Copyright
©The Author(s) 2024.
World J Gastroenterol. Mar 14, 2024; 30(10): 1346-1357
Published online Mar 14, 2024. doi: 10.3748/wjg.v30.i10.1346
Published online Mar 14, 2024. doi: 10.3748/wjg.v30.i10.1346
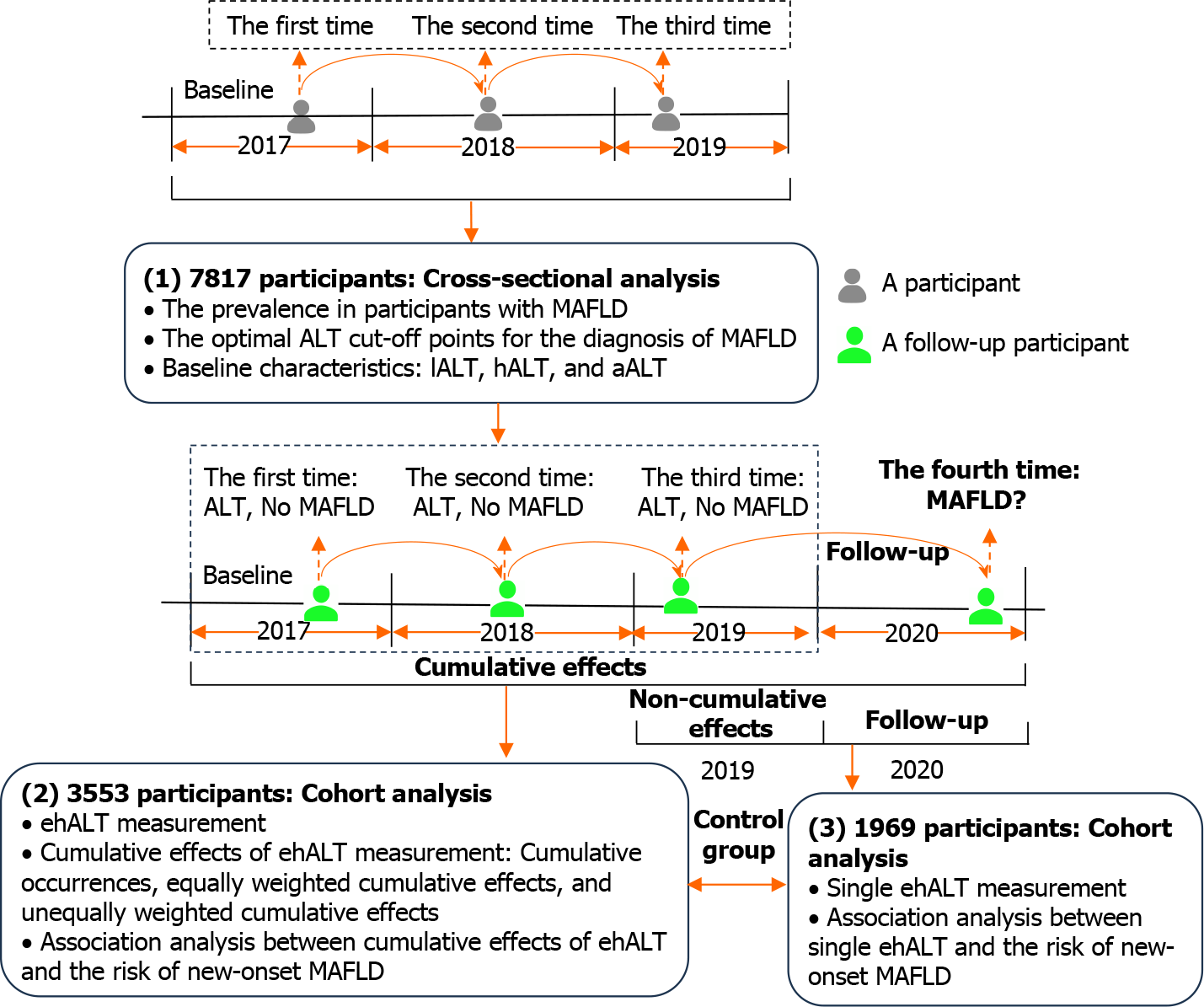
Figure 1 Schematic description of the study design.
7817 participants with three consecutive health examinations from 2017 to 2019 were analysed to determine the optimal alanine aminotransferase (ALT) cut-off points for the diagnosis of metabolic dysfunction-associated fatty liver disease (MAFLD). A follow-up cohort of 3553 participants who completed their fourth health examination in 2020 was subsequently analysed to calculate the cumulative effects of excess high-normal ALT and explore its association with the risk of new-onset MAFLD. ALT: Alanine aminotransferase; MAFLD: Metabolic dysfunction-associated fatty liver disease; lALT: Low-normal alanine aminotransferase; hALT: High-normal alanine aminotransferase; aALT: Abnormal alanine aminotransferase; ehALT: Excess high-normal alanine aminotransferase.
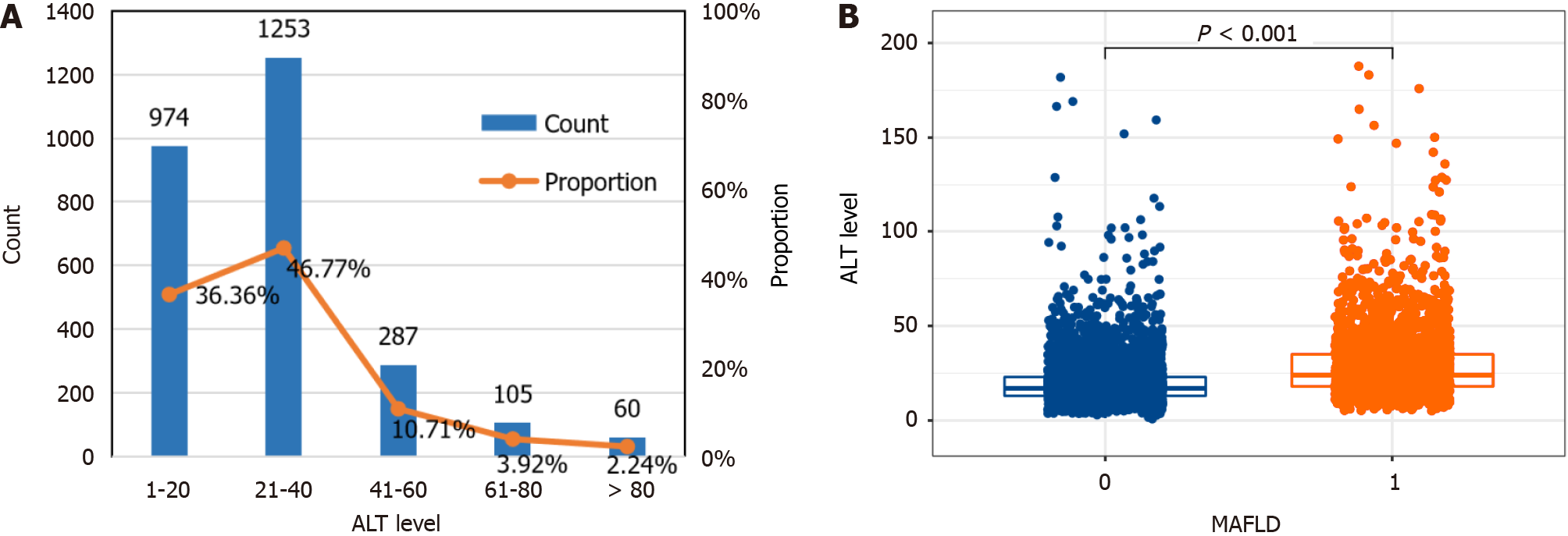
Figure 2 The prevalence of metabolic dysfunction-associated fatty liver disease in a large-scale, longitudinal population-based cohort.
A: Distribution of alanine aminotransferase (ALT) levels in participants with metabolic dysfunction-associated fatty liver disease (MAFLD); B: Differential analysis of ALT levels between healthy participants and those with MAFLD. The prevalence of MAFLD was 34.27%, and 83.13% of participants with MAFLD had normal ALT levels. ALT levels were significantly greater in MAFLD patients than in healthy individuals. ALT: Alanine aminotransferase; MAFLD: Metabolic dysfunction-associated fatty liver disease.
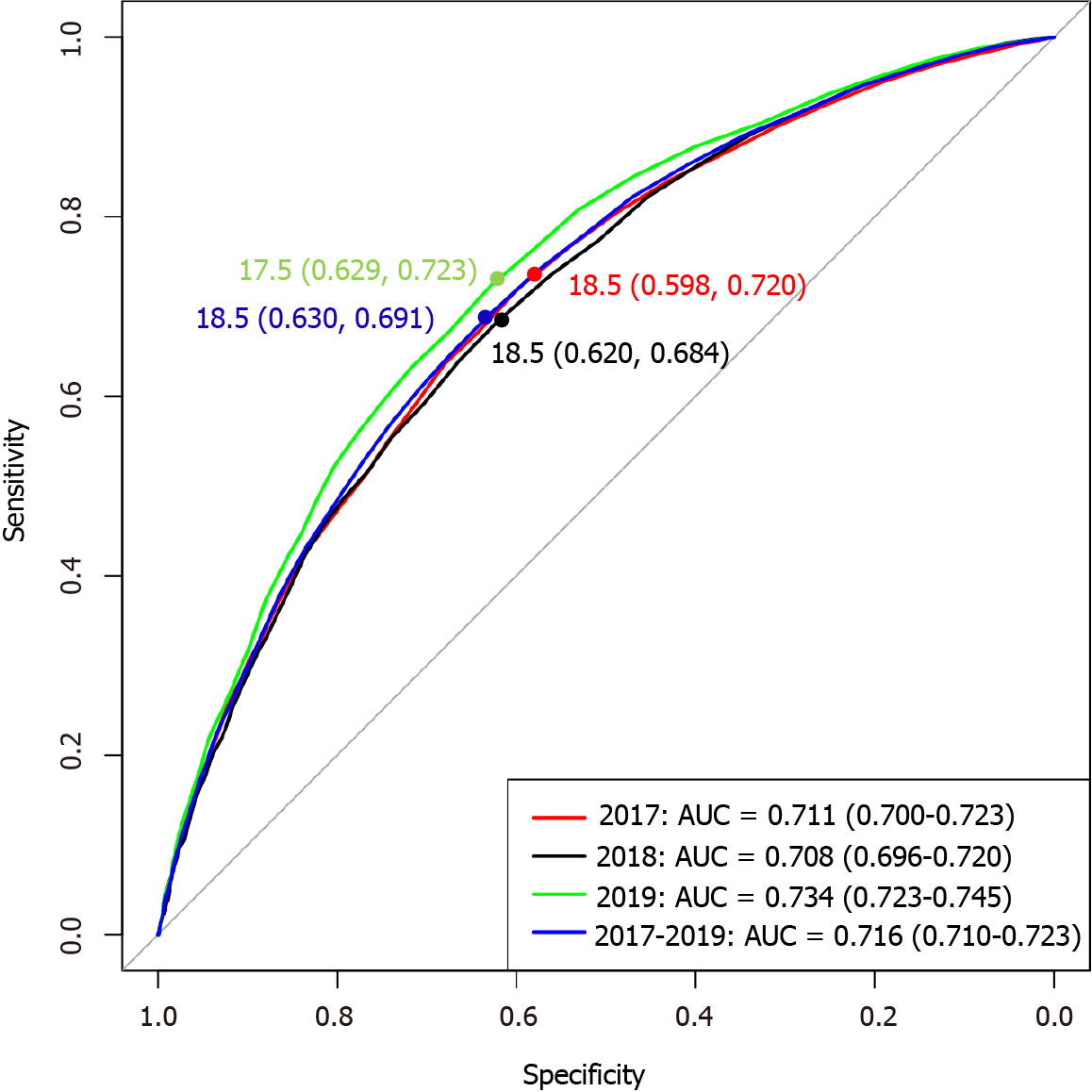
Figure 3 Optimal alanine aminotransferase cut-off points for the diagnosis of metabolic dysfunction-associated fatty liver disease.
The optimal alanine aminotransfer (ALT) cut-off point was 18.5 U/L based on receiver-operating characteristic curve and Youden index, and the cut-off point for high-normal ALT was 18.6-40 U/L. AUC: Area under the curve.
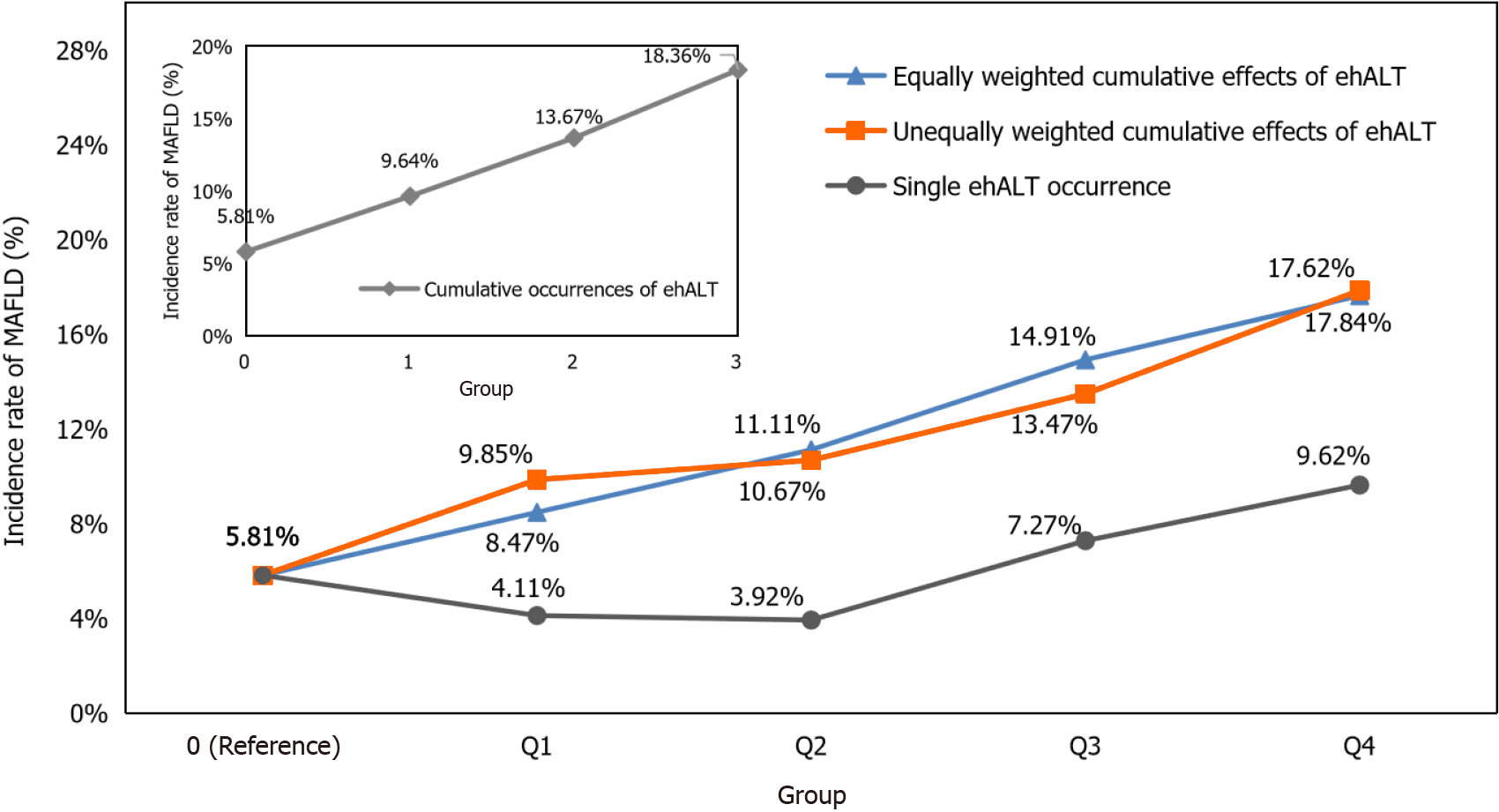
Figure 4 Incidence rate of metabolic dysfunction-associated fatty liver disease under the cumulative effects of excess high-normal alanine aminotransferase levels and a single excess high-normal alanine aminotransferase level occurrence in different groups.
The incidence rate of metabolic dysfunction-associated fatty liver disease showed a linear increasing trend in the cumulative excess high-normal alanine aminotransferase (ehALT) levels groups, while a single ehALT occurrence did not show a linear increasing trend in different groups. MAFLD: Metabolic dysfunction-associated fatty liver disease; ehALT: Excess high-normal alanine aminotransferase.
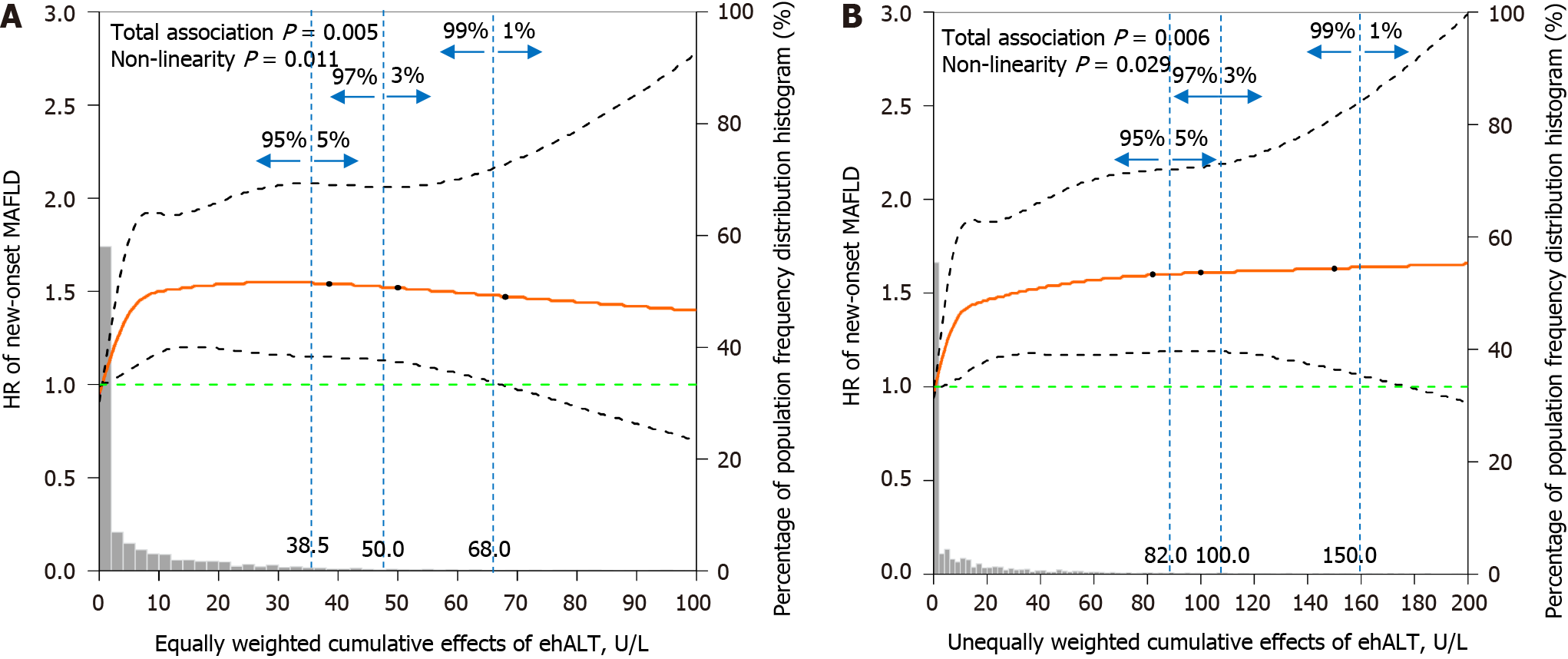
Figure 5 Dose-response relationship between the cumulative effects of excess high-normal alanine aminotransferase levels and the risk of new-onset metabolic dysfunction-associated fatty liver disease.
A: Equally weighted cumulative effects of excess high-normal alanine aminotransferase (ehALT) levels; B: Unequally weighted cumulative effects of ehALT. The equally and unequally weighted cumulative effects of ehALT had a positive nonlinear relationship with the risk of new-onset metabolic dysfunction-associated fatty liver disease in approximately 95% of the enrolled participants. Gray histogram: The probability distribution of the population corresponding to the accumulation of ehALT. Orange solid line: The restricted cubic splines [hazard ratios (HRs)]. Black dashed curves: The 95% confidence interval of the restricted cubic splines (HRs). Green dashed line: The reference line of the restricted cubic splines (HR = 1). Blue dashed lines: The dividing lines indicating population proportions of less than 5%, 3%, and 1%, respectively. MAFLD: Metabolic dysfunction-associated fatty liver disease; ehALT: Excess high-normal alanine aminotransferase; HR: Hazard ratio.
- Citation: Chen JF, Wu ZQ, Liu HS, Yan S, Wang YX, Xing M, Song XQ, Ding SY. Cumulative effects of excess high-normal alanine aminotransferase levels in relation to new-onset metabolic dysfunction-associated fatty liver disease in China. World J Gastroenterol 2024; 30(10): 1346-1357
- URL: https://www.wjgnet.com/1007-9327/full/v30/i10/1346.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i10.1346