Copyright
©The Author(s) 2025.
World J Gastroenterol. Feb 21, 2025; 31(7): 100973
Published online Feb 21, 2025. doi: 10.3748/wjg.v31.i7.100973
Published online Feb 21, 2025. doi: 10.3748/wjg.v31.i7.100973
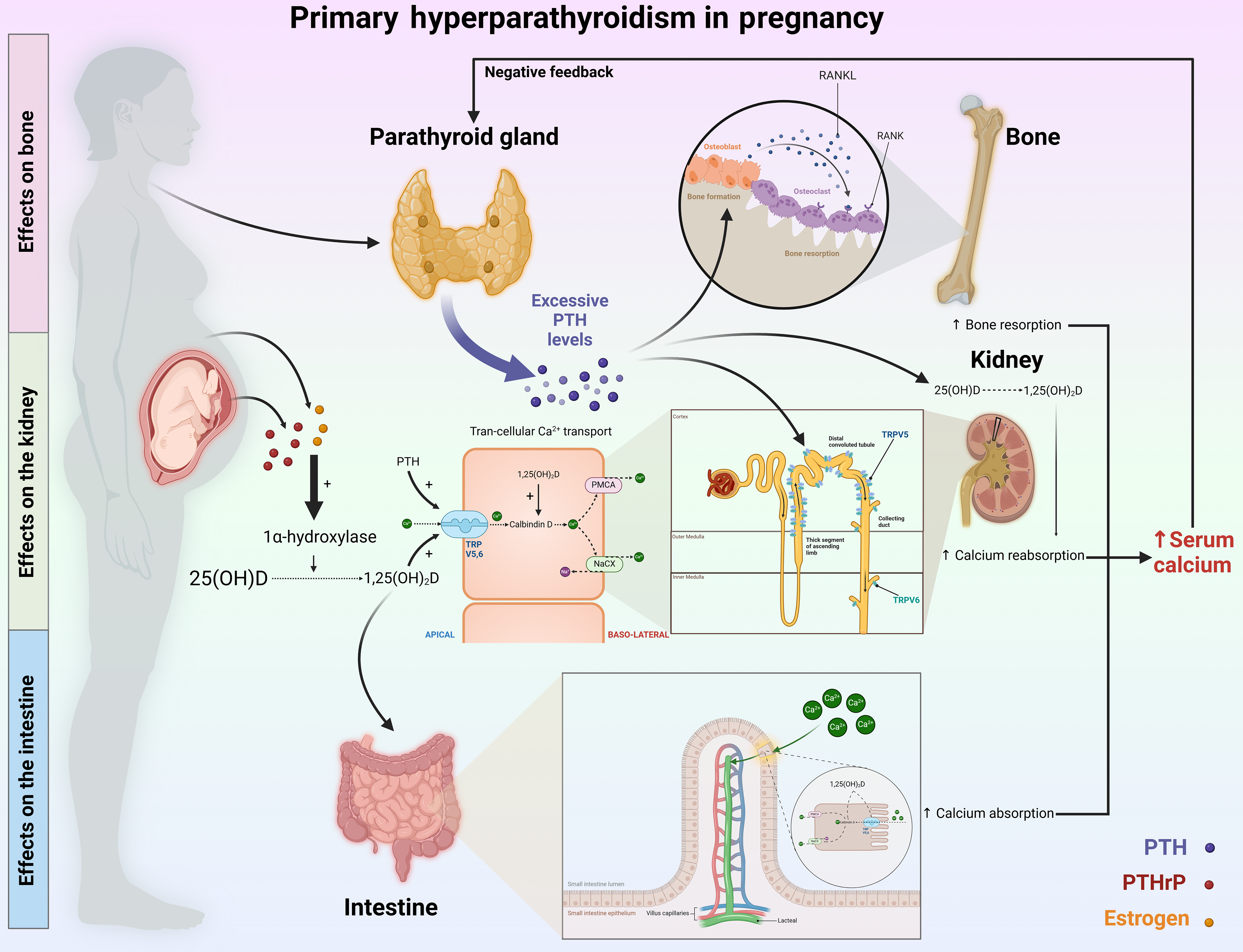
Figure 1 Key mechanisms of calcium regulation in pregnant individuals with primary hyperparathyroidism.
In patients with primary hyperparathyroidism, excessive secretion of parathyroid hormone (PTH) leads to hypercalcemia by impacting bones, kidneys, and intestines. It initiates this process in bones by promoting the secretion of receptor activators of nuclear factor kappa beta ligand, which activates osteoclasts to increase bone resorption, releasing calcium into the bloodstream. Concurrently, in the kidneys, PTH enhances calcium reabsorption by increasing transient receptor potential vanilloid 5 activity and stimulating the enzyme 1α-hydroxylase, which is crucial for converting vitamin D into its active form, 1,25-dihydroxyvitamin D, which is essential for effective calcium metabolism. PTH also indirectly influences intestinal calcium and phosphate absorption by upregulating transport proteins such as transient receptor potential vanilloid 6, calbindin, and adenosine triphosphate-dependent calcium pumps. During pregnancy, the situation is compounded by increased levels of estrogen and PTH-related protein, which activate 1-alpha hydroxylase, facilitating the conversion of 25-hydroxyvitamin D to calcitriol. This increase in calcitriol levels further increases the expression of calcium transport proteins in the intestines, thereby exacerbating hypercalcemia. PTH: Parathyroid hormone; PTHrP: Parathyroid hormone-related protein; 25(OH)D: 25-hydroxyvitamin D; NACX: Sodium-calcium exchanger; PMCA: Plasma membrane calcium adenosine triphosphatase; RANK: Receptor activator of nuclear factor kappa beta; TRPV5: Transient receptor potential vanilloid 5.
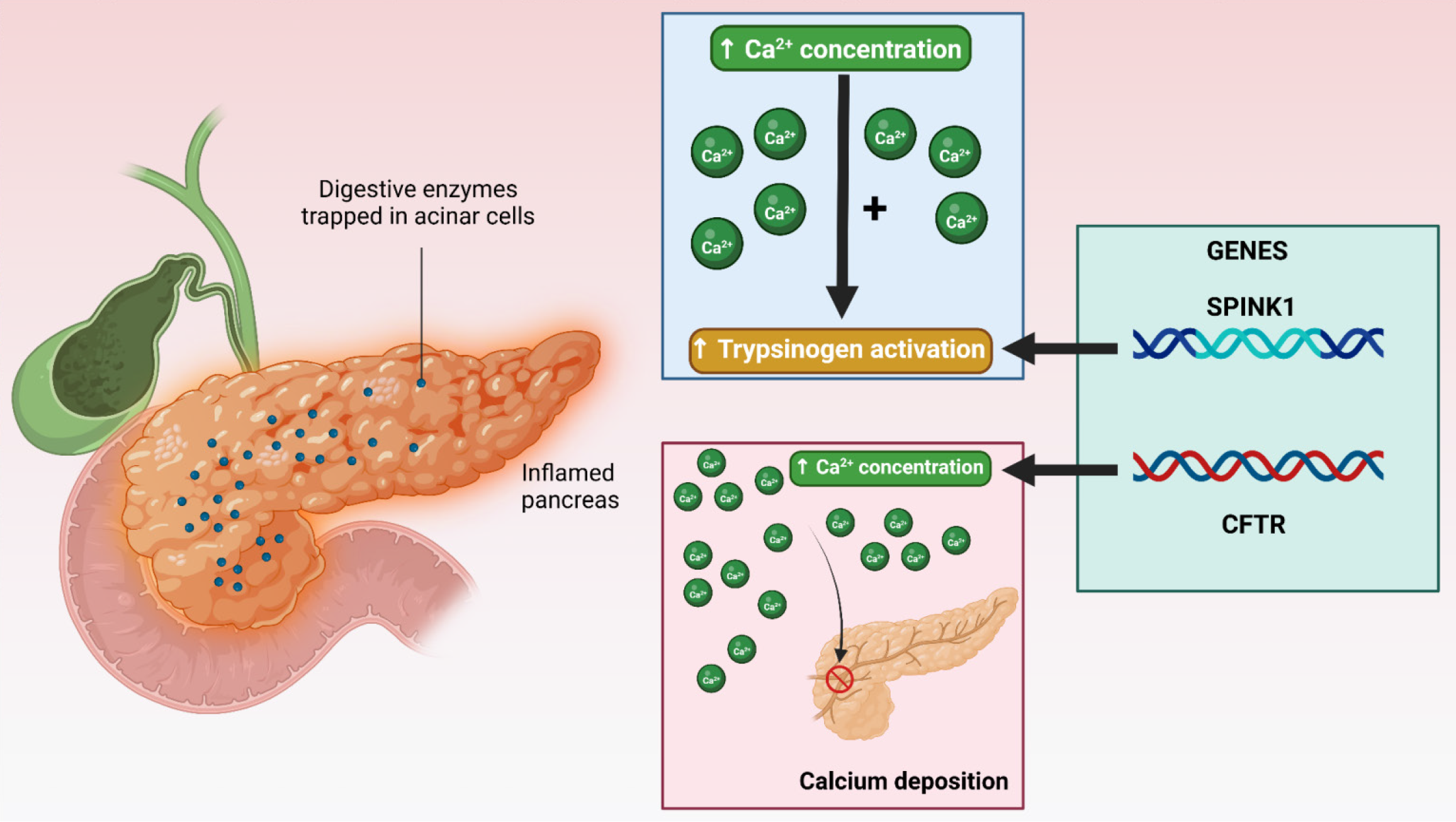
Figure 2 Mechanisms of acute pancreatitis due to hyperparathyroidism during pregnancy.
This figure outlines the two principal mechanisms contributing to acute pancreatitis: Increased trypsinogen activation due to elevated calcium levels and increased calcium deposition. This finding also highlights the exacerbating role of genetic variants, with serine peptidase inhibitor Kazal type 1 mutations intensifying trypsinogen activation and cystic fibrosis transmembrane conductance regulator mutations promoting calcium deposition. SPINK1: Serine peptidase inhibitor Kazal type 1; CFTR: Cystic fibrosis transmembrane conductance regulator.
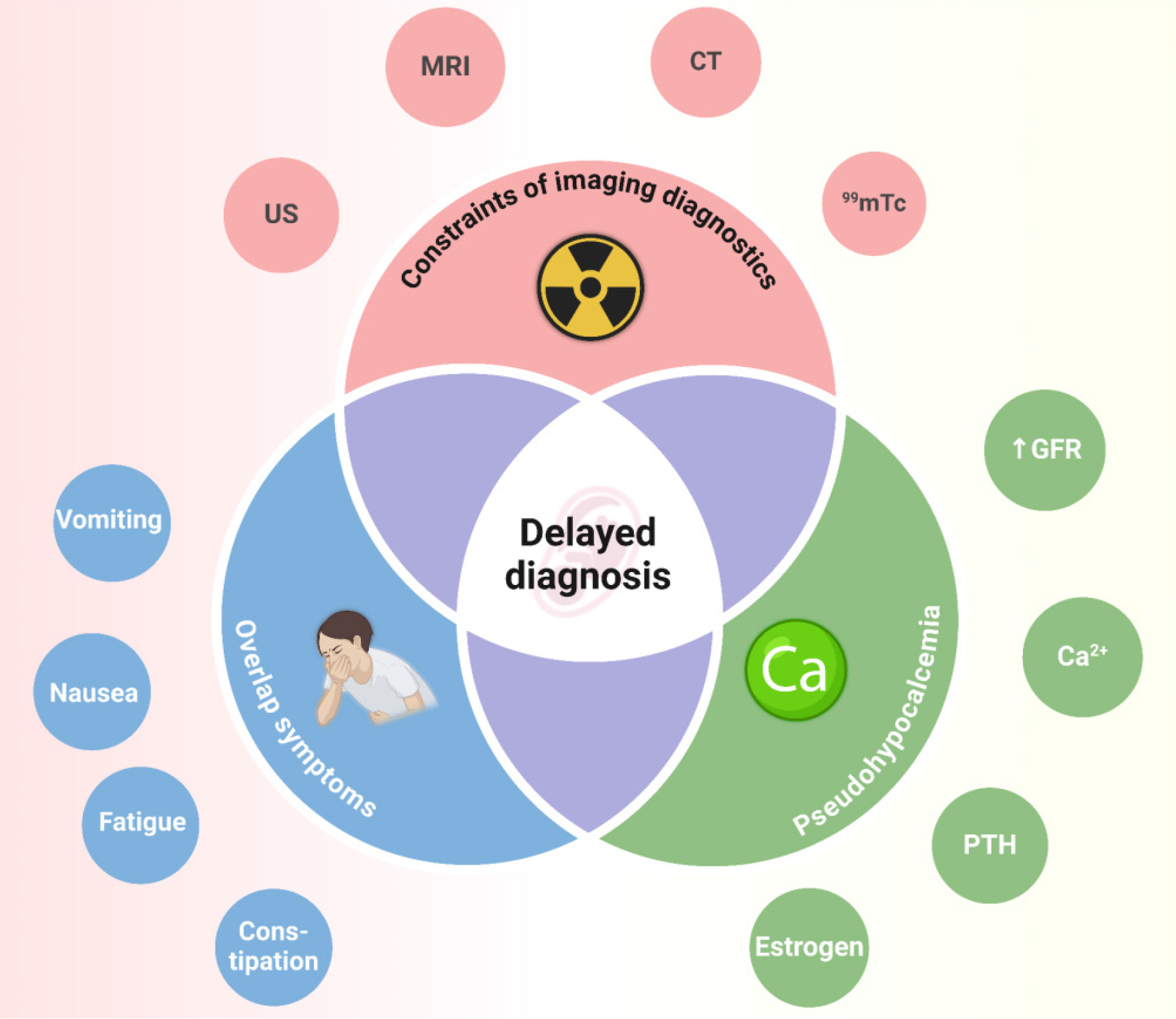
Figure 3 Challenges in the early diagnosis of acute pancreatitis due to primary hyperthyroidism during pregnancy.
The difficulties in diagnosing primary hyperparathyroidism during pregnancy are related primarily to physiological changes, which lead to overlapping clinical symptoms and affect the results of biochemical tests. Additionally, imaging tests are limited in use because of the potential negative impact on the fetus. 99mTc: 99m Technetium; CT: Computed tomography; GFR: Glomerular filtration rate; MRI: Magnetic resonance imaging; PTH: Parathyroid hormone; US: Ultrasound.
Figure 4 Algorithm for primary hyperparathyroidism-induced acute pancreatitis during pregnancy.
Pregnant patients presenting with symptoms such as anorexia, abdominal pain, nausea, vomiting, and constipation from the 20th week of pregnancy should undergo careful clinical evaluation. If acute pancreatitis is suspected, tests including amylase, lipase, and imaging studies should be performed, with abdominal ultrasound being the first-line test because of its low cost and lack of fetal impact. After acute pancreatitis is diagnosed, biochemical and imaging tests should be conducted to confirm the presence of primary hyperparathyroidism. In patients with symptoms of hypercalcemia due to primary hyperparathyroidism, parathyroidectomy should be considered. Additionally, the fetal condition should be assessed. If fetal distress is present, treatment with tocolytic drugs should be initiated, and an emergency cesarean section should be considered if initial medical management is ineffective. 1Consider using a low radiation dose with patient consent when an magnetic resonance imaging cannot be performed; 2When the patient has a family history, it is young and is able to undergo the procedure; 3Perform when MRI cannot be detected/used, with patient consent, and using a low radiation dose. 99mTc: 99m Technetium; CT: Computed tomography; MRI: Magnetic resonance imaging; US: Ultrasound.
- Citation: Luong TV, Le LD, Nguyen NVD, Dang HNN. Persistent challenges in the diagnosis of acute pancreatitis due to primary hyperparathyroidism during pregnancy. World J Gastroenterol 2025; 31(7): 100973
- URL: https://www.wjgnet.com/1007-9327/full/v31/i7/100973.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i7.100973