Copyright
©The Author(s) 2025.
World J Gastroenterol. Mar 21, 2025; 31(11): 104377
Published online Mar 21, 2025. doi: 10.3748/wjg.v31.i11.104377
Published online Mar 21, 2025. doi: 10.3748/wjg.v31.i11.104377
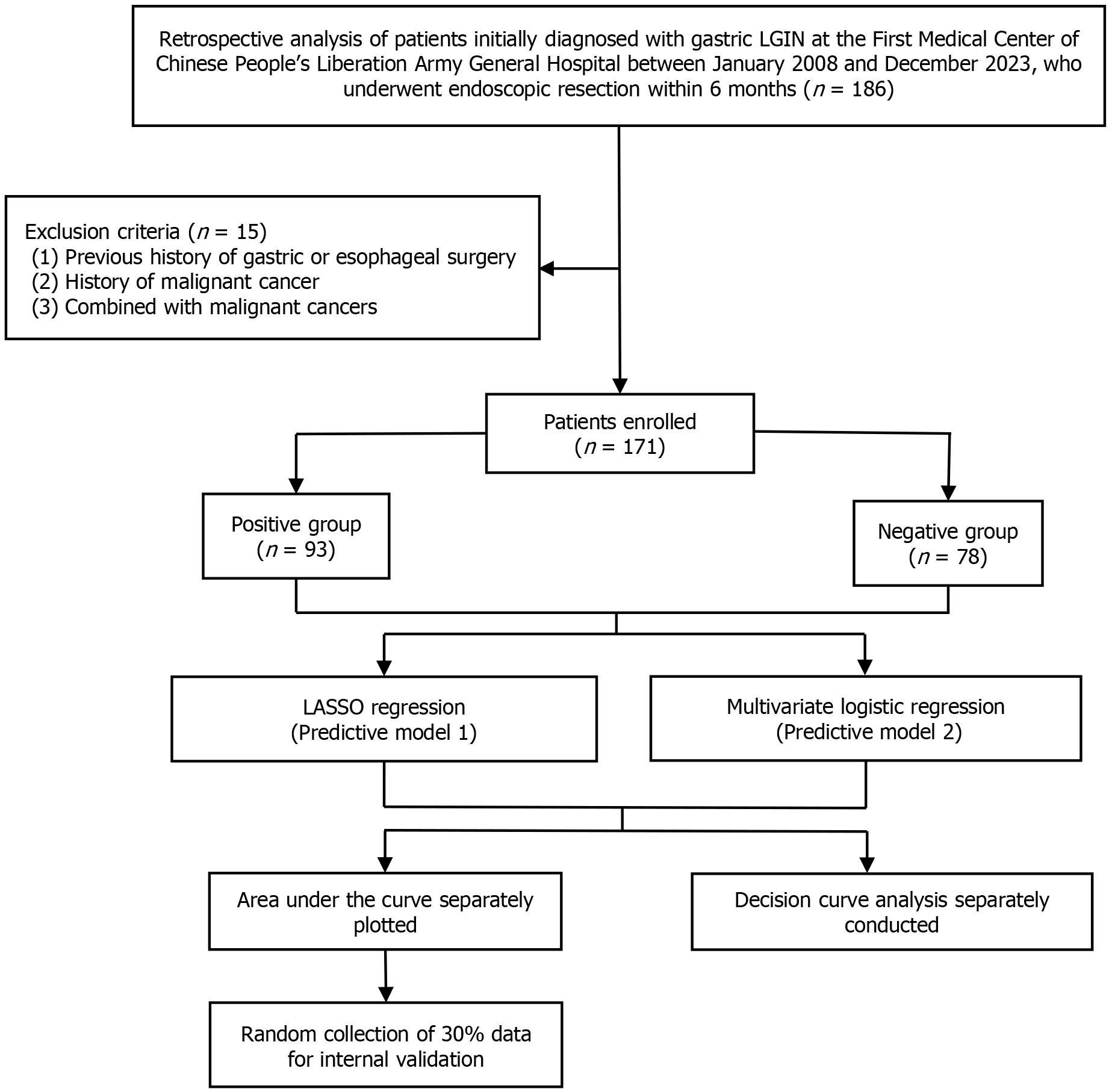
Figure 1 Study flowchart.
LGIN: Low-grade intraepithelial neoplasia.
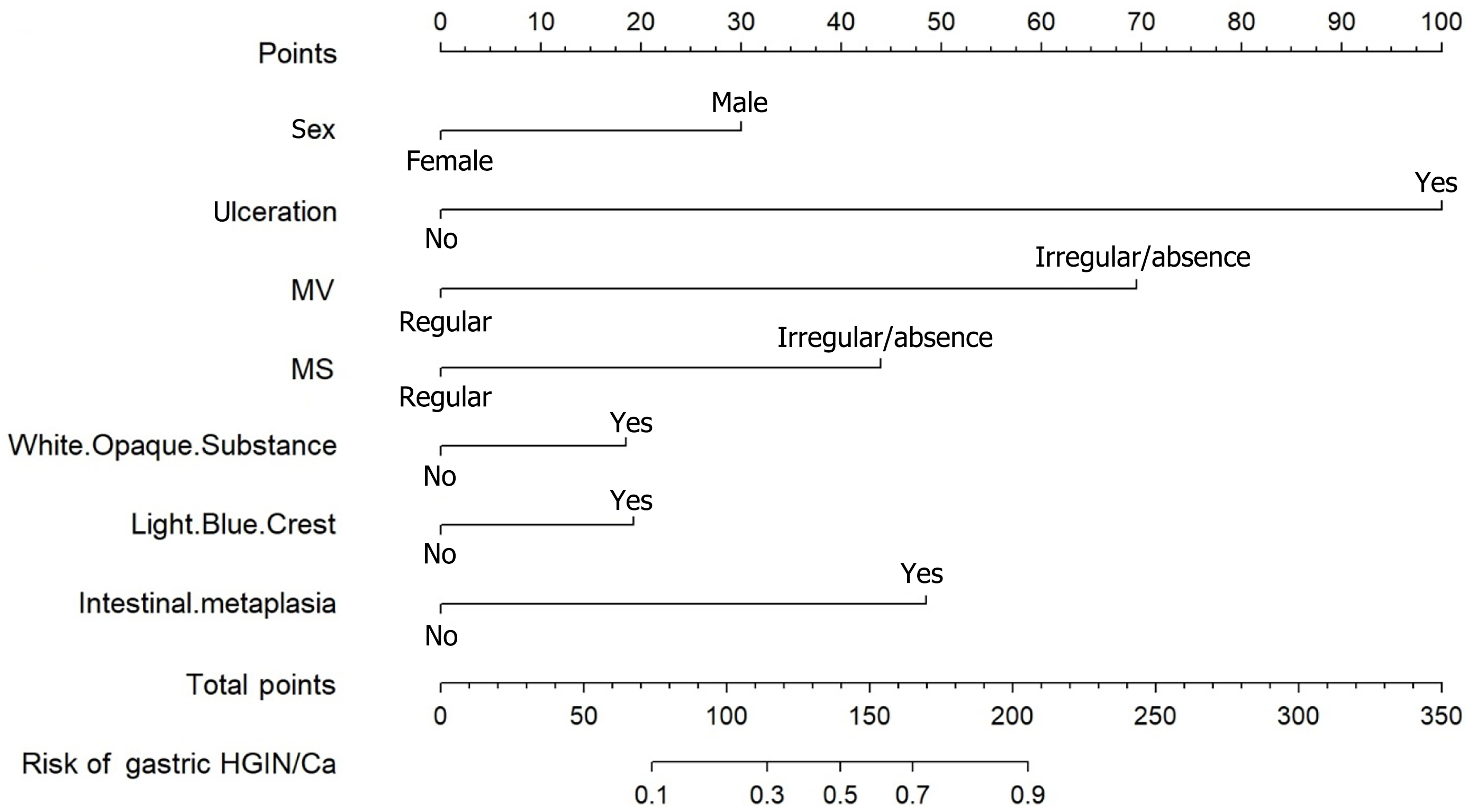
Figure 2 Nomogram of the stepwise logistic regression model.
An individual patient’s value is located on the axes for each variable, and a line is drawn upward to determine the number of points received for each variable value. The sum of these numbers is located on the Total Points axis, and a line is drawn downward to the Risk of Pathological Progression axis to determine the risk probability of high-grade intraepithelial neoplasia/cancer. MV: Microvascular; MS: Microsurface; HGIN: High-grade intraepithelial neoplasia; Ca: Cancer.
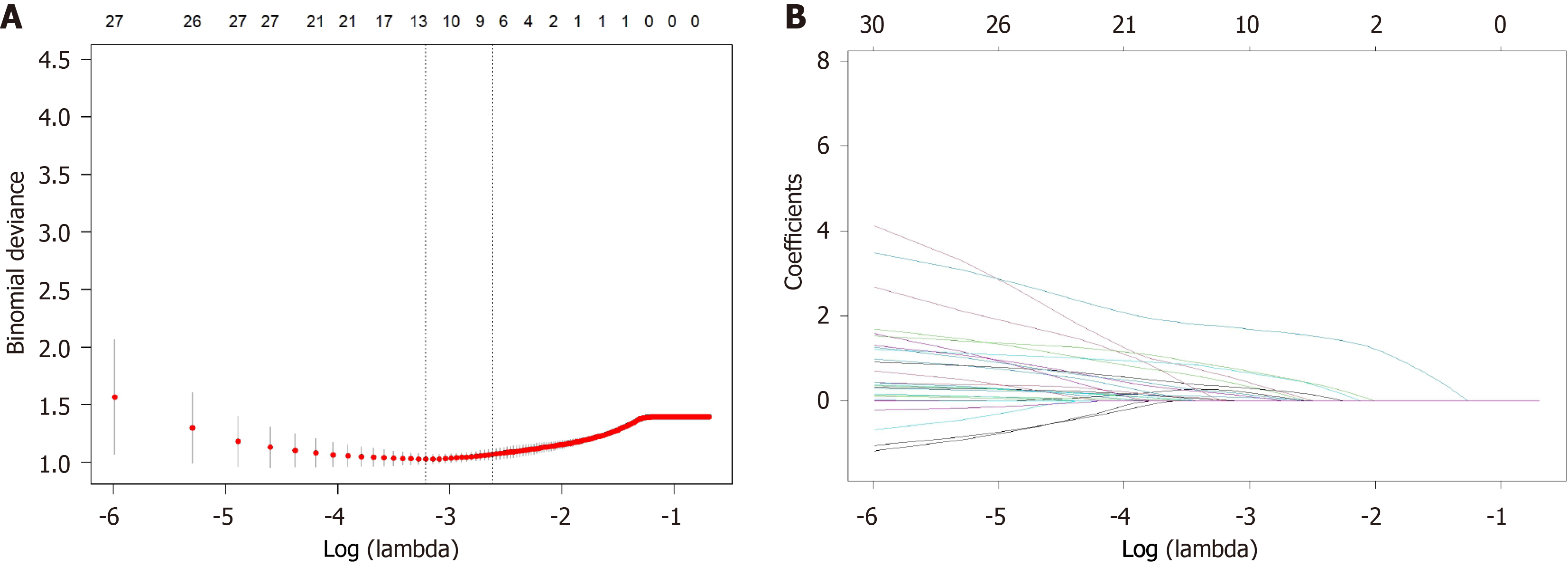
Figure 3 Demographic and clinical feature selection using the least absolute shrinkage and selection operator binary logistic regression model.
A: Optimal parameter (lambda) selection in the least absolute shrinkage and selection operator (LASSO) model used five-fold cross-validation through minimum criteria. The partial likelihood deviance (binomial deviance) curve was plotted vs log (lambda). Dotted vertical lines were drawn by the optimal values using the minimum criteria and the 1 SE of the minimum criteria (the 1-SE criteria); B: LASSO coefficient profiles of the 30 candidate features.
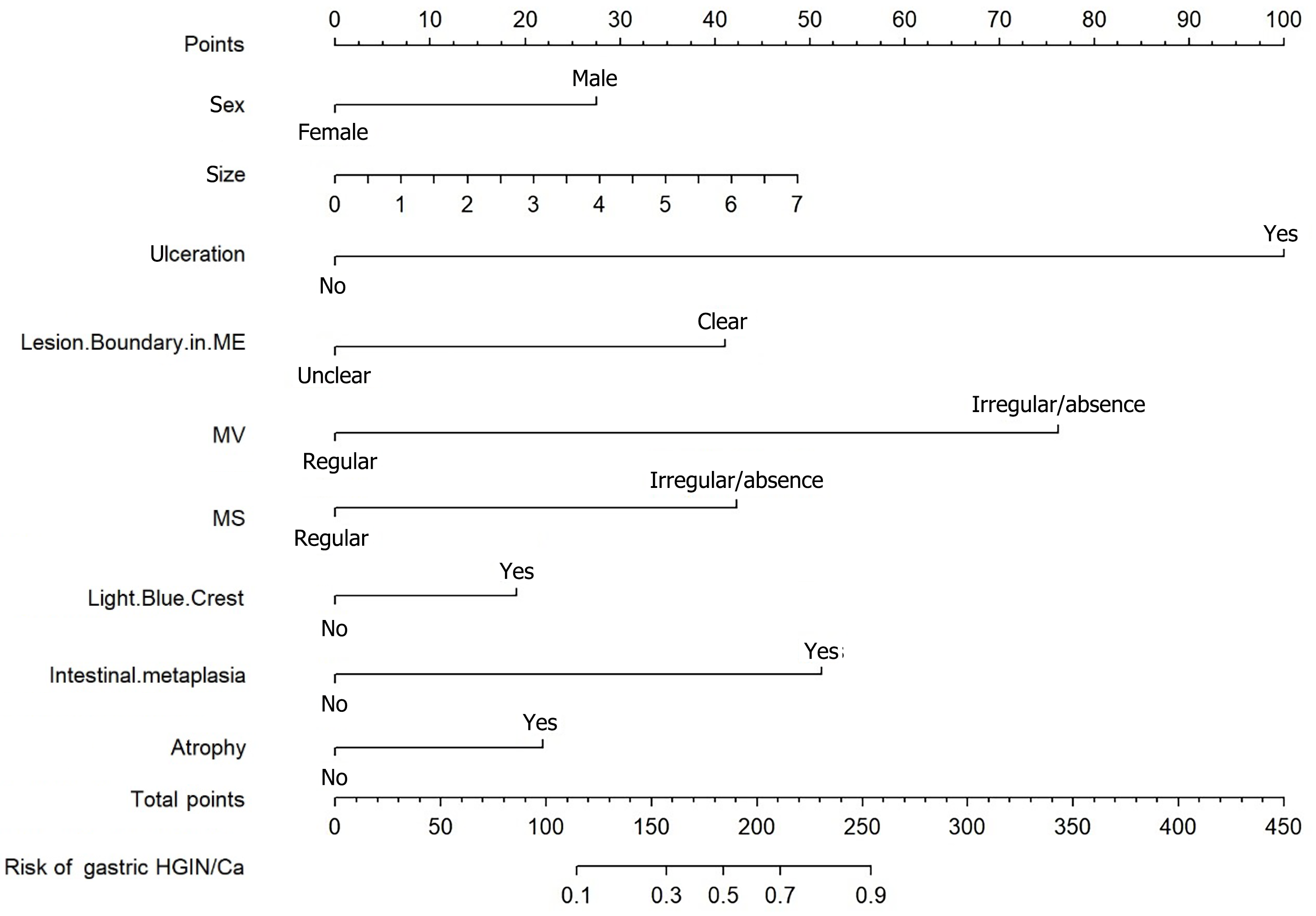
Figure 4 Nomogram of the least absolute shrinkage and selection operator regression analysis model.
An individual patient’s value is located on the axes for each variable, and a line is drawn upward to determine the number of points received for each variable value. The sum of these numbers is located on the total points axis, and a line is drawn downward to the Risk of Pathological Progression axis to determine the risk probability of high-grade intraepithelial neoplasia/cancer. ME: Magnifying endoscopy; MV: Microvascular; MS: Microsurface; HGIN: High-grade intraepithelial neoplasia; Ca: Cancer.
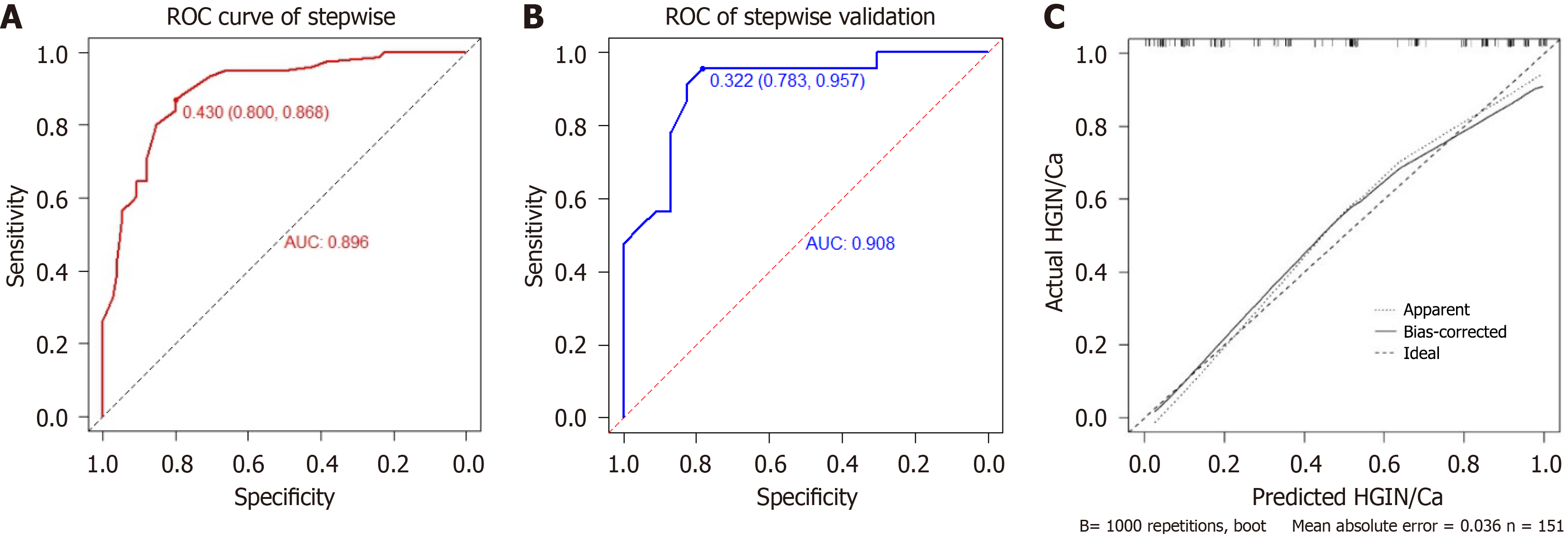
Figure 5 Evaluation of the performance of the nomogram in predicting the risk of pathologic upgrade in patients with gastric low-grade intraepithelial neoplasia in the logistic stepwise regression model.
A: The receiver-operating characteristic curve of the nomogram in the training cohort (area under the curve = 0.896); B: The receiver-operating characteristic curve of the nomogram in the internal validation cohort (area under the curve = 0.908); C: The calibration curve. ROC: Receiver-operating characteristic; AUC: Area under the curve; HGIN: High-grade intraepithelial neoplasia; Ca: Cancer.
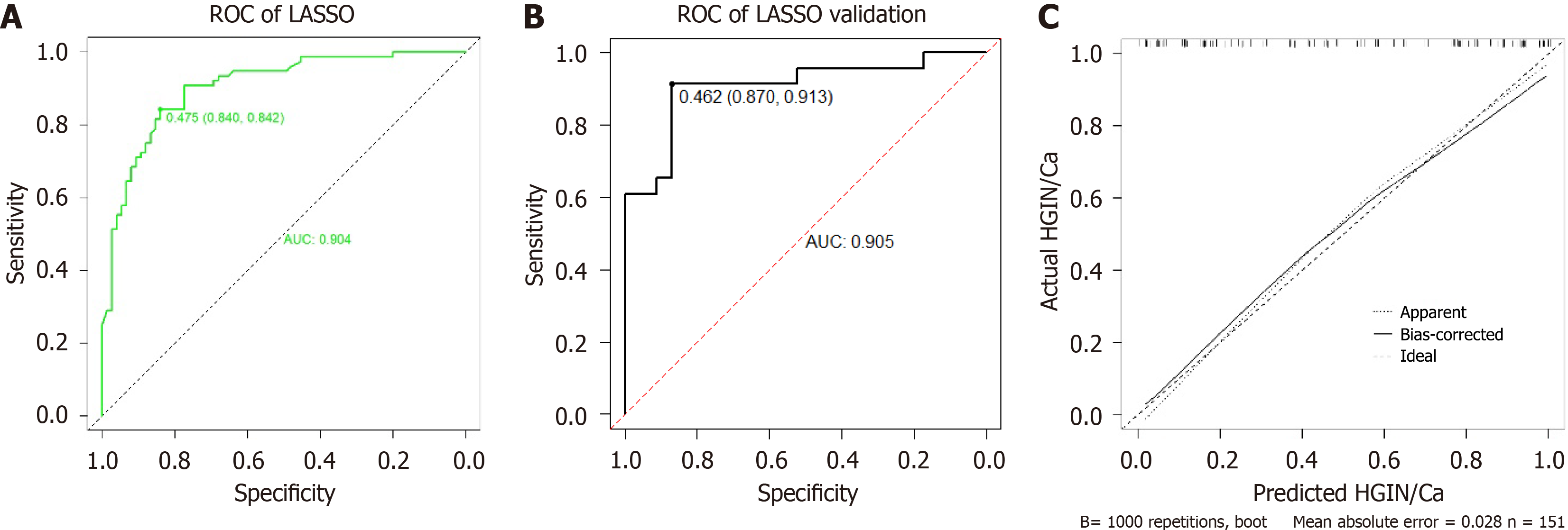
Figure 6 Evaluation of the performance of the nomogram in predicting the risk of pathologic upgrade in patients with gastric low-grade intraepithelial neoplasia in the least absolute shrinkage and selection operator regression model.
A: The receiver-operating characteristic curve of the nomogram in the training cohort (area under the curve = 0.904); B: The receiver-operating characteristic curve of the nomogram in the internal validation cohort (area under the curve = 0.905); C: The calibration curve. ROC: Receiver-operating characteristic; AUC: Area under the curve; HGIN: High-grade intraepithelial neoplasia; Ca: Cancer; LASSO: Least absolute shrinkage and selection operator.
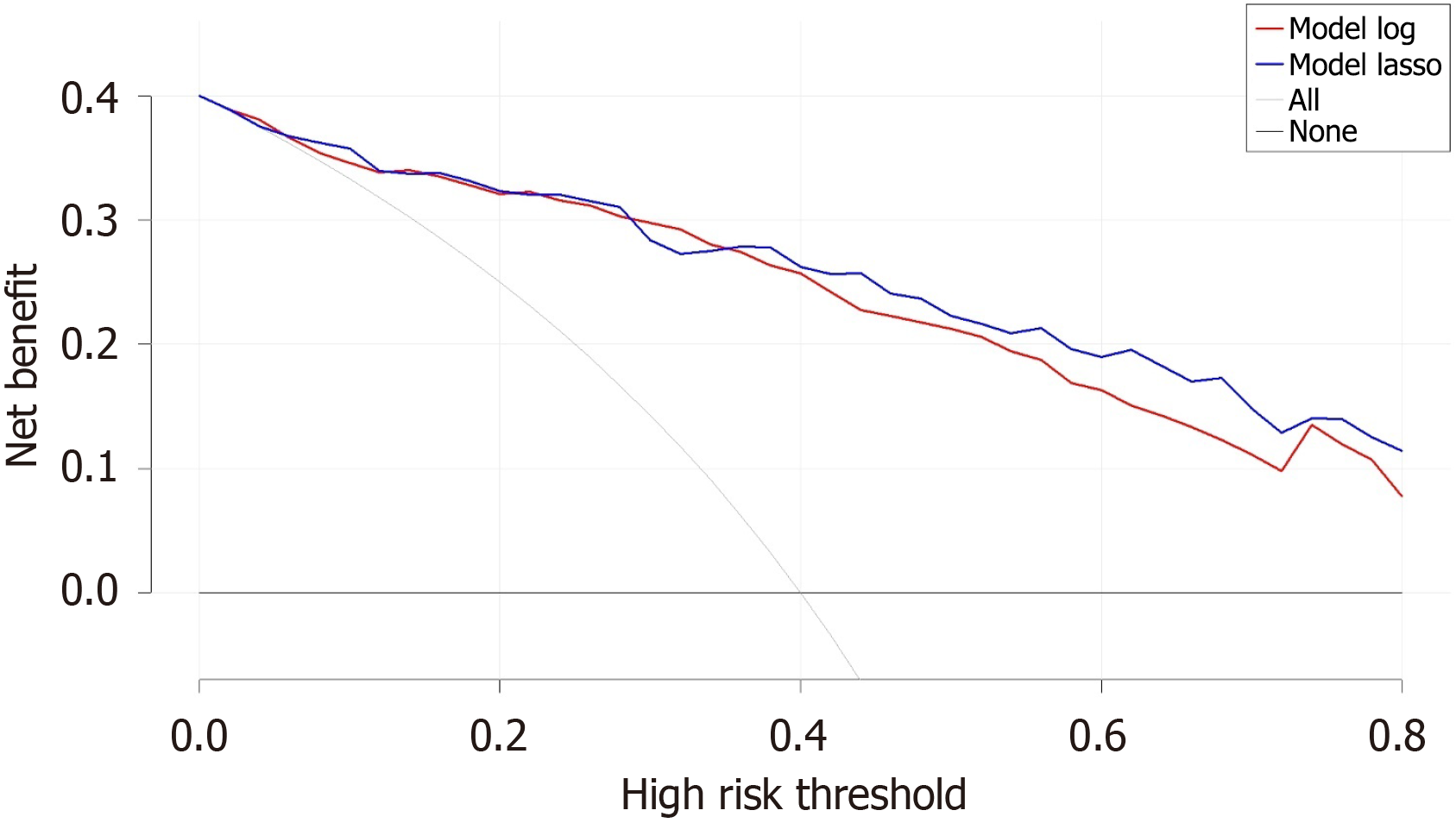
Figure 7 Decision curve analysis on the prediction models.
A high-risk threshold of 0.8 was set, above which clinically recommended endoscopic resection was advised. The gray curve represents the net benefit for all patients receiving endoscopic resection, while the black line indicates the net benefit (NB) when all patients were followed up. The red curve represents the NB based on intervention decisions made using a stepwise regression model, and the blue curve represents the NB based on intervention decisions made using the least absolute shrinkage and selection operator model.
- Citation: Lyu KM, Chen QQ, Xu YF, Yuan YQ, Wang JF, Wan J, Ling-Hu EQ. Development and validation of a predictive model for the pathological upgrading of gastric low-grade intraepithelial neoplasia. World J Gastroenterol 2025; 31(11): 104377
- URL: https://www.wjgnet.com/1007-9327/full/v31/i11/104377.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i11.104377