Published online Mar 1, 2004. doi: 10.3748/wjg.v10.i5.765
Revised: December 9, 2003
Accepted: December 16, 2003
Published online: March 1, 2004
A 74-year-old man was admitted to the hospital because of chemotherapy for relapsed non-Hodgkin’s lymphoma (NHL). The patient became febrile and experienced diarrhea after chemotherapy. Although ceftazidime and amikacin sulfate were administered as empiric therapy, diarrhea was continued. After several days, stool cytotoxin assay for clostridium difficile (C. difficile) was positive and he was diagnosed as having antibiotics-associated colitis (AAC). Although antibiotics were discontinued and both oral vancomycin and metronidazole were administrated, disease was not improved. To rule out the presence of an additional cause of diarrhea, colon fiberoscopic examination was performed. It revealed multiple deep ulcerative lesions at right side colon, surface erosive and minute erosive lesions in all continuous colon. Pseudomembranes were not seen. These findings are compatible with AAC without pseudomembranes. There are no reports that the rifampin is effective on refractory AAC. However, we administered oral rifampin for the current patient. The reasons are 1) conventional antibiotics were not effective, 2) rifampin has excellent in vitro activity against C. difficile, and 3) the efficacy of rifampin on relapsing colitis due to C. difficile is established. After administration of rifampin, fever alleviated and diarrhea was improved. Because AAC may result in significant mortality, patients with refractory or fulminant AAC should be treated with oral rifampin from outset.
- Citation: Nomura K, Matsumoto Y, Yoshida N, Taji S, Wakabayashi N, Mitsufuji S, Horiike S, Morita M, Okanoue T, Taniwaki M. Successful treatment with rifampin for fulminant antibiotics-associated colitis in a patient with non-Hodgkin’s lymphoma. World J Gastroenterol 2004; 10(5): 765-766
- URL: https://www.wjgnet.com/1007-9327/full/v10/i5/765.htm
- DOI: https://dx.doi.org/10.3748/wjg.v10.i5.765
Antibiotics-associated colitis (AAC) due to clostridium difficile (C. difficile) is a nosocomial infection that may result in significant morbidity and mortality. AAC is capable of causing toxigeneic colitis in susceptible patients such as those receiving chemotherapy. Approximately, 50% cases having endoscopic evidence of pseudomembranous colitis revealed exudative and puntate raised plaques with slip areas. The remainder had milder degrees of colitis without pseudomembranes[1,2]. The clinical features of AAC without pseudomembranes are thought to be similar to those seen with pseudomembranes colitis, but of less severity[3,4]. Patients with mild colitis are improved only by discontinuation of antibiotics. However, most patients are now treated with vancomycin (VCM) or metronidazole capable of eradicating C. difficile infection because of high mortality from AAC. The typical response to VCM therapy is improvement in diarrhea within a few days.
The recommendation is not established for patients with fulminant AAC. Colectomy may be life-saving in patients with severe AAC who fail to respond to antibiotic therapy. However, the surgical mortality is approximately 50%[5].
We described a refractory patient having AAC without pseudomembranes. This patient was refractory to metronidazole and VCM. We administered oral rifampin for the current patient and he gained improvement. This is the first report that rifampin is effective for refractory or fulminant AAC.
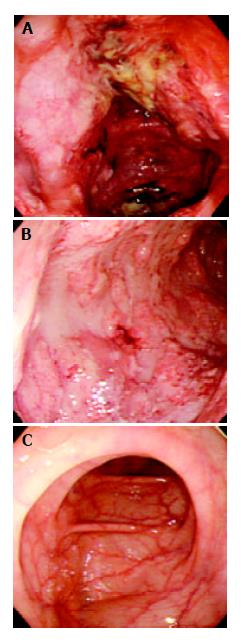
A 74-year-old man was admitted to our hospital in May 2002 because of chemotherapy for relapsed non-Hodgkin’s lymphoma. He presented a huge mass of NHL at lumber. He was treated with 3 courses of VeMP combination chemotherapy[6]. After the first VeMP chemotherapy, he complained of diarrhea. Fosfomycin calcium (FOM) was administered and diarrhea was stopped. There was no side effect during the second course of VeMP chemotherapy. During the third chemotherapy, he became febrile without diarrhea, we administered ceftazidime (CAZ) and amikacin sulfate (AMK) as empiric therapy. Fever alleviated immediately. Considering the high frequencies of relapse in patients treated with VeMP, we stopped VeMP therapy and started CHOP therapy (cyclophosphamide, adriamycin, vincristine, and predonisolone) on 6 August. Because the patient became febrile and experienced diarrhea from d 4, we administrated lactomin. On d 8, the patient developed massive watery diarrhea (over 1500 mL/d) with exacerbation of fever, respiratory distress and marked hypovolemia. Ultrasound examination revealed massive ascites and pleural effusion. Although bolus methylprednisolone was administered promptly and CAZ and AMK as empiric therapy, the patient remained febrile and watery green diarrhea was not controlled. Salmonella, Shigella, campylobacter, cryptosporidium, fecal viruses and parasites were negative in repeated stool cultures. Because C. difficile toxin was detected using an enzyme immunoassay (Meridian Diagnostics, Inc., Cincinnati, OH, USA) in stools on day 13, the patient was diagnosed as having AAC. Although CAZ and AMK were stopped and oral VCM and metronidazole 250 mg daily were started concomitantly, symptom did not improve. Colonoscopic examination revealed multiple deep ulcerative lesions at right side colon, surface erosive and minute erosive lesions in all continuous colon. Pseudomembranes were not seen. Biopsy reveals an outpouring of fibrin, mucus, and inflammatory cells from a microulceration of the surface epithelium. These findings are compatible with AAC without pseudomembranes. Because VCM and metronidazole were not effective, the enteral use of rifampin 600 mg twice daily was started on d 23. In the following several days, fever alleviated and diarrhea was improved (Figure 1).
We described a patient having refractory AAC without pseudomembranes. The current patient presented severe watery diarrhea, malaise, fever, leukocytosis and dehydration. Administration of VCM and metronidazole was not effective. Some treatment regimens as the second therapy for refractory AAC have been tried, but none has been completely effective in randomized clinical trials. Although there have been some reports of the efficacy of oral teicoplanin for the treatment of antibiotics-associated colitis[7,8], oral teicoplanin is not available in Japan. Colectomy was not required, because the current patient had a substantial comorbid disease and was extremely ill.
Rifampin had excellent in vitro activity against C.difficile with minimum inhibitory concentrations averaging < 0.2 μg/mL[9,10] and the efficacy of rifampin on relapsing colitis due to C. difficile was established[11]. Thus, we administered rifampin 600 mg twice daily. Diarrhea and abdominal pain resolved promptly. Although there are no reports that rifampin is a useful agent for refractory and severe AAC, patients should be treated with oral rifampin from the outset.
Edited by Wang XL Proofread by Zhu LH
| 1. | Lishman AH, Al-Jumaili IJ, Record CO. Spectrum of antibiotic-associated diarrhoea. Gut. 1981;22:34-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 29] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Bergstein JM, Kramer A, Wittman DH, Aprahamian C, Quebbeman EJ. Pseudomembranous colitis: how useful is endoscopy. Surg Endosc. 1990;4:217-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Totten MA, Gregg JA, Fremont-Smith P, Legg M. Clinical and pathological spectrum of antibiotic-associated colitis. Am J Gastroenterol. 1978;69:311-319. [PubMed] |
| 4. | Gerding DN, Olson MM, Peterson LR, Teasley DG, Gebhard RL, Schwartz ML, Lee JT. Clostridium difficile-associated diarrhea and colitis in adults. A prospective case-controlled epidemiologic study. Arch Intern Med. 1986;146:95-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 228] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 5. | Klingler PJ, Metzger PP, Seelig MH, Pettit PD, Knudsen JM, Alvarez SA. Clostridium difficile infection: risk factors, medical and surgical management. Dig Dis. 2000;18:147-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Santini G, Contu A, Porcellini A, Chisesi T, Coser P, Congiu AM, Morandi S, Manna A, Schintu GM, Quaini R. Mitoxantrone alone or in combination chemotherapy (VeMP) as second-line treatment in relapsed or refractory poor-prognosis non-Hodgkin's lymphoma. A report of the Non-Hodgkin's Lymphoma Co-operative Study Group (NHLCSG). Haematologica. 1991;76:485-490. [PubMed] |
| 7. | de Lalla F, Privitera G, Rinaldi E, Ortisi G, Santoro D, Rizzardini G. Treatment of Clostridium difficile-associated disease with teicoplanin. Antimicrob Agents Chemother. 1989;33:1125-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 29] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Wenisch C, Parschalk B, Hasenhündl M, Hirschl AM, Graninger W. Comparison of vancomycin, teicoplanin, metronidazole, and fusidic acid for the treatment of Clostridium difficile-associated diarrhea. Clin Infect Dis. 1996;22:813-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 352] [Cited by in RCA: 322] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 9. | O'Connor RP, Silva J, Fekety R. Rifampicin and antibiotic-associated colitis. Lancet. 1981;1:499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Ripa S, Mignini F, Prenna M, Falcioni E. In vitro antibacterial activity of rifaximin against Clostridium difficile, Campylobacter jejunii and Yersinia spp. Drugs Exp Clin Res. 1987;13:483-488. [PubMed] |
| 11. | Buggy BP, Fekety R, Silva J. Therapy of relapsing Clostridium difficile-associated diarrhea and colitis with the combination of vancomycin and rifampin. J Clin Gastroenterol. 1987;9:155-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 74] [Article Influence: 1.9] [Reference Citation Analysis (0)] |