Copyright
©The Author(s) 2024.
World J Gastroenterol. Mar 7, 2024; 30(9): 1043-1072
Published online Mar 7, 2024. doi: 10.3748/wjg.v30.i9.1043
Published online Mar 7, 2024. doi: 10.3748/wjg.v30.i9.1043
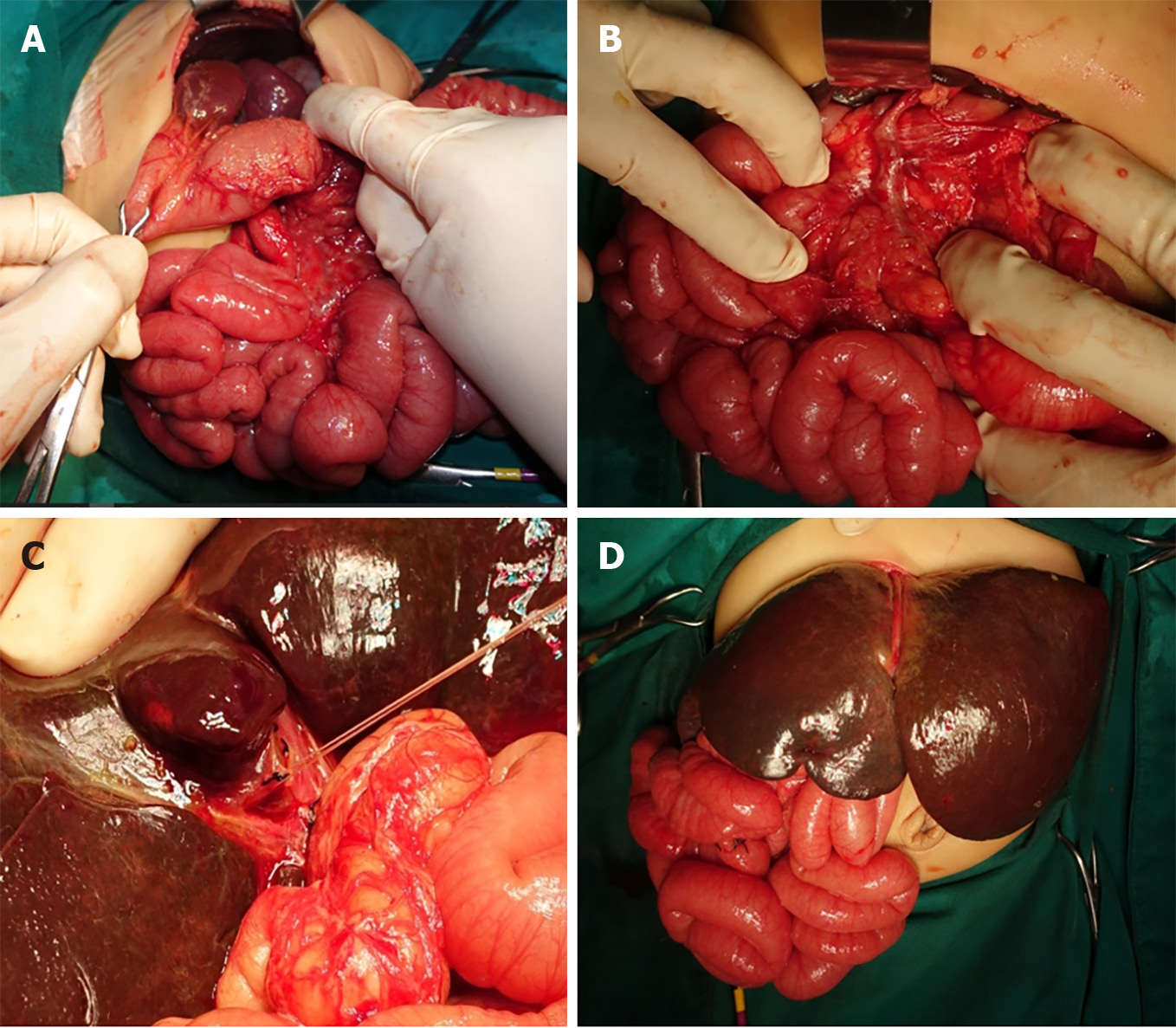
Figure 1 A term female infant with progressive jaundice and pale stool since birth.
At the age of 1 month 22 d, biliary atresia was diagnosed by intraoperative cholangiography and exploratory laparotomy for Kasai operation. A: Polysplenia; B: Preduodenal portal vein; C: Atretic gallbladder with a fibrous band; D: Situs ambiguous.
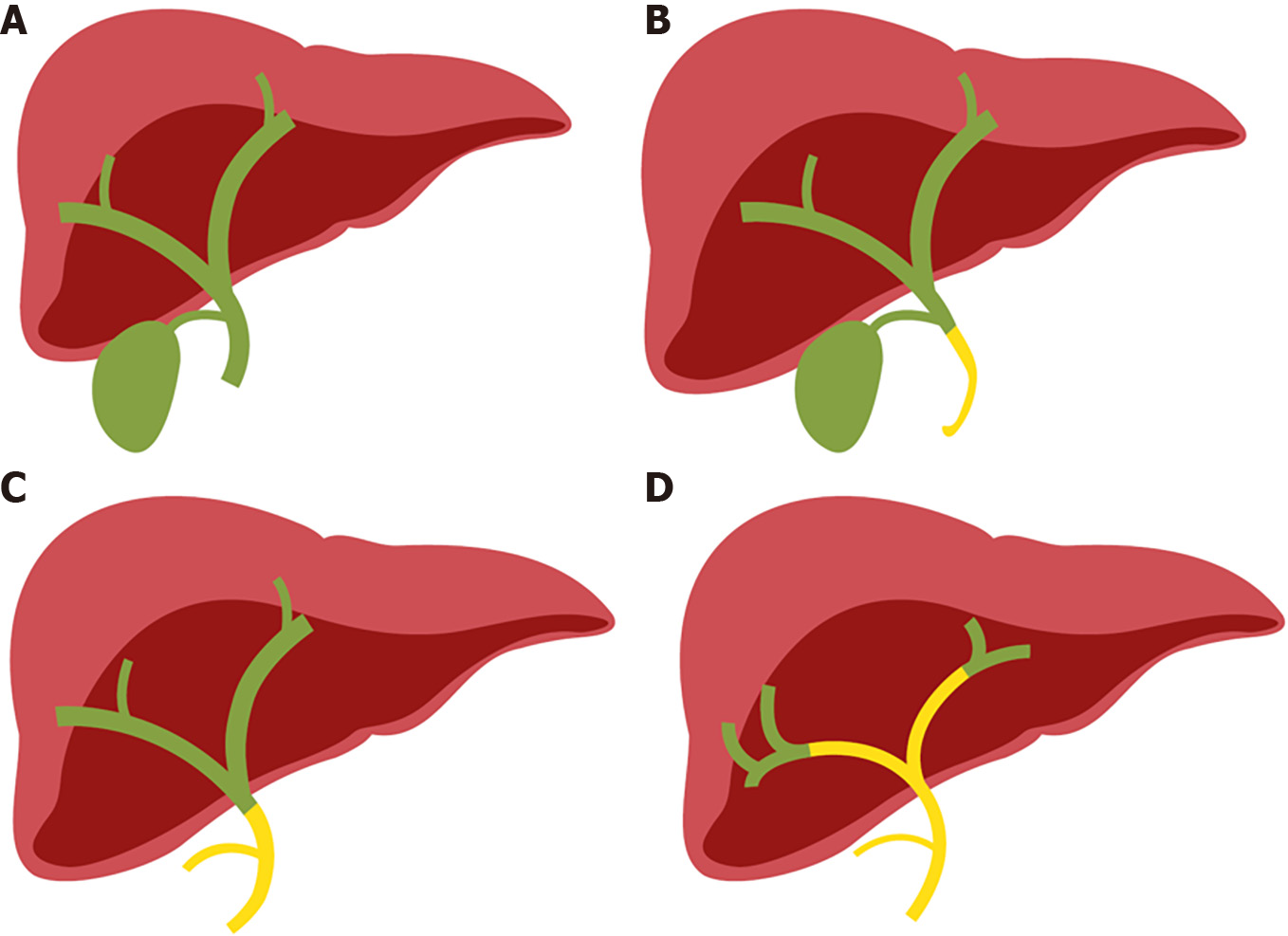
Figure 2 Type of biliary atresia classified by anatomical variants by the Japanese Society of Pediatric Surgeons.
A: Normal; B: Type I: 3%; C: Type II: 5%; D: Type III: 90%.
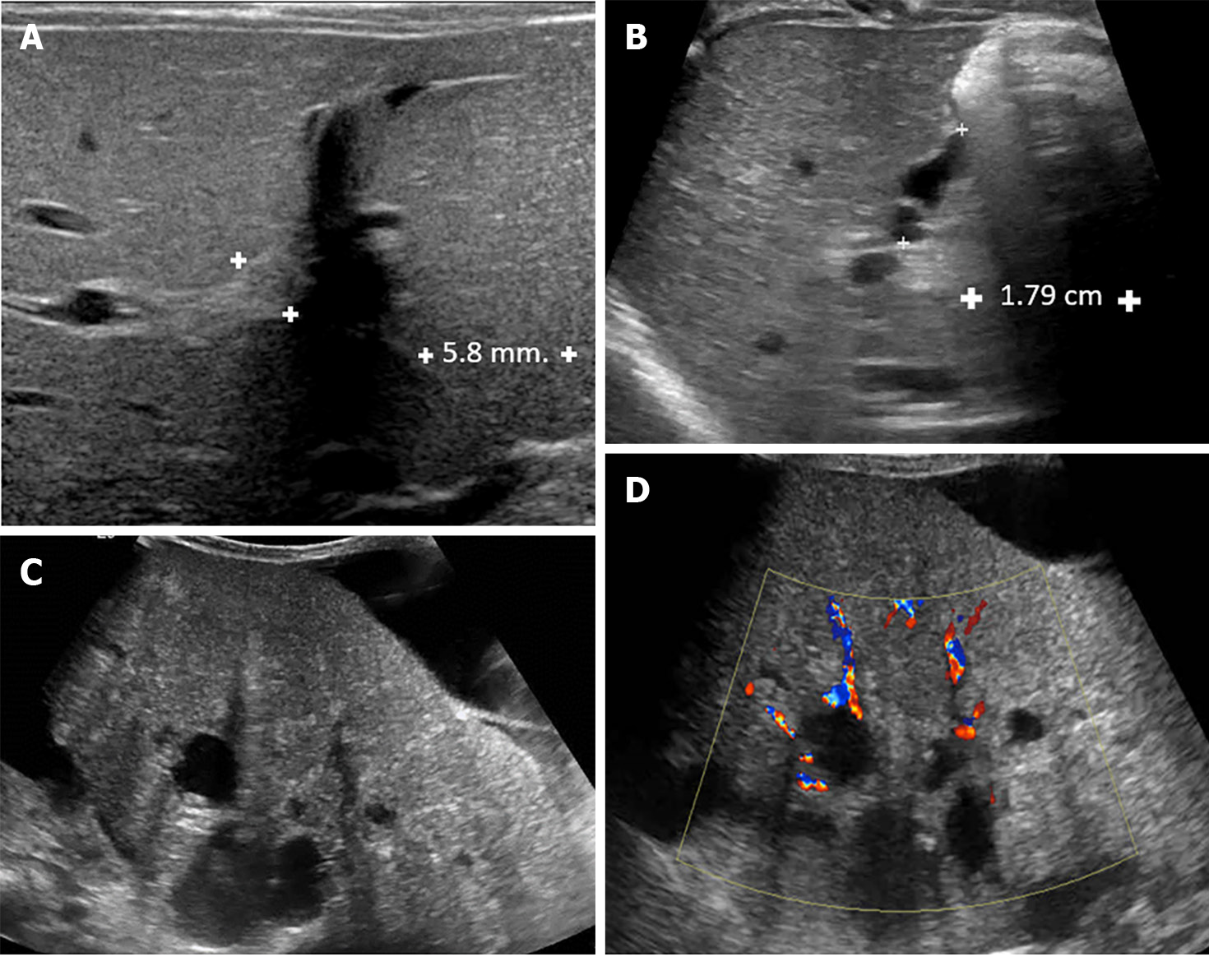
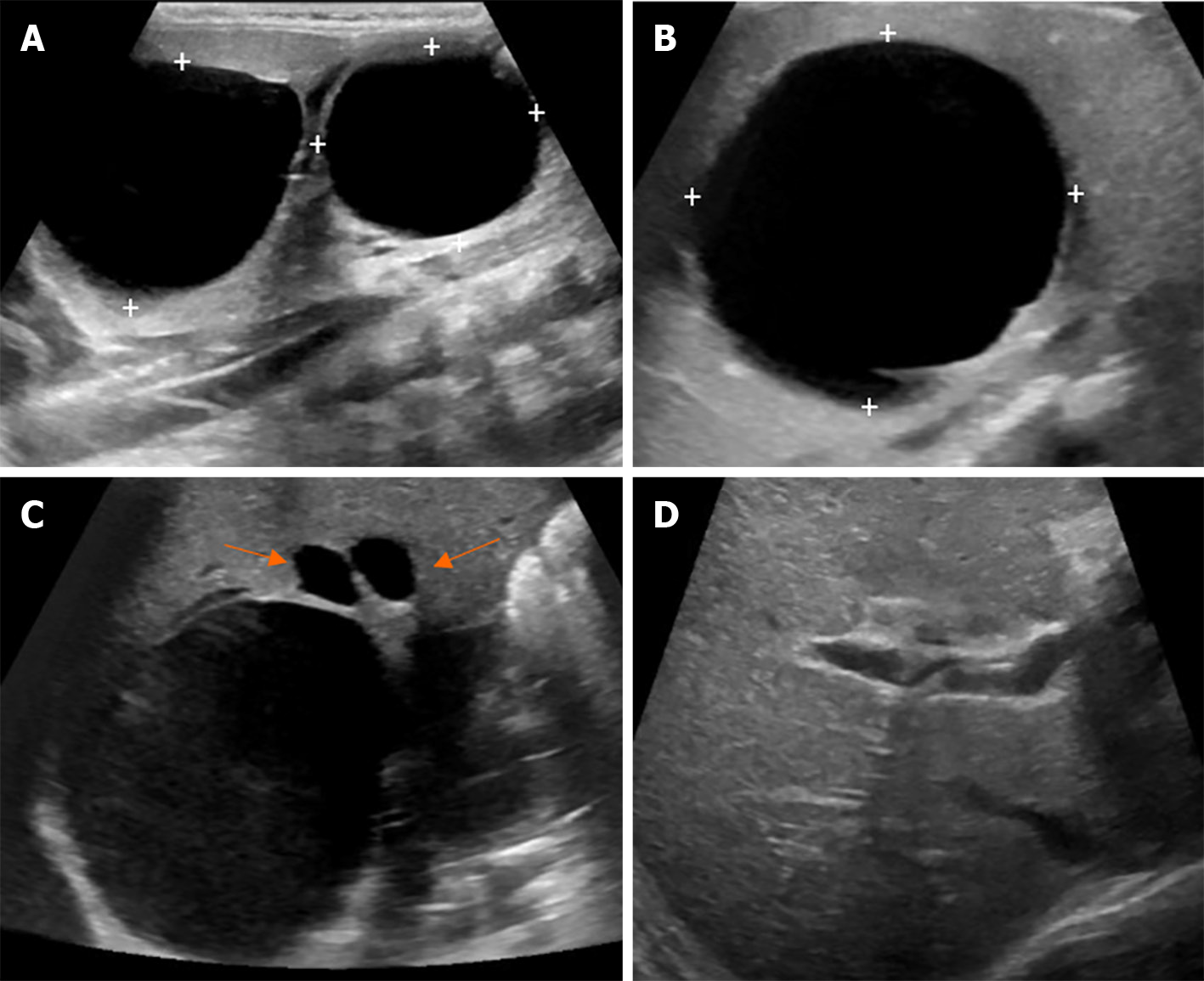
Figure 3 Ultrasound finding of biliary atresia.
A: A 25-d-old boy presented with prolong jaundice. Ultrasonography of the upper abdomen showed a thick echogenic band located anterior to the right portal vein and measuring approximately 5.8 mm in thickness, representing a positive triangular cord sign; B: A 49-d-old boy presented with prolonged jaundice and pale stools. Ultrasonography of the upper abdomen revealed: (1) A small size of gallbladder, measuring a maximal length of approximately 15.4 mm; (2) Lack of smooth, complete echogenic mucosal lining with an indistinct wall; and (3) Irregular gallbladder contour. These findings are consistent with a positive gallbladder ghost triad. The common bile duct was not visualized; C and D: An 11-month-old boy presented with clinical obstructive jaundice with abdominal distension. Ultrasonography of the upper abdomen revealed multiple irregular cystic lesions of various sizes in the central region of the right and left hepatic lobes and at the porta hepatis. Some cyst had echogenic content. Liver cirrhosis and ascites were noted.
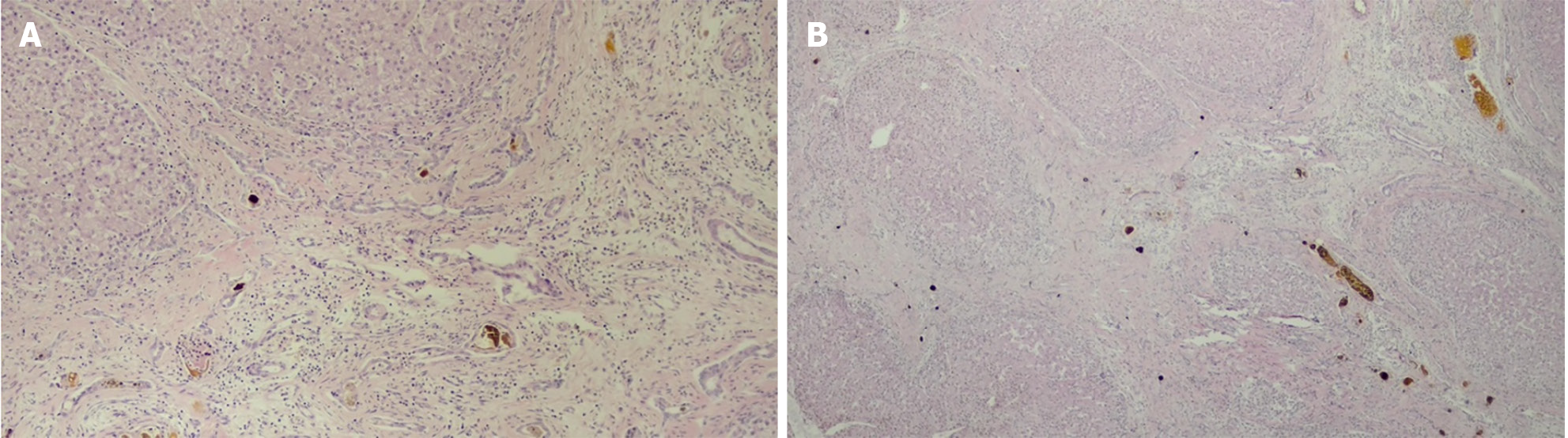
Figure 4 Histopathology of the liver in biliary atresia.
A: Ductular reaction and bile plug; B: Nodular, fibrosis and bile plug.
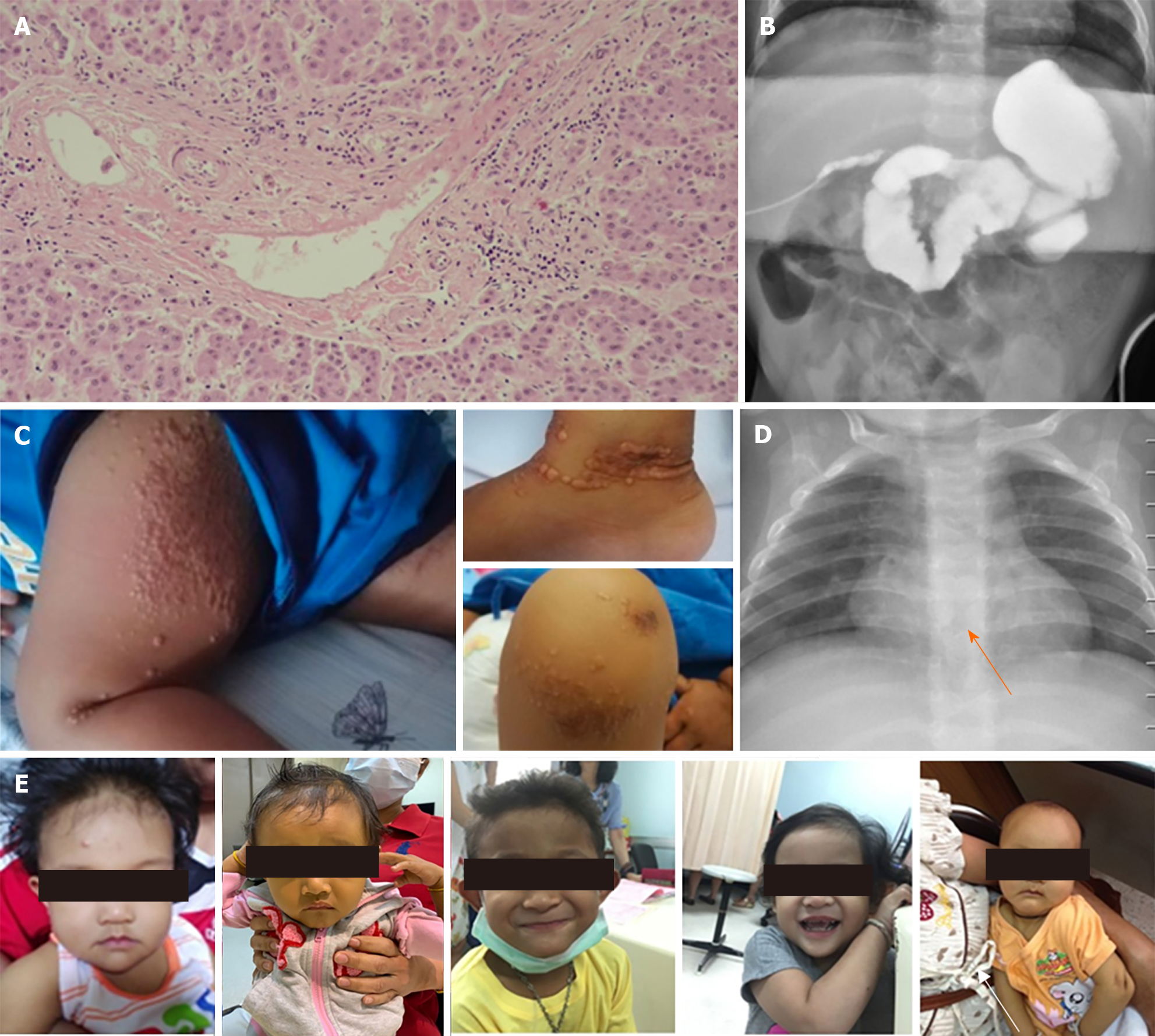
Figure 5 Characteristics of Alagille syndrome.
A: Bile duct paucity; B: A potential hypoplasia of the intralobular bile duct from intraoperative cholangiography; C: Xanthomas; D: A butterfly vertebra found on intraoperative cholangiography, the contrast was freely passing through the duodenal area and reasonably passing through the upper to the intrahepatic duct; E: Triangular face, deep-set eyes, hypertelorism, prominent forehead and point chin.
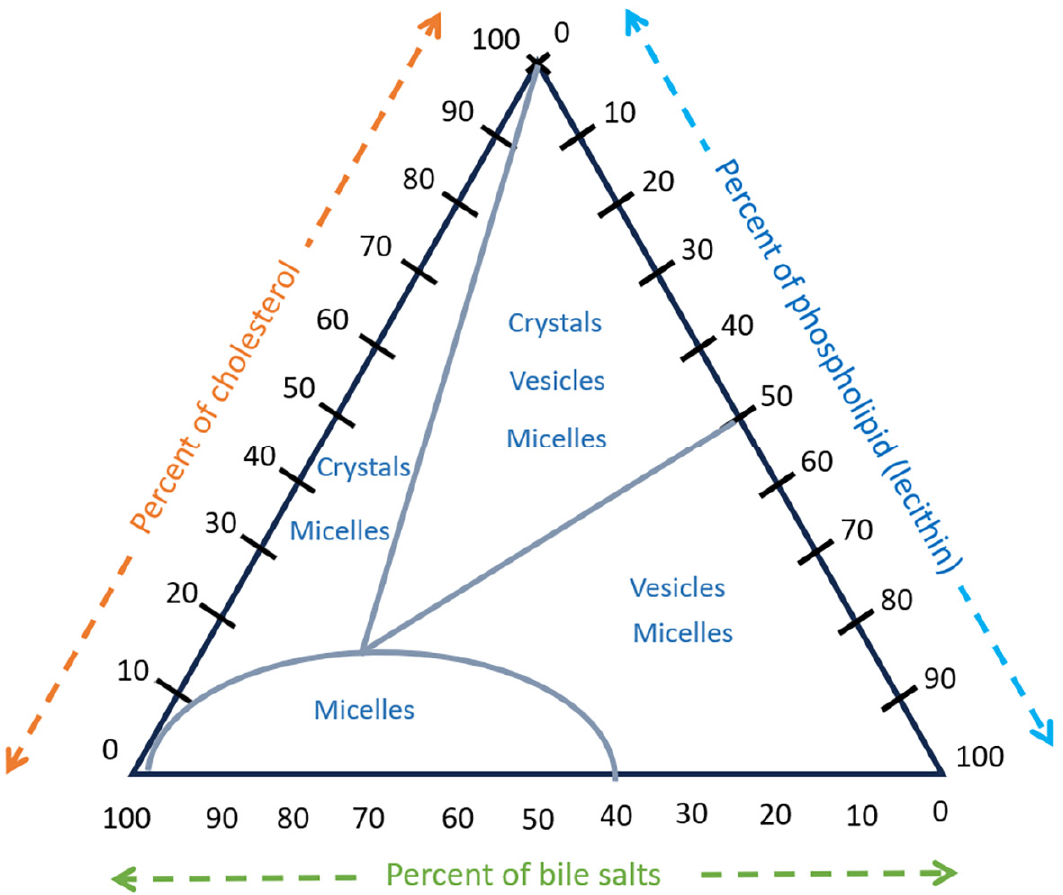
Figure 6 Percentage of the total moles of bile salt, lecithin, and cholesterol in bile composition.
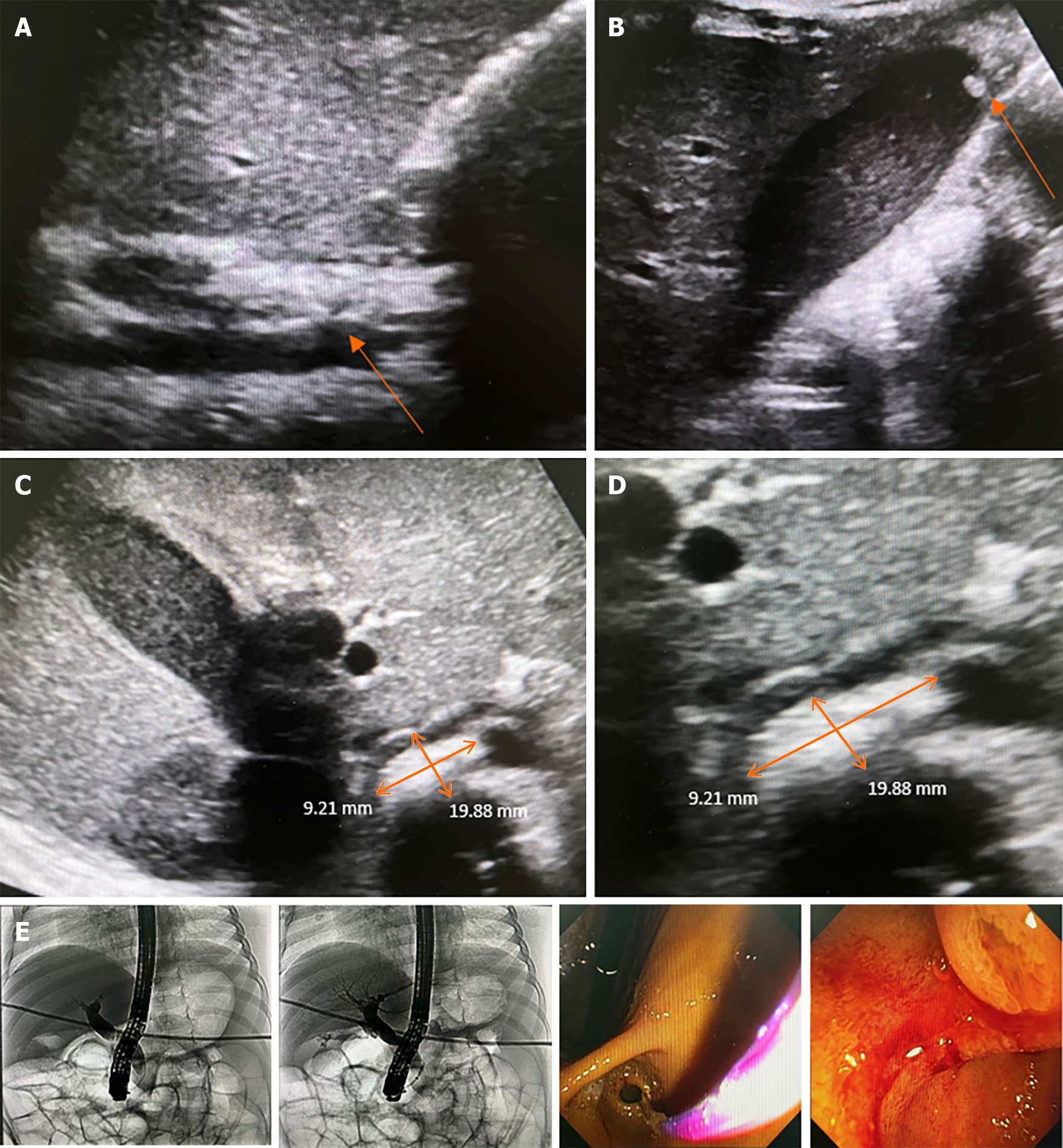
Figure 7 A 2-month-old female infant with anemia caused by chronic hemolysis.
Genetic analysis demonstrated heterozygous PKLR1 mutation/large deletion that was compatible with pyruvate kinase deficiency. Subsequently, she received regular blood transfusions every 3-4 wk. At the age of 3 years, the patient experienced intermittent abdominal pain, nausea, jaundice, and decreased appetite with no fever. Liver function test showed total bilirubin (TB) of 33.4, direct bilirubin (DB) of 31.2 mg/dL, aspartate aminotransferase of 270, alanine transaminase of 530, and alkaline phosphatase of 277 U/L. Abdominal ultrasonography showed marked splenomegaly, a dilated common bile duct (CBD) up to 0.9 cm in diameter, mild wall thickening, a suspected 2 cm × 0.9 cm distal CBD stone - well-distended gallbladder with bile sludge, and a 0.4 cm gallstone in the fundus. Subsequently, endoscopic retrograde cholangiography (ERCP) was performed, which revealed a bulging ampulla and CBD dilatation of 1 cm. The CRE balloon (12-15 mm) filled with 40 mL of air was placed for 60 s for sphincteroplasty. Later, balloon sweeping was performed, and small, blackish-pigmented stones were observed. After stone removal, the liver function test improved gradually as TB/DB 7.84/4.57 at 1 wk and normal values at 1 month. A: Dilated CBD, up to 9 mm, with mild wall thickening; B: A well-distended gallbladder with bile sludge and 0.4 cm stone at the fundus; C: A 2 cm × 0.9 cm distal CBD stone; D: A 2 cm × 0.9 cm distal CBD stone (zoom in); E: ERCP with CBD dilation with 12-15 mm CRE balloon filled with 40 mL of air placed for 60 s as sphincteroplasty.
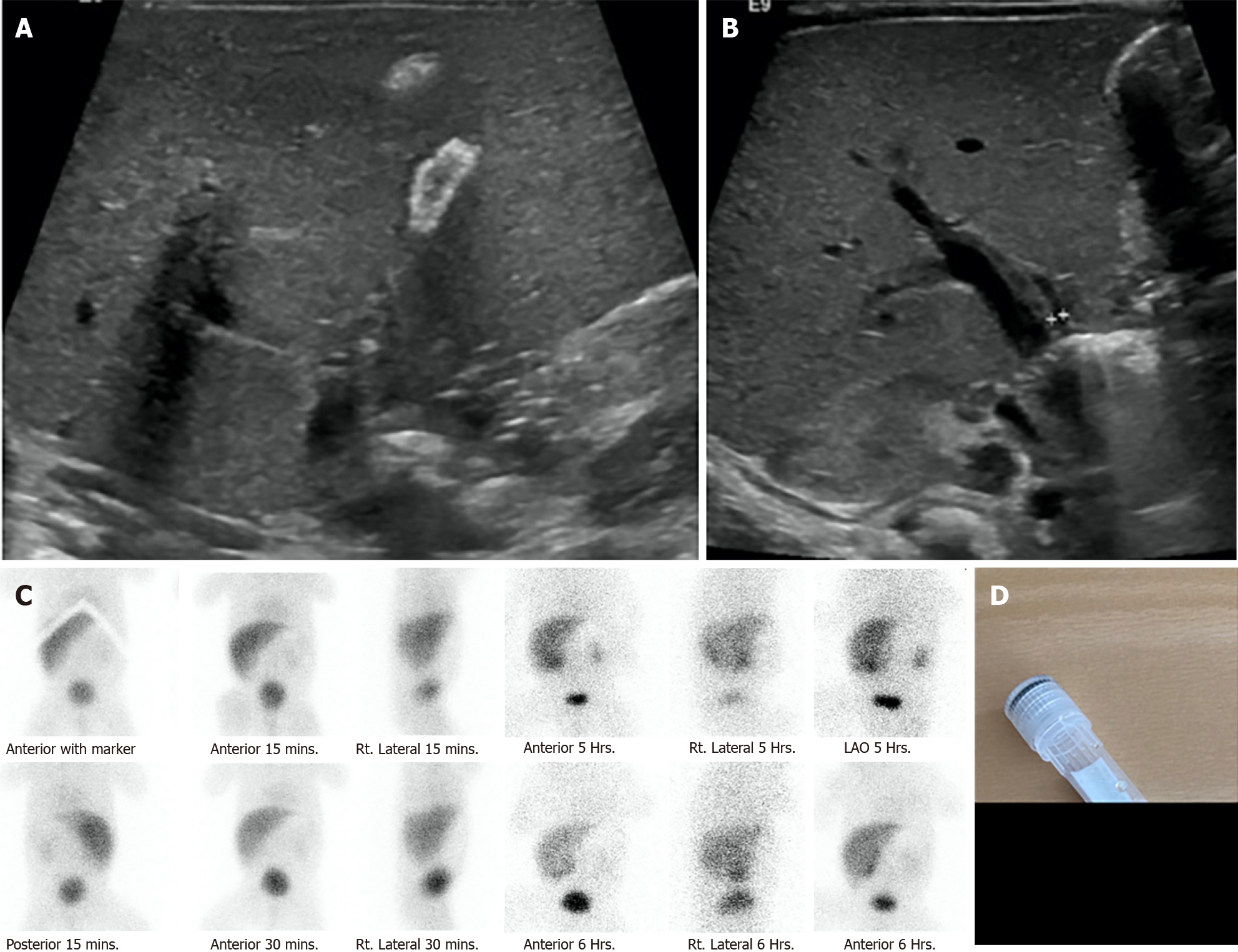
Figure 8 A 3-year-old girl was diagnosed with tetralogy of Fallot and brain abscess.
She was admitted for intravenous antibiotic therapy, including ceftriaxone 100 mg/kg/d and metronidazole 30 mg/kg/d for 6 wk. After 3 wk of ceftriaxone administration, she experienced intermittent colicky pain in her right upper abdomen and ultrasonography showed an enlarged gallbladder with multiple gallstones in the posterior dependent part extending to the gallbladder neck. A: Multiple gallstones; B: Enlarged gallbladder measuring 6.3 cm in length, 1.5 mm gallbladder wall, and no pericholecystic fluid; C: Enlarged gallbladder with multiple gallstones in the posterior dependent part extending to gallbladder neck; D: Multiple gallstones.
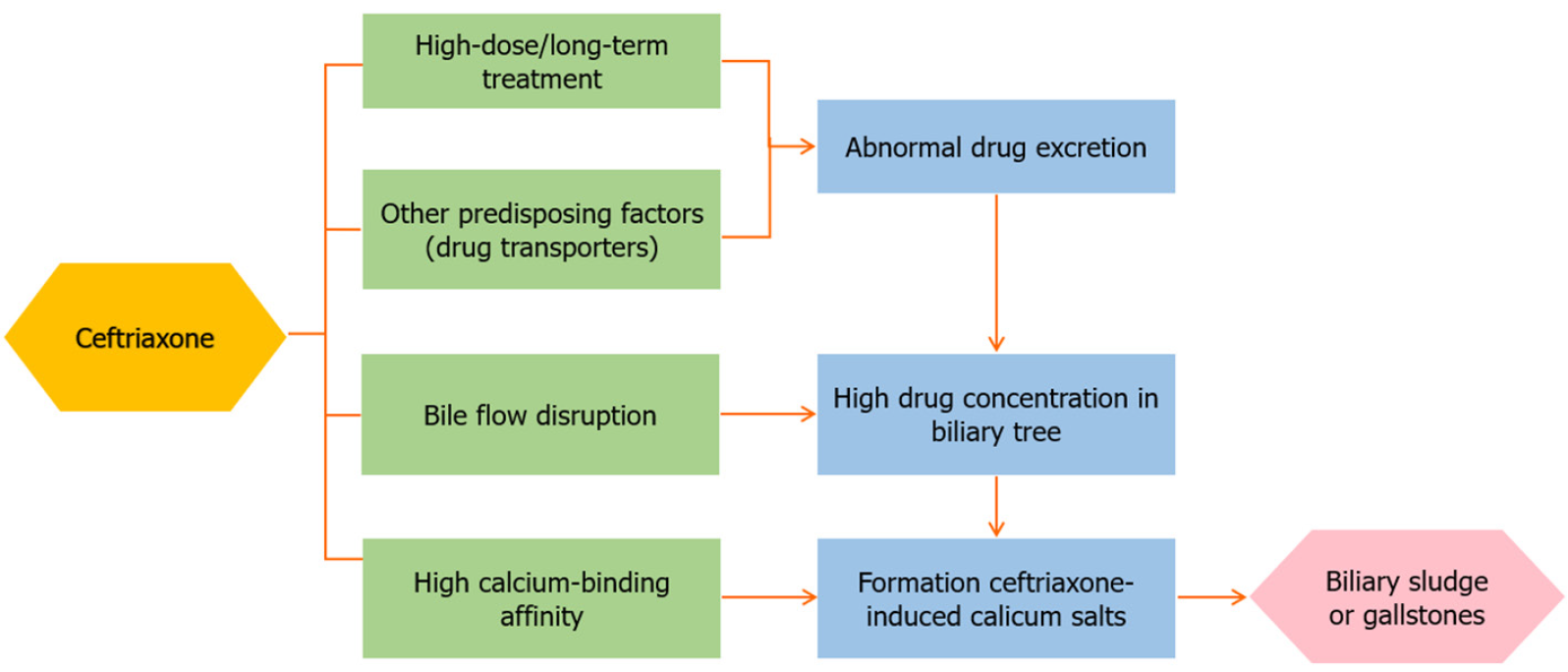
Figure 9 Ceftriaxone excretion in the biliary tract.
Figure 10 A 29-wk preterm newborn with neonatal sepsis, stage IIA necrotizing enterocolitis, bronchopulmonary dysplasia on the endotracheal tube, and prolonged total parenteral nutrition.
He had obvious jaundice and pale stool at 1 month of age. Liver function test showed total bilirubin (TB)/direct bilirubin (DB) values of 8.7/4.6 mg/dL, aspartate aminotransferase of 132, alanine aminotransferase of 52, alkaline phosphatase of 447 U/L, and albumin of 2.8 mg/dL. Intraoperative cholangiography was performed after 3 months of and showed a patent bile duct but the formation of large stone. The histopathology of liver biopsy revealed giant cell transformation with cholestasis in the bile canaliculi and hepatocytes, bile ductopenia, and absence of significant fibrosis. He underwent an eye examination by an ophthalmologist who found the posterior embryotoxon at the inferior of the eyes. The trio-exome showed a NOTCH2 mutation. After stone removal, TB and DB dramatically decreased to normal level in 7 d. A: Ultrasonography showing a small gallbladder with a diffused calcified wall; B: Ultrasonography showing non-dilatation of the intrahepatic or common bile duct (only 3 mm); C: Technetium-99m di-isopropyl iminodiacetic acid shows faint radiotracer excretion into the gastrointestinal tract; D: Gross stone specimen.
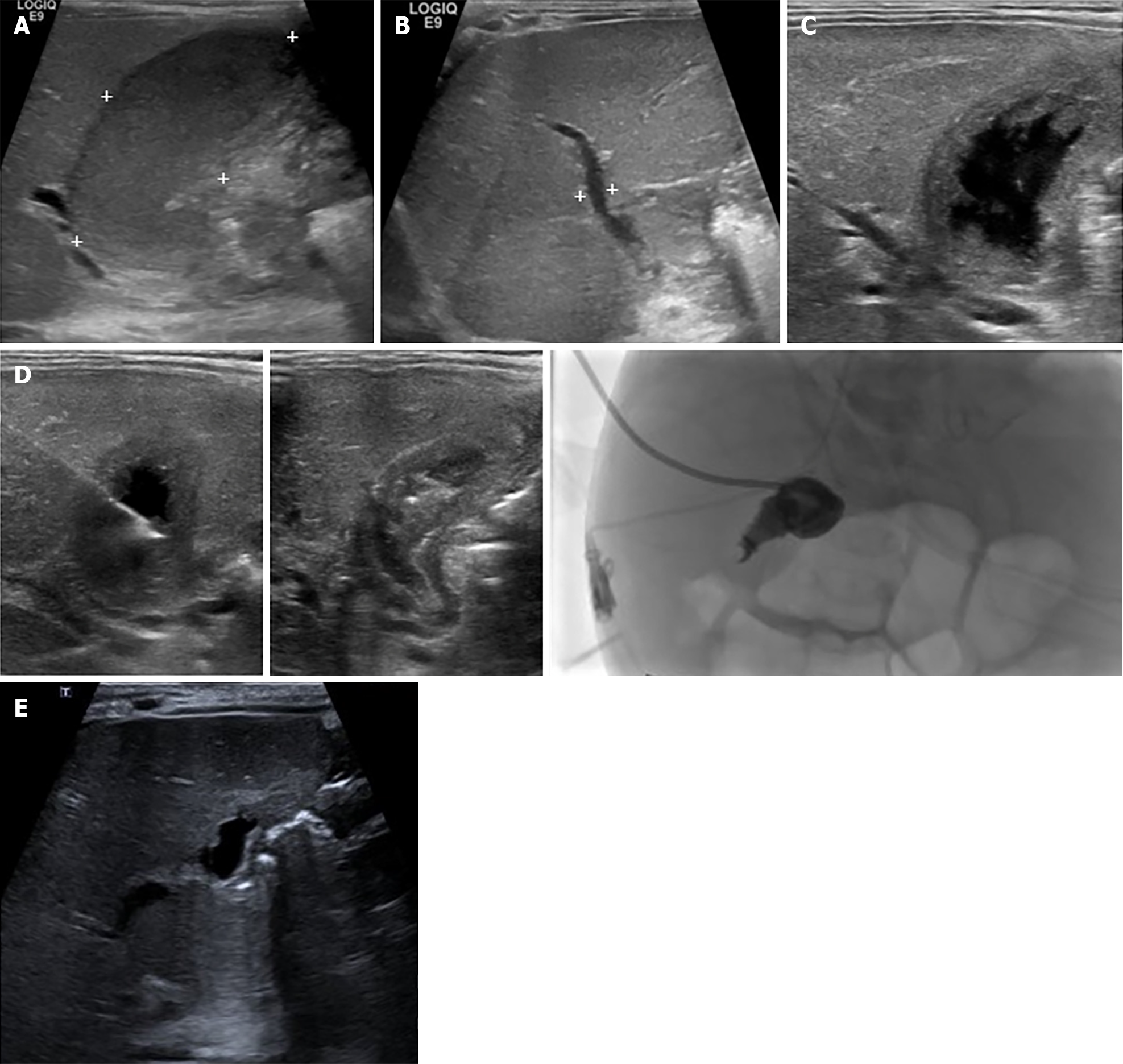
Figure 11 A 30-wk old male infant, with a birth weight of 1130 g, had a short bowel syndrome caused by necrotizing enterocolitis stage IIIB with multiple small bowels, and colonic, and cecal perforations.
He underwent multiple exploratory laparotomies with severe intra-abdominal adhesion. At the age of 3 months, he experienced jaundice and multiple episodes of sepsis. Abdominal ultrasonography revealed a marked distended gallbladder containing bile sludge with mucocele, as hydrops gall bladder, with no bile duct dilatation. The maximum total bilirubmin/direct bilirubin (TB/DB) was 28/23 mg/dL, with unclear sepsis. Percutaneous transhepatic cholecystostomy was performed. After the procedure, sepsis was clear, and TB/DB gradually returned to normal levels within 2 months. Before percutaneous cholecystostomy. A: Hydrops gallbladder 5.4 cm × 2 cm (markedly distended gallbladder with bile sludge); B: Mild dilatation ofz the common bile duct measured 3.2 mm in diameter; C: Percutaneous cholecystostomy via a transhepatic approach; D: A 6-F percutaneous cholecystostomy catheter was inserted over 0.035 Terumo wire with its tip located in the gallbladder. A 5 mL aliquot of dark bile was aspirated; then, a drainage catheter was placed in the gallbladder and connected to the drainage bag and cholecystography was performed; follow-up 1.5 years after percutaneous cholecystotomy; E: Small, lobulated gallbladder.
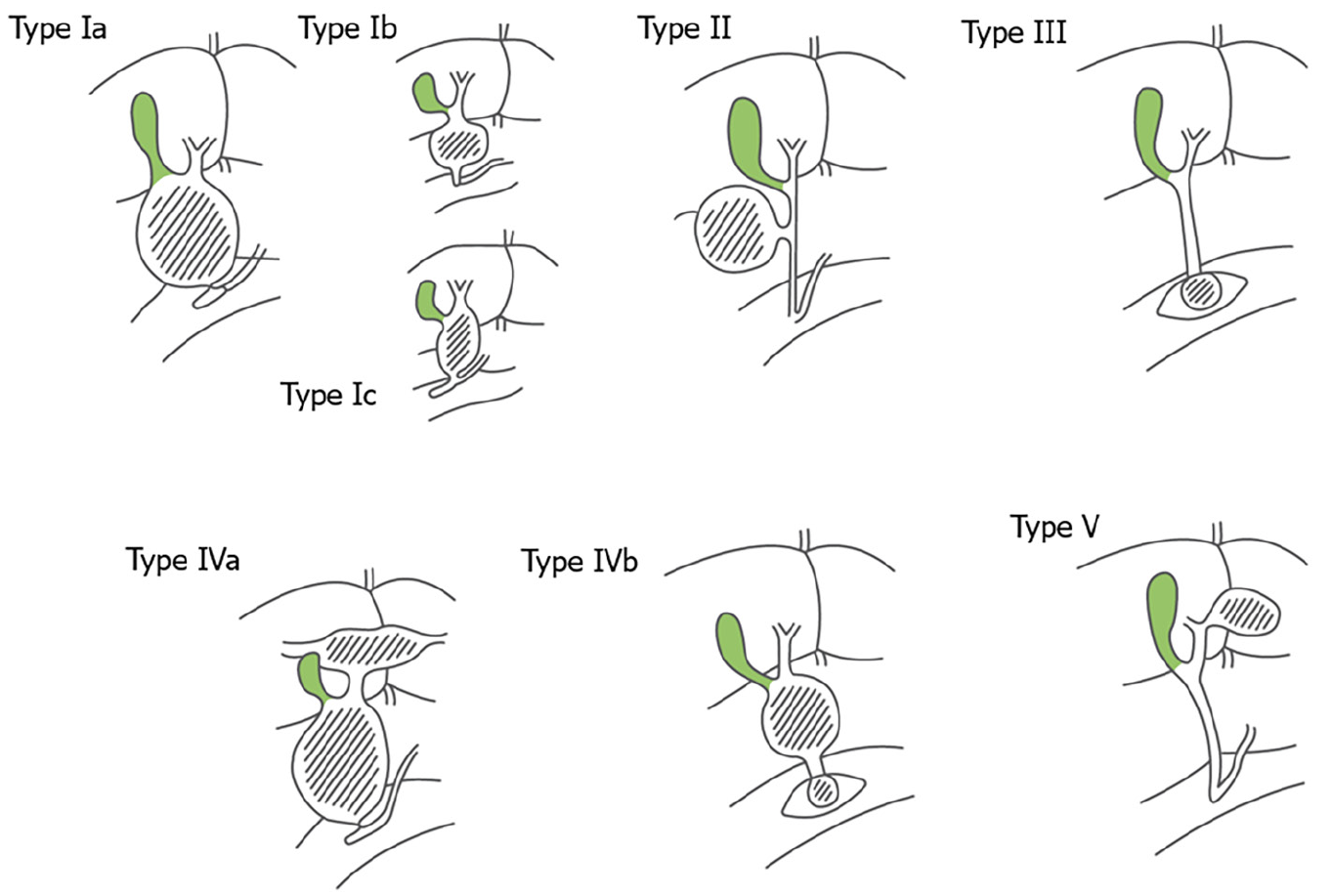
Figure 12 Todani classification of choledochal cysts.
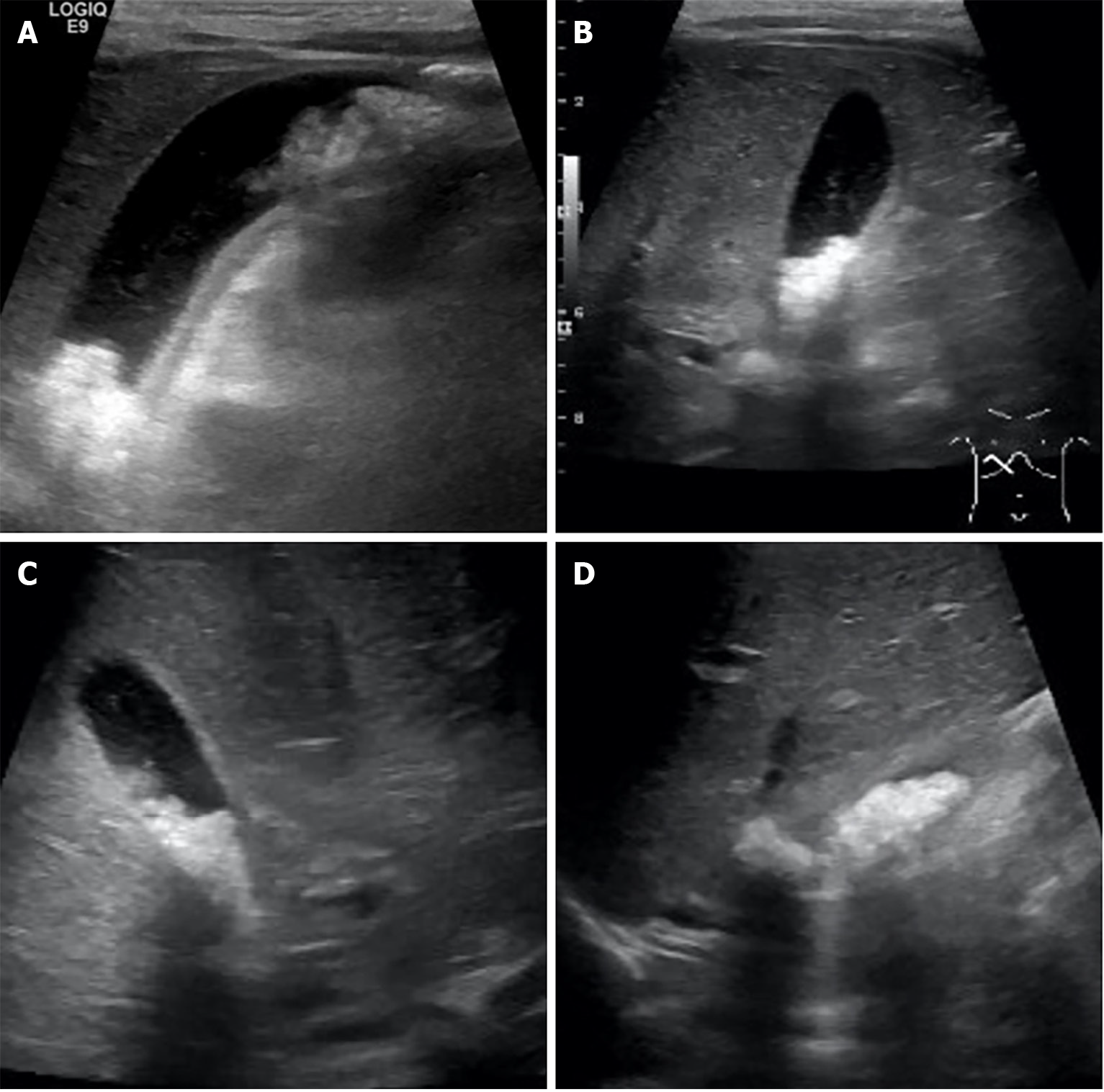
Figure 13 A term female infant with hepatic cyst detected by prenatal ultrasonography, presented with jaundice since birth.
Repeated abdominal ultrasonography showed fusiform dilatation of extrahepatic and intrahepatic bile ducts, 3.3 cm × 4.5 cm, suggestive of choledochal cyst type IVa (Todani’s classification), containing bile sludge, and another large hepatic cyst in segment IV, 4.7 cm × 4.3 cm. After conservative treatment, clinical jaundice progressed. Liver function test showed total bilirubin/direct bilirubin (TB/DB) of 10.9/1.68 mg/dL, aspartate aminotransferase of 45, alanine aminotransferase of 23, alkaline phosphatase of 150, gamma-glutamyltransferase of 172 U/L, and albumin of 3.9 mg/dL. Computed tomography revealed a cystic lesion measuring 3.7 cm × 5 cm × 4 cm, at the common bile duct area, slight bilateral intrahepatic duct dilatation, a smooth thin wall hypodense lesions measuring 5.1 cm × 4.6 cm × 4.3 cm at hepatic segment 4a/8, and a few small hypodensity lesions at segment 7 that were suspected to be an infected hepatic cyst. After percutaneous aspiration of the hepatic cyst and intensive antibiotics, the cyst enlarged to 5.4 cm × 5.8 cm. Finally, choledochal cyst excision with Roux-en-Y hepaticojejunostomy of the subcutaneous limb was performed. One year later, ultrasonography revealed a reduction in the size of the lobulated cystic lesion to size 2.9 cm × 2.8 cm × 2.1 cm and mild dilatation of the intrahepatic bile ducts at the porta hepatis region. A: Fusiform dilatation of the extrahepatic cyst and intrahepatic bile ducts, measuring 3.3 cm × 4.5 cm, containing bile sludge; B: Another large cyst, 4.7 cm × 4.3 cm, in hepatic segment IV; C: Decreased size of the lobulated cystic lesion at the porta hepatis region with a few small hypoechoic lesions surroundings the cystic lesion, probably cysts or focal IHD dilatation; D: Mild dilatation of the intrahepatic bile ducts at the porta hepatis region.
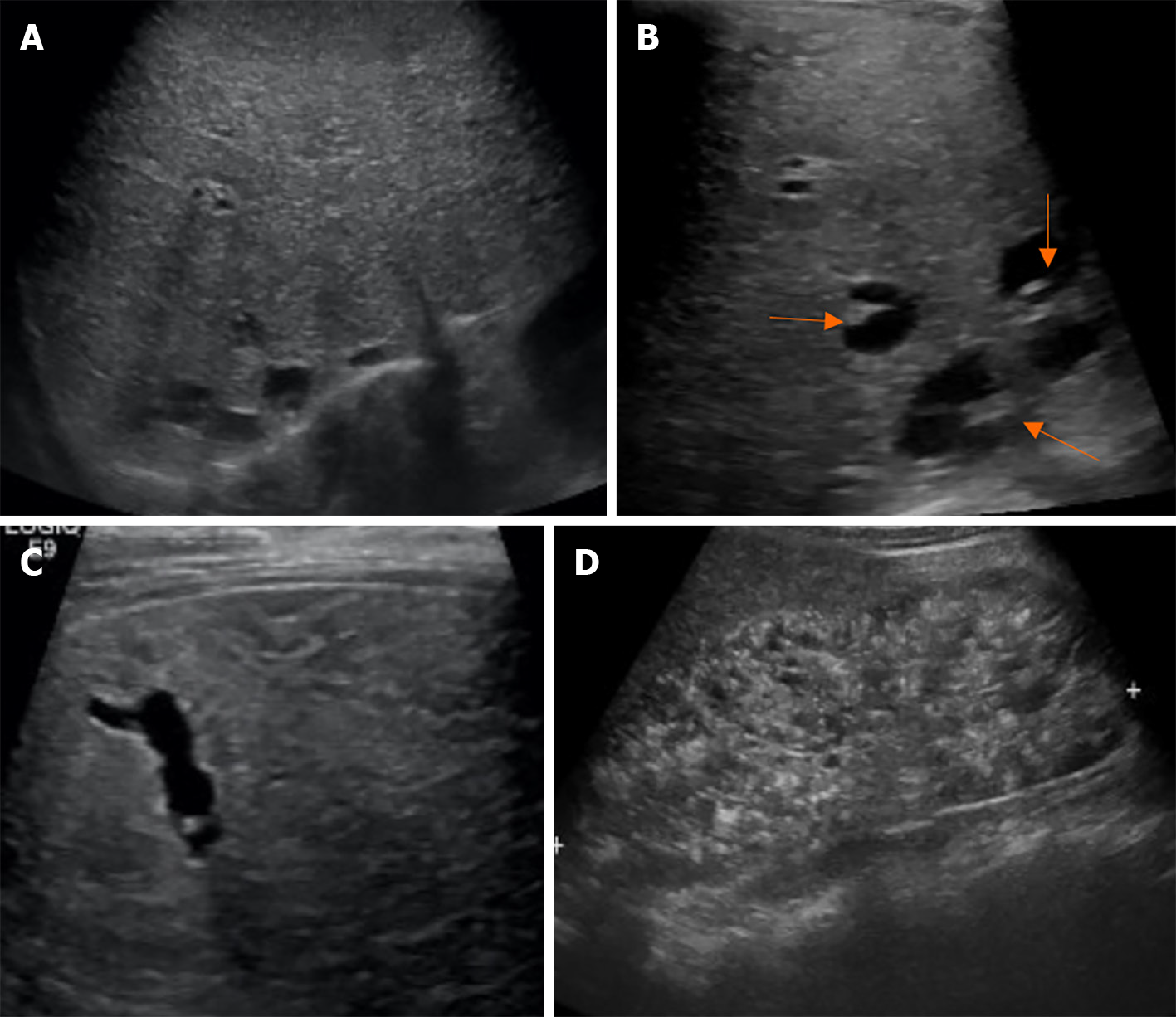
Figure 14 A 32-wk-old female infant with a family history of consanguinity, presented with an abdominal mass.
She was diagnosed with Calori syndrome (congenital hepatic fibrosis, choledochal cyst type V, and multiple cysts in the kidneys). Abdominal ultrasonography revealed enlargement of the left hepatic lobe, coarse parenchymal echotexture with a periportal hyperechoic band, small cysts in a posterosuperior segment of the right hepatic lobe, and marked enlargement of both kidneys with evidence suggestive of multi-cystic kidney disease. She had upper gastrointestinal bleeding from esophageal varices that can be controlled with esophageal ligation at the 8-year follow-up. A: Diffusely enlarged liver and coarse parenchymal echogenicity with several round and tubular cystic-like structures; B: Focal intrahepatic dilatation with central dot sign; C: Tubular cystic-like structures; D: Markedly enlarged kidneys with loss of corticomedullary differentiation, and multiple cysts in the medulla and cortices.
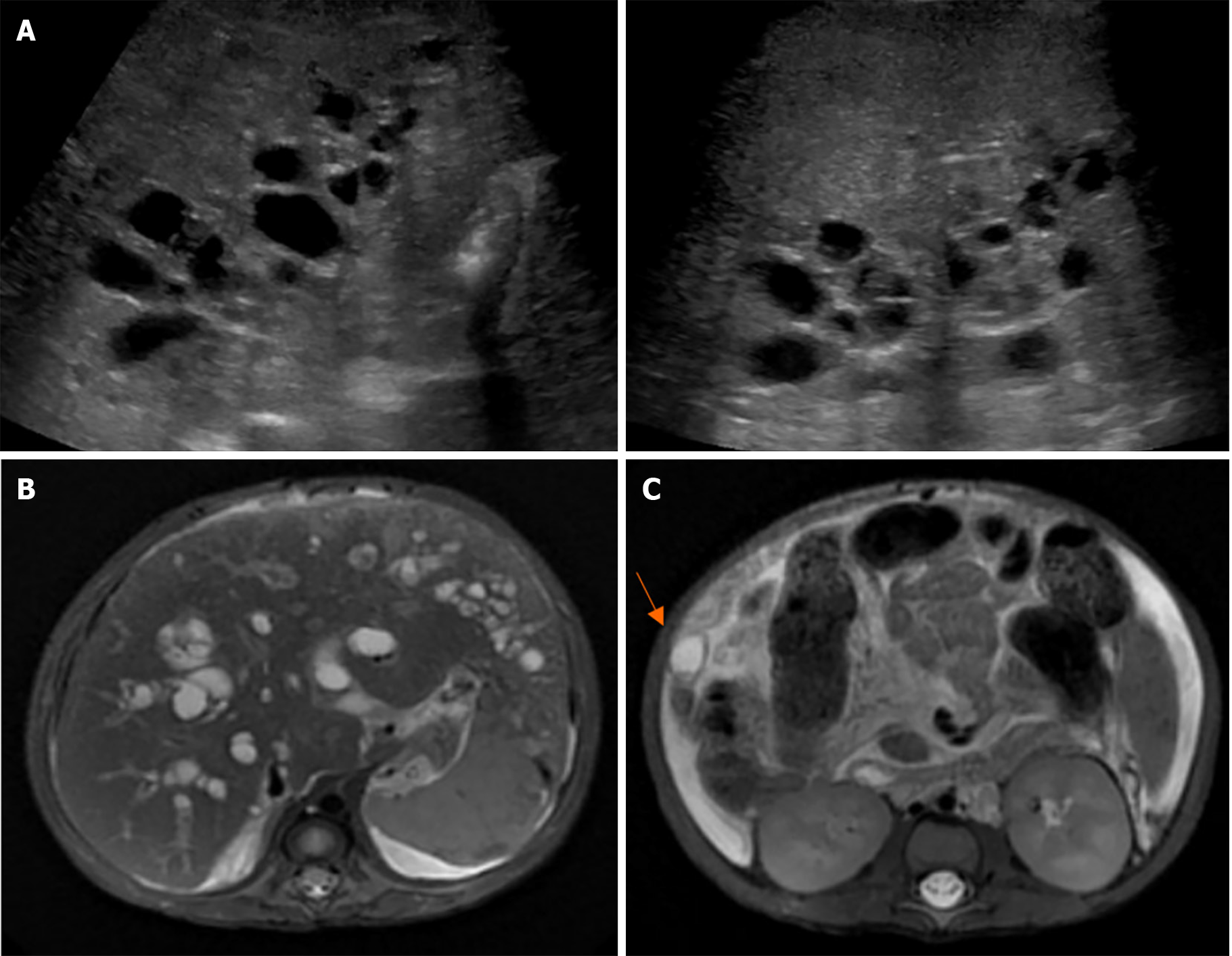
Figure 15 A 2-month-old male infant presented with jaundice and pale stools.
Exploratory laparotomy revealed a collapsed gallbladder, yellow bile, and patent right hepatic bile duct. The liver histopathology at the age of 2 months revealed cirrhosis with cholestasis jaundice. At the age of 7 months, repeated ultrasonography showed liver cirrhosis with evidence of portal hypertension, multiple cysts along the periportal distribution with a hyperechogenic area at the periportal region, probably a periportal type of Caroli disease, enlarged and diffusely increased parenchymal echogenicity of both kidneys, splenomegaly, and a moderate amount of ascites. The MRCP findings were diffuse cystic dilatation of bilateral intrahepatic bile ducts with the presence of a central dot sign at the peripheral zone and evidence of liver cirrhosis with portal hypertension. The patient underwent liver transplantation with a favorable outcome and a follow-up period of 10 years. A: Ultrasonography shows liver cirrhosis with multiple cysts along the periportal distribution, probably a periportal type of Caroli disease; B: Magnetic resonance cholangiopancreatography shows diffuse cystic dilatation of bilateral intrahepatic bile ducts; C: A 1.1 cm probable hepatic cyst at segment VI with a central dot sign.
- Citation: Eiamkulbutr S, Tubjareon C, Sanpavat A, Phewplung T, Srisan N, Sintusek P. Diseases of bile duct in children. World J Gastroenterol 2024; 30(9): 1043-1072
- URL: https://www.wjgnet.com/1007-9327/full/v30/i9/1043.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i9.1043