLA types of the three patients were assessed by using the Tasaki HLA class I dry tissue typing tray (One Lambda, Canoga Park, CA). Briefly, blood samples were drawn and lymphocytes were isolated immediately. After antibody and 2 × 106 lymphocytes were mixed in each well, 1 μL of complement was added into each well to incubate at room temperature for 1 hour. After incubation, the cells were stained with eosin and fixed with formaldehyde. Positive (dead) lymphocytes appeared dark and non-refractiles with eosin dye.
Single step guanidine thiocyanate-chloroform method[23] was used to extract HCV RNA from 50 μL of plasma. RNA extracted was reverse-transcribed using random primers. Nested PCR (primers see Table 1) was used to amplify the HCV NS3 region that spanned a reported cytotoxic T cell epitope (-KLVALGINAV-)[24], which is HLA-A2-restricted. The first round PCR was run for 35 cycles with denaturing at 94 °C for 1 min, annealing at 53 °C for 1 min, and elongating at 72 °C for 1 min. The second round of PCR was run for 35 cycles with denaturing at 94 °C for 1 min, annealing at 60 °C for 1 min, and elongating at 72 °C for 1 min.
| Primer sequences | Strand | Nucleotide positionin HCV genome | |
| First round primers (5’-3’) | CCCCATCAC(A/G)TACTC(C/T)ACCTA | + | 4 197 |
| ACA(C/T)GT(A/G)TT(G/A)CAGTC(T/G)ATCAC | _ | 4 681 | |
| Second round primers (5’-3’) | CGAGGATCCGTCCT(T/G)GACCAAGC(A/G)GAGAC | + | 4 315 |
| GCAACTGCAGCT(G/A)G(T/A)(C/T)GG(G/T)ATGAC(A/G)GACAC | _ | 4 597 |
PCR products were subcloned into M13mp19 phage. For each blood sample, 5 clones were selected and amplified. The single strand DNA produced by the M13mp19 phage was purified by QIAprep Spin 13 kit (Qiagen, Valencia, CA) and sequenced using sequence version 2.0 sequencing kit (USB, Cleveland, OH).
DNA sequences were translated and aligned. Consensus sequence was produced for every 5 clones of each blood sample. Cytotoxic T cell epitopes for each consensus sequence were predicted based on the HLA type of the patients and MHC molecule binding motifs[25].
Patient C was (A11, 30; B13, -; Bw4, -). Patient Z was [A2, 11; B60 (40), 70; Bw6, -]. Patient W was [A2, 11; B40, 55 (22); Bw6, -].
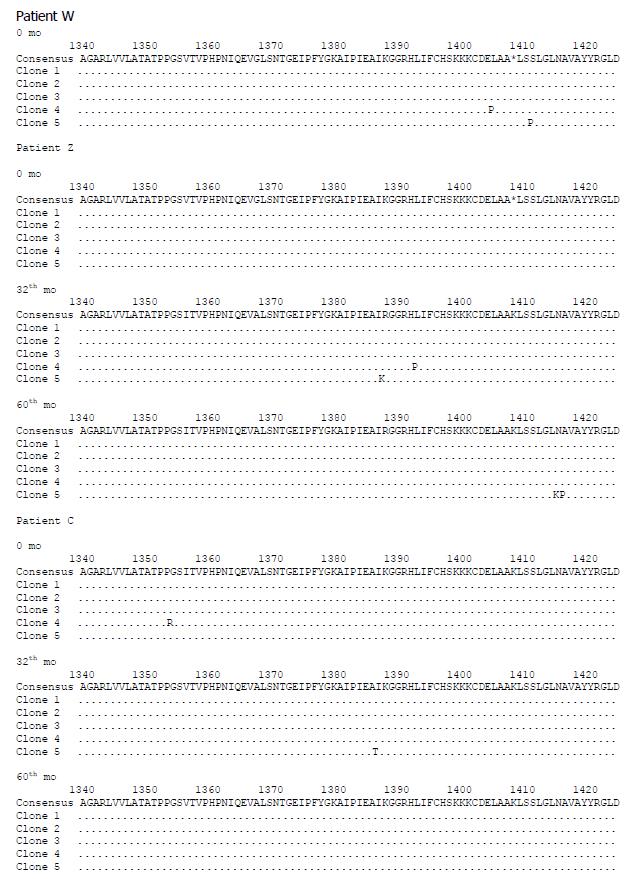
Five clones of NS3 sequences were ascertained for each blood sample. Since all the blood samples of patients C and Z were positive for HCV RNA, 15 sequences were obtained from each one of them. Due to the negative result of HCV RNA in the later 2 blood samples in patient W, only 5 cDNA sequences were obtained. The GenBank accession numbers for all the sequences are in Table 2. The translated amino acid sequences are aligned in Figure 1.
| Time point measured | Patient W | Patient C | Patient Z |
| 0 mo | AF051270 | AF051261 | AF051270 |
| AF051270 | AF051261 | AF051270 | |
| AF051271 | AF051261 | AF051270 | |
| AF051272 | AF051260 | AF051270 | |
| AF051273 | AF051259 | AF051270 | |
| 32th mo | NA | AF051254 | AF051265 |
| AF051255 | AF051266 | ||
| AF051256 | AF051267 | ||
| AF051257 | AF051268 | ||
| AF051258 | AF051269 | ||
| 60th mo | NA | AF051253 | AF051262 |
| AF051253 | AF051262 | ||
| AF051253 | AF051263 | ||
| AF051253 | AF051263 | ||
| AF051253 | AF051264 |
Our consensus sequences showed (K/*)LSSLGLNAV (*: stop codon) on the site of the reported HLA-A2-restricted cytotoxic T cell epitope[24]. In patient C, who was not HLA-A2-restricted, all the 15 sequences were KLSSLGLNAV. In patient W, who was HLA-A2-restricted, all the 5 sequences showed a stop codon at the beginning of this peptide (four sequences showed *LSSLGLNAV and one sequence showed *LSPLGLNAV). In patient Z, who was also HLA-A2-restricted, all the sequences from 0-mo showed the stop codon at the beginning of the epitope (*LSSLGLNAV), nine sequences from blood samples at mo 32 and 60 showed KLSSLGLNAV, one sequence from blood sample at mo 32 showed KLSSLGLKPV.
Using MHC binding motifs to predict cytotoxic T cell epitopes, we found that most sites which showed changes of consensus sequences between successive blood samples were on the predicted cytotoxic T cell epitopes (Table 3).
| Patient | HLA sutype | MHC binding peptide motif[38,39] | Genome position | Predicted epitope | Time point measured |
| C | A11 | X[MLIVSATGNCDF]XXXXXX[KRHY] | 1349 | ATPPGSITVPH* | 0 mo |
| ATPPGSVTVPH* | 32th, 60th mo | ||||
| 1378 | KAIPIEAIR | 0 mo | |||
| KAIPIEAIK | 32th, 60th mo | ||||
| Z | A11 | X[MLIVSATGNCDF]XXXXXX[KRHY] | 1381 | PIEAIKGGR | 0 mo |
| PIEAIRGGR | 32th, 60th mo | ||||
| 1347 | ATATPPGSV | 0 mo | |||
| ATATPPGSI | 32th, 60th mo | ||||
| A 2 | X[LMIVAT]XXXXXX[LVIAMT] | 1348 | TATPPGSVT | 0 mo | |
| TATPPGSIT | 32th, 60th mo | ||||
| 1349 | ATPPGSVTV | 0 mo | |||
| ATPPGSITV | 32th, 60th mo |
Due to errors of the RNA-dependent RNA polymerase, RNA genomes had a relatively high mutation rate[25,26]. RNA viruses evolve as complex distributions of mutants termed viral quasispecies. These coexisting mutant genomes always have a consensus or master sequence. Despite the potentially high mutation rate and variability of RNA viruses, changes in the consensus sequence of a viral population would occur only if some selection mechanism acted on the population and caused a shift in the population equilibrium[27]. Immune response of the host can influence the distribution between different viral variants and will consequently cause a change in the consensus sequence. A cellular immune-driven selection pressure has been demonstrated by the existence of HCV escape mutants in relation to cytotoxic T cell epitopes[28]. In the HCV-infected human, the NS3 protein seems to be fairly immunogenic. T cell activation in response to NS3 has been detected in a number of studies of patients with acute or chronic HCV infection[24,29]. It was proposed that a strong in vitro T cell reaction to NS3 correlated with clearance of acute HCV infection whereas a less vigorous, or absent, NS3-specific T cell reactivity was observed in those who progressed to chronicity[30]. Thus, in this study, we chose a segment of HCV NS3 region as our focus on sequence evolution.
T lymphocytes recognize their antigens in context of MHC-encoded molecules, a phenomenon called MHC restriction. Our sequence segment encompassed a cytotoxic T cell epitope, which was restricted by HLA-A2 and reported by Rehermann et al[24]. In patients with HLA-A2 allele, their viral consensus sequences showed stop codons at the initial part of this epitope. On the contrary, in patients without HLA-A2 allele, their viral consensus sequences did not show the stop codon. Normally, stop codons are generated by random non-sense mutations in RNA virus and they are expected to occur randomly throughout the entire coding region. Viruses with stop codon in the open reading frame have been found to be defective viruses which usually make a small fraction of the RNA virus quasispecies[31,32]. Here, stop codons were unusually concentrated at the beginning of the reported epitope, in the sequences of patients with HLA-A2 allele, suggesting that they are specifically selected by some pressure, probably by cytotoxic T cells. We would suppose that HCV specific and HLA-A2-restricted cytotoxic T cells, which recognize and kill the infected hepatocytes to prevent replication and proliferation of the viruses, were generated in patients W and Z. Under this immune pressure, viral quasispecies in these two patients would have shifted toward a new equilibrium to avoid the immune attack. In patients W and Z, the defective viruses, which did not express the reported cytotoxic T cell epitope, dominated the viral quasispecies at month 0. This may reflect the strong immune pressure at that time. Thirty-two months later, in patient W, the viruses were cleared and the patient was recovered. In patient Z, the viruses were not cleared at month 32 or 60, suggesting that the viral quasispecies escaped from the immune pressure and survived.
Cytotoxic T cells could recognize peptides loaded on the MHC class I molecules[33]. The solution of the crystal structure of MHC class I molecules could reveal peptide-binding groove made up by α1 and α2 domains of heavy chains[34,35]. Naturally occurring processed peptides have been isolated from purified MHC class I molecules. Analyzing their sequences revealed the presence of simple amino acid sequence motifs that were specific to particular allelic forms of class I molecules[36]. Based on the sequence motifs, we found that most sites, with changes of the consensus sequences, were on the putative cytotoxic T cell epitopes in the corresponding patients, implying the possible underlying immune impetus for sequence evolution.
In summary, by molecular sequencing, the quasispecies nature and sequence evolution of HCV NS3 region can be revealed. By HLA typing and epitope prediction, the non-sense mutation and changes of consensus sequences might be the result of immune pressure. This study has paved the way for further cytotoxicity assay[37] to confirm the possible immune target sites of HCV.
Edited by Chen WW and Wang XL Proofread by Xu FM
| 1. | National Institutes of Health Consensus Development Conference Panel statement: management of hepatitis C. Hepatology. 1997;26:2S-10S. [PubMed] |
| 2. | Maier I, Wu GY. Hepatitis C and HIV co-infection: a review. World J Gastroenterol. 2002;8:577-579. [PubMed] |
| 3. | Meier V, Mihm S, Braun Wietzke P, Ramadori G. HCV-RNA positivity in peripheral blood mononuclear cells of patients with chronic HCV infection: does it really mean viral replication. World J Gastroenterol. 2001;7:228-234. [PubMed] |
| 4. | Chen MY, Huang ZQ, Chen LZ, Gao YB, Peng RY, Wang DW. Detection of hepatitis C virus NS5 protein and genome in Chinese carcinoma of the extrahepatic bile duct and its significance. World J Gastroenterol. 2000;6:800-804. [PubMed] |
| 5. | He QQ, Cheng RX, Sun Y, Feng DY, Chen ZC, Zheng H. Hepatocyte transformation and tumor development induced by hepatitis C virus NS3 c-terminal deleted protein. World J Gastroenterol. 2003;9:474-478. [PubMed] |
| 6. | Li K, Wang L, Cheng J, Lu YY, Zhang LX, Mu JS, Hong Y, Liu Y, Duan HJ, Wang G. Interaction between hepatitis C virus core protein and translin protein--a possible molecular mechanism for hepatocellular carcinoma and lymphoma caused by hepatitis C virus. World J Gastroenterol. 2003;9:300-303. [PubMed] |
| 7. | Worman HJ, Lin F. Molecular biology of liver disorders: the hepatitis C virus and molecular targets for drug development. World J Gastroenterol. 2000;6:465-469. [PubMed] |
| 8. | Nelson DR, Marousis CG, Davis GL, Rice CM, Wong J, Houghton M, Lau JY. The role of hepatitis C virus-specific cytotoxic T lymphocytes in chronic hepatitis C. J Immunol. 1997;158:1473-1481. [PubMed] |
| 9. | Assy N, Minuk G. A comparison between previous and present histologic assessments of chronic hepatitis C viral infections in humans. World J Gastroenterol. 1999;5:107-110. [PubMed] |
| 10. | Caselmann WH, Serwe M, Lehmann T, Ludwig J, Sproat BS, Engels JW. Design, delivery and efficacy testing of therapeutic nucleic acidsused to inhibit hepatitis C virus gene expression in vitro and in vivo. World J Gastroenterol. 2000;6:626-629. [PubMed] |
| 11. | Chen LK, Hwang SJ, Tsai ST, Luo JC, Lee SD, Chang FY. Glucose intolerance in Chinese patients with chronic hepatitis C. World J Gastroenterol. 2003;9:505-508. [PubMed] |
| 12. | Fan XG, Tang FQ, Ou ZM, Zhang JX, Liu GC, Hu GL. Lymphoproliferative response to hepatitis C virus (HCV) anti-gens in patients with chronic HCV infection. Shijie Huaren Xiaohua Zazhi. 1999;7:1038-1040. |
| 13. | Song ZQ, Hao F, Zhang J, Gu CH. Detection of antibodies against hypervariable region 1 in sera from patients with hepatitis C. Shijie Huaren Xiaohua Zazhi. 1999;7:666-668. |
| 14. | Wu HB, Li ZW, Li Y. Clinical significance of detection of posi-tive and negative strands of HCV RNA in peripheral blood mono-nuclear cells. Shijie Huaren Xiaohua Zazhi. 1999;7:220-221. |
| 15. | Zhou YX, Feng ZH, Jia ZS, Lian JQ, Li JG, Li WB. A study of gene immunization with recombinant expression plasmid of hepatitis C virus core antigen. Shijie Huaren Xiaohua Zazhi. 1998;6:966-968. |
| 16. | Major ME, Feinstone SM. The molecular virology of hepatitis C. Hepatology. 1997;25:1527-1538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 212] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 17. | Chen S, Wang YM. Genetic evolution of structural region of hepatitis C virus in primary infection. World J Gastroenterol. 2002;8:686-693. [PubMed] |
| 18. | Flichman D, Kott V, Sookoian S, Campos R. Acute hepatitis C in a chronically HIV-infected patient: evolution of different viral genomic regions. World J Gastroenterol. 2003;9:1496-1500. [PubMed] |
| 19. | Chen YD, Liu MY, Yu WL, Li JQ, Dai Q, Zhou ZQ, Tisminetzky SG. Mix-infections with different genotypes of HCV and with HCV plus other hepatitis viruses in patients with hepatitis C in China. World J Gastroenterol. 2003;9:984-992. [PubMed] |
| 20. | Weiner AJ, Geysen HM, Christopherson C, Hall JE, Mason TJ, Saracco G, Bonino F, Crawford K, Marion CD, Crawford KA. Evidence for immune selection of hepatitis C virus (HCV) putative envelope glycoprotein variants: potential role in chronic HCV infections. Proc Natl Acad Sci USA. 1992;89:3468-3472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 499] [Cited by in RCA: 482] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 21. | Rehermann B, Chang KM, McHutchison JG, Kokka R, Houghton M, Chisari FV. Quantitative analysis of the peripheral blood cytotoxic T lymphocyte response in patients with chronic hepatitis C virus infection. J Clin Invest. 1996;98:1432-1440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 229] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 22. | Li CP, Wang KX, Wang J, Pan BR. mIL-2R, T cell subsets & amp; hepatitis C. World J Gastroenterol. 2002;8:298-300. [PubMed] |
| 23. | Chomczynski P, Sacchi N. Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Anal Biochem. 1987;162:156-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40518] [Cited by in RCA: 39087] [Article Influence: 1028.6] [Reference Citation Analysis (0)] |
| 24. | Rehermann B, Chang KM, McHutchinson J, Kokka R, Houghton M, Rice CM, Chisari FV. Differential cytotoxic T-lymphocyte responsiveness to the hepatitis B and C viruses in chronically infected patients. J Virol. 1996;70:7092-7102. [PubMed] |
| 25. | Guo H, Wang W, Wang T. An application of T cell epitope pre-diction computer program in the study of HCV adaptive immune responses. Disi Junyi Daxue Xuebao. 1999;20:845-848. |
| 26. | Huang F, Zhao GZ, Li Y. HCV genotypes in hepatitis C patients and their clinical significances. World J Gastroenterol. 1999;5:547-549. [PubMed] |
| 27. | Elena SF, Miralles R, Cuevas JM, Turner PE, Moya A. The two faces of mutation: extinction and adaptation in RNA viruses. IUBMB Life. 2000;49:5-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 28. | Wodarz D. Hepatitis C virus dynamics and pathology: the role of CTL and antibody responses. J Gen Virol. 2003;84:1743-1750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 62] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 29. | Encke J, zu Putlitz J, Geissler M, Wands JR. Genetic immunization generates cellular and humoral immune responses against the nonstructural proteins of the hepatitis C virus in a murine model. J Immunol. 1998;161:4917-4923. [PubMed] |
| 30. | Wertheimer AM, Miner C, Lewinsohn DM, Sasaki AW, Kaufman E, Rosen HR. Novel CD4+ and CD8+ T-cell determinants within the NS3 protein in subjects with spontaneously resolved HCV infection. Hepatology. 2003;37:577-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 96] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 31. | Martell M, Esteban JI, Quer J, Genescà J, Weiner A, Esteban R, Guardia J, Gómez J. Hepatitis C virus (HCV) circulates as a population of different but closely related genomes: quasispecies nature of HCV genome distribution. J Virol. 1992;66:3225-3229. [PubMed] |
| 32. | Higashi Y, Kakumu S, Yoshioka K, Wakita T, Mizokami M, Ohba K, Ito Y, Ishikawa T, Takayanagi M, Nagai Y. Dynamics of genome change in the E2/NS1 region of hepatitis C virus in vivo. Virology. 1993;197:659-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 87] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 33. | Androlewicz MJ. Peptide generation in the major histocompatibility complex class I antigen processing and presentation pathway. Curr Opin Hematol. 2001;8:12-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 34. | Khan AR, Baker BM, Ghosh P, Biddison WE, Wiley DC. The structure and stability of an HLA-A*0201/octameric tax peptide complex with an empty conserved peptide-N-terminal binding site. J Immunol. 2000;164:6398-6405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 142] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 35. | Sliz P, Michielin O, Cerottini JC, Luescher I, Romero P, Karplus M, Wiley DC. Crystal structures of two closely related but antigenically distinct HLA-A2/melanocyte-melanoma tumor-antigen peptide complexes. J Immunol. 2001;167:3276-3284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 74] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 36. | Davenport MP, Smith KJ, Barouch D, Reid SW, Bodnar WM, Willis AC, Hunt DF, Hill AV. HLA class I binding motifs derived from random peptide libraries differ at the COOH terminus from those of eluted peptides. J Exp Med. 1997;185:367-371. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 37. | Zhou HC, Xu DZ, Wang XP, Zhang JX, Huang Y, Yan YP, Zhu Y, Jin BQ. Identification of the epitopes on HCV core protein recognized by HLA-A2 restricted cytotoxic T lymphocytes. World J Gastroenterol. 2001;7:583-586. [PubMed] |
| 38. | Reche PA, Glutting JP, Reinherz EL. Prediction of MHC class I binding peptides using profile motifs. Hum Immunol. 2002;63:701-709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 249] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 39. | Rammensee H, Bachmann J, Emmerich NP, Bachor OA, Stevanović S. SYFPEITHI: database for MHC ligands and peptide motifs. Immunogenetics. 1999;50:213-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1764] [Cited by in RCA: 1776] [Article Influence: 68.3] [Reference Citation Analysis (0)] |
| 40. | Guo HC, Jardetzky TS, Garrett TP, Lane WS, Strominger JL, Wiley DC. Different length peptides bind to HLA-Aw68 similarly at their ends but bulge out in the middle. Nature. 1992;360:364-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 294] [Cited by in RCA: 315] [Article Influence: 9.5] [Reference Citation Analysis (0)] |