Copyright
©The Author(s) 2025.
World J Gastroenterol. Apr 14, 2025; 31(14): 103901
Published online Apr 14, 2025. doi: 10.3748/wjg.v31.i14.103901
Published online Apr 14, 2025. doi: 10.3748/wjg.v31.i14.103901
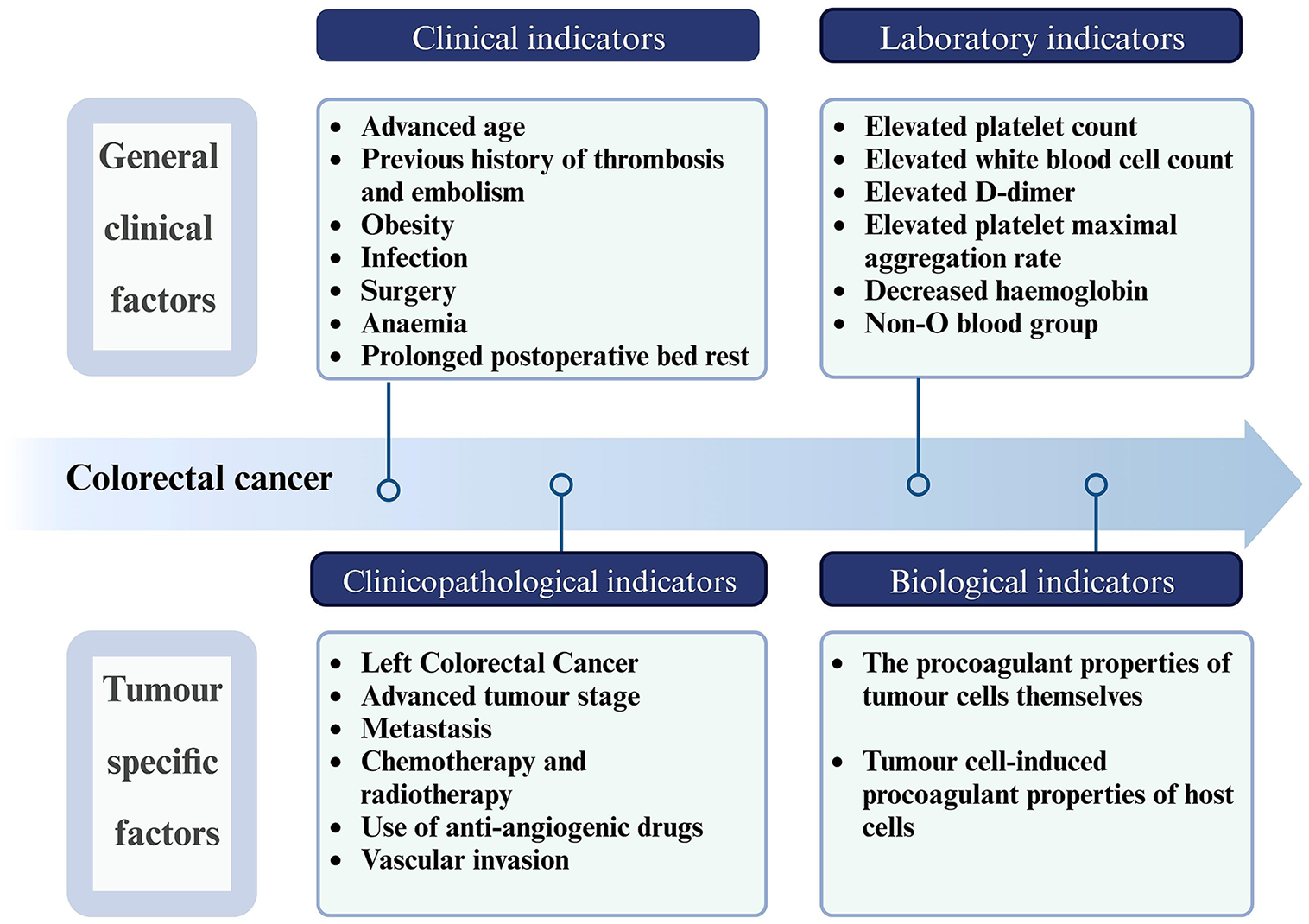
Figure 1 Clinical risk factors influencing thrombosis in colorectal cancer.
This figure delineates two primary categories of clinical risk factors: General clinical factors and tumor-specific factors. General clinical factors, prevalent in both tumor and non-tumor patients, contribute to the overall risk landscape. However, it is the presence of tumor-specific clinical risk indicators and biological markers unique to malignant tumors that particularly delineates the pathogenesis of thrombosis associated with colorectal cancer. Collectively, these factors precipitate a shift in hemostatic equilibrium, favoring a hypercoagulable state. Created in BioRender (Supplementary material).
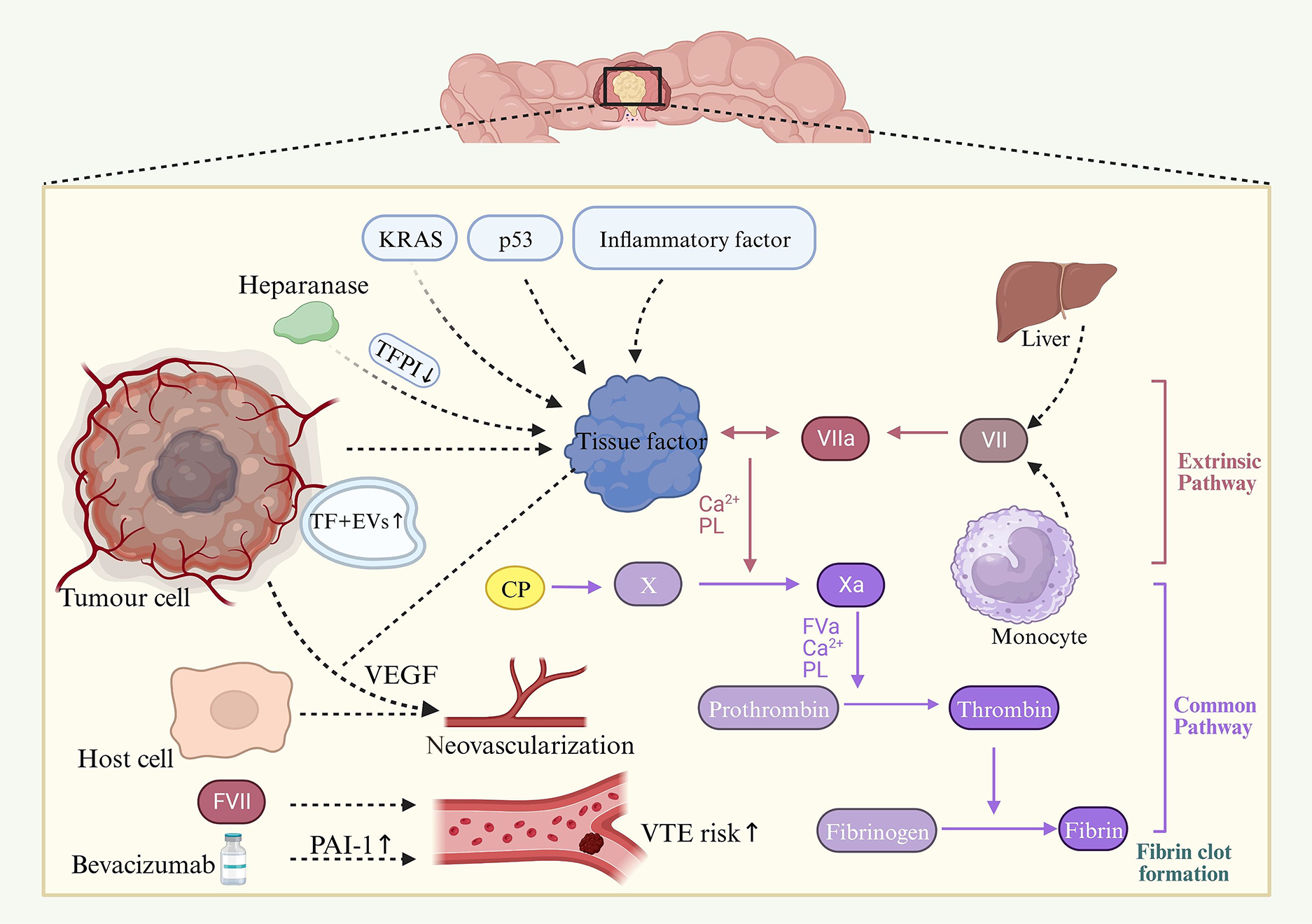
Figure 2 Self-promoting procoagulant properties of tumor cells: An insight into tumor-induced coagulation mechanisms.
This figure illustrates the multifaceted role of colorectal cancer cells in activating the coagulation system. Central to this process is the self-expression of tissue factor (TF), a pivotal protein in cancer-associated thrombosis. The regulation of TF is influenced by key genetic alterations, including activation of the KRAS oncogene and loss of the p53 tumor suppressor, as well as by the tumor’s inflammatory milieu. TF not only initiates coagulation via its complex with activated factor VII, leading to exogenous pathway activation, but also enhances tumor progression by upregulating vascular endothelial growth factor (VEGF) in both malignant and host vascular cells. Concurrently, cancer procoagulant activates factor X, bypassing the need for factor VII. The role of acetylheparinase in increasing TF activity through the dissociation of tissue factor pathway inhibitor is also noted. Moreover, we observe an upsurge in TF-positive extracellular vesicles (TF+ EVs) in colorectal cancer, reinforcing the coagulation cascade. The association of plasma coagulation factors VII (FVII) and VIII (FVIII) with hypercoagulability is highlighted, along with the thrombotic implications of Bevacizumab treatment, a VEGF-targeting drug that elevates plasminogen activator inhibitor-1 levels. PL: Phospholipid; VTE: Venous thromboembolism. Created in BioRender (Supplementary material).
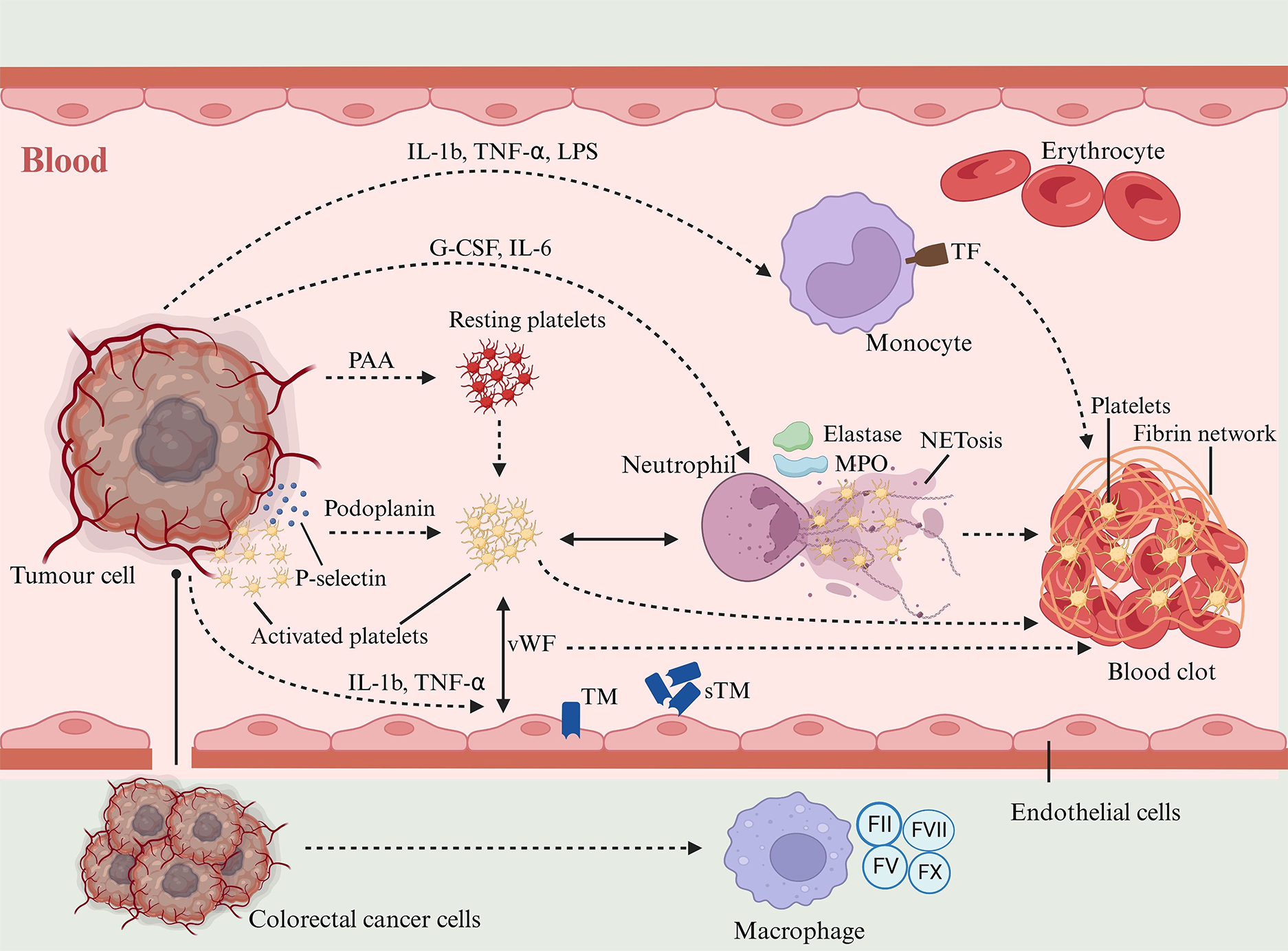
Figure 3 Induction of procoagulant phenotype in host cells by colorectal cancer cells: A cascade of cellular interactions.
This section delineates how colorectal cancer cells orchestrate a procoagulant environment through dynamic interactions with host cells. These interactions occur via direct adhesion or through the release of soluble mediators, leading to the expression of a procoagulant phenotype in host cells. A key mechanism involves the secretion of platelet aggregation agonists by tumor cells, stimulating platelet aggregation. Tumor cells also express Podoplanin, which activates platelets. These activated platelets are pivotal in inducing neutrophil extracellular traps from neutrophils, further promoting thrombus formation by trapping and activating additional platelets. The role of activated platelets extends to enhancing blood hypercoagulability through interactions with endothelium-bound von Willebrand factor. In parallel, cancer cells secrete granulocyte colony-stimulating factor and interleukin-6 (IL-6), which activate neutrophils. The secretion of IL-1β, tumor necrosis factor-alpha, and lipopolysaccharide by tumor cells induces a thrombotic mechanism in monocytes, characterized by increased expression of procoagulant tissue factor. Moreover, tumor-infiltrating macrophages express coagulation factors II, V, VII, and X on their surfaces, contributing further to the procoagulant milieu. Finally, the secretion of inflammatory mediators by tumor cells alters the expression of endothelial cellular products such as thrombomodulin (TM), leading to elevated levels of soluble TM and a concurrent decrease in surface TM expression, thereby diminishing the anticoagulant properties of endothelial cell membranes. MPO: Myeloperoxidase; NETosis: Formation of neutrophil extracellular traps. Created in BioRender (Supplementary material).
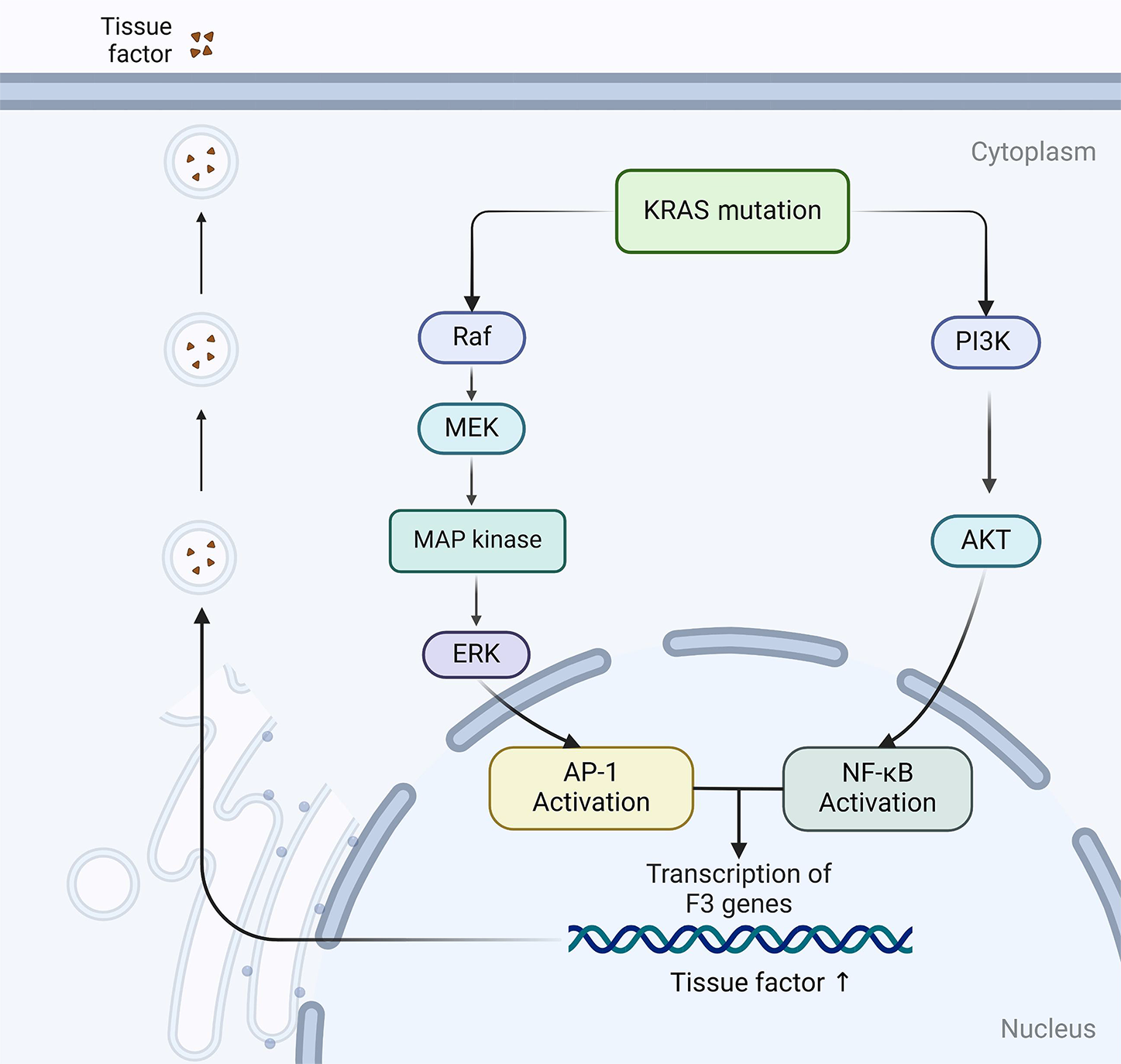
Figure 4 The mechanism diagram illustrates that KRAS gene mutations lead to an increase in tissue factor expression through constitutive activation of the RAS/mitogen-activated protein kinase and phosphatidylinositol 3-kinase/AKT signaling pathways.
Created in BioRender (Supplementary material).
- Citation: Xu DG, Tan J. Interplay of genetic and clinical factors in cancer-associated thrombosis: Deciphering the prothrombotic landscape of colorectal cancer. World J Gastroenterol 2025; 31(14): 103901
- URL: https://www.wjgnet.com/1007-9327/full/v31/i14/103901.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i14.103901