Copyright
©The Author(s) 2023.
World J Gastroenterol. Aug 28, 2023; 29(32): 4851-4859
Published online Aug 28, 2023. doi: 10.3748/wjg.v29.i32.4851
Published online Aug 28, 2023. doi: 10.3748/wjg.v29.i32.4851
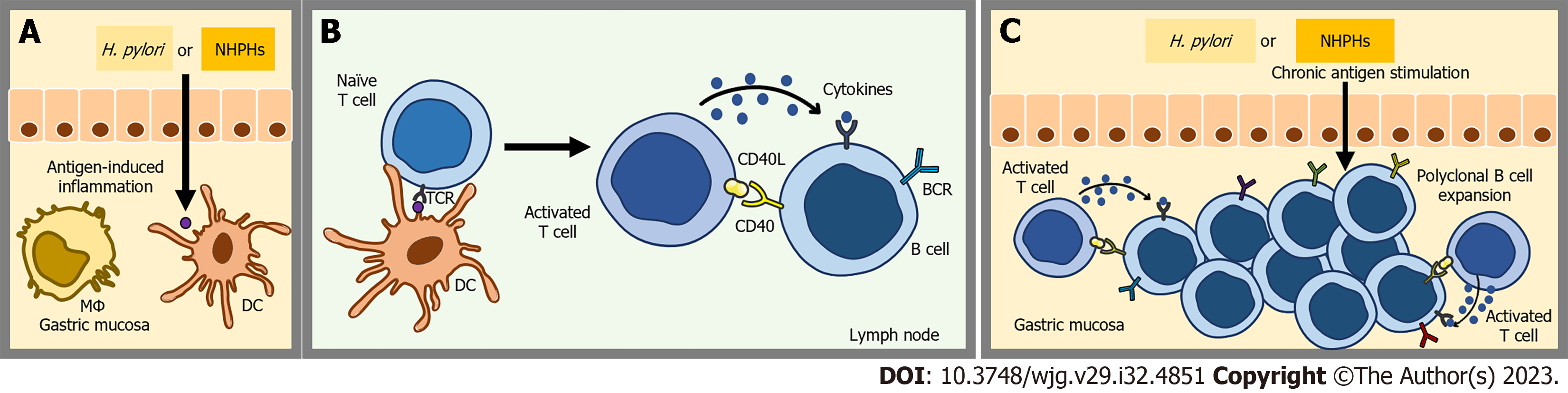
Figure 1 Antigen-induced acquisition of gastric mucosa-associated lymphoid tissue.
A: Antigen-induced inflammation; B: Clonal expansion of B cells supported by specific T helper cells; C: Acquisition of mucosa-associated lymphoid tissue (MALT). In the presence of chronic antigenic stimulation, gastric mucosal cells undergo activation and produce proinflammatory cytokines. These molecular mediators play a crucial role in initiating and perpetuating an immune response within the gastric tissue. As a consequence, lymphoid cells are recruited and infiltrate the gastric tissue. This cascade of events ultimately culminates in the development of MALT. H. pylori: Helicobacter pylori; NHPHs: Non-Helicobacter pylori gastric helicobacters; DC: Dendritic cell; MΦ: Macrophage; TCR: T cell receptor; CD40: Cluster of differentiation 40; CD40L: Cluster of differentiation 40 Ligand; BCR: B cell receptor.
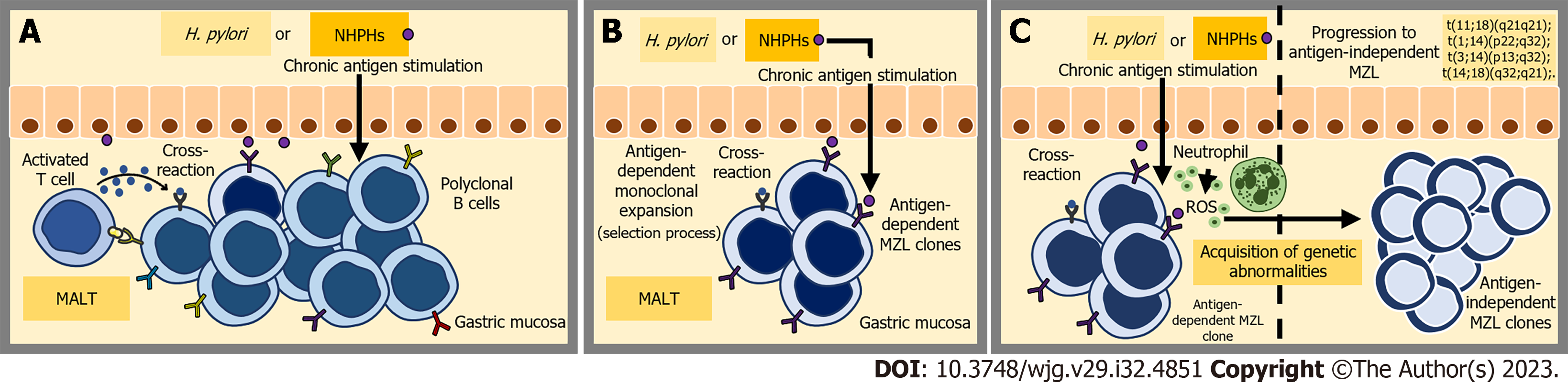
Figure 2 Simplified scheme of antigen-induced transformation of normal marginal-zone B-cells into malignant cells.
A: Polyclonal B cell expansion and a selection process; B: Antigen-dependent monoclonal expansion; C: Acquisition of genetic abnormalities and antigen-independent lymphomagenesis. The proliferation of B cells is primarily induced by the interaction between CD40 and CD40 Ligand, facilitated by antigen-activated reactive T cells. Additionally, cytokines play a role in driving this B-cell proliferation. The persistent proliferative state of these B cells, along with chronic inflammation, triggers additional oncogenic events. Ultimately, these events lead to the development of antigen-independent lymphoproliferation. NHPHs: Non-Helicobacter pylori gastric helicobacters; ROS: Reactive oxygen species; MZL: Marginal zone lymphoma; MALT: Mucosa-associated lymphoid tissue; H. pylori: Helicobacter pylori.
- Citation: Lemos FFB, Silva Luz M, Rocha Pinheiro SL, Teixeira KN, Freire de Melo F. Role of non-Helicobacter pylori gastric Helicobacters in helicobacter pylori-negative gastric mucosa-associated lymphoid tissue lymphoma. World J Gastroenterol 2023; 29(32): 4851-4859
- URL: https://www.wjgnet.com/1007-9327/full/v29/i32/4851.htm
- DOI: https://dx.doi.org/10.3748/wjg.v29.i32.4851