Copyright
©The Author(s) 2023.
World J Gastroenterol. Jul 7, 2023; 29(25): 4072-4084
Published online Jul 7, 2023. doi: 10.3748/wjg.v29.i25.4072
Published online Jul 7, 2023. doi: 10.3748/wjg.v29.i25.4072
Figure 1 Area under the curve of various models in predicting high-risk esophageal varices of patients.
A: Modelling group; B: External validation group. The area under the curve of the new model in predicting high-risk esophageal varices of patients was 0.965 in the modelling group, which was higher than that of liver stiffness-spleen diameter to platelet ratio score, variceal risk index, aspartate aminotransferase/alanine aminotransferase ratio and Baveno VI; and it was 1 in the external validation group. LSPS: Liver stiffness-spleen diameter to platelet ratio score; VRI: Variceal risk index; AAR: Aspartate aminotransferase/alanine aminotransferase ratio.
Figure 2 Calibration scatter plot of data of patients.
A: Modelling group; B: External validation group. In predicting patients in the modelling group and external validation group, the scattered points fluctuated around the reference line without significant deviations.
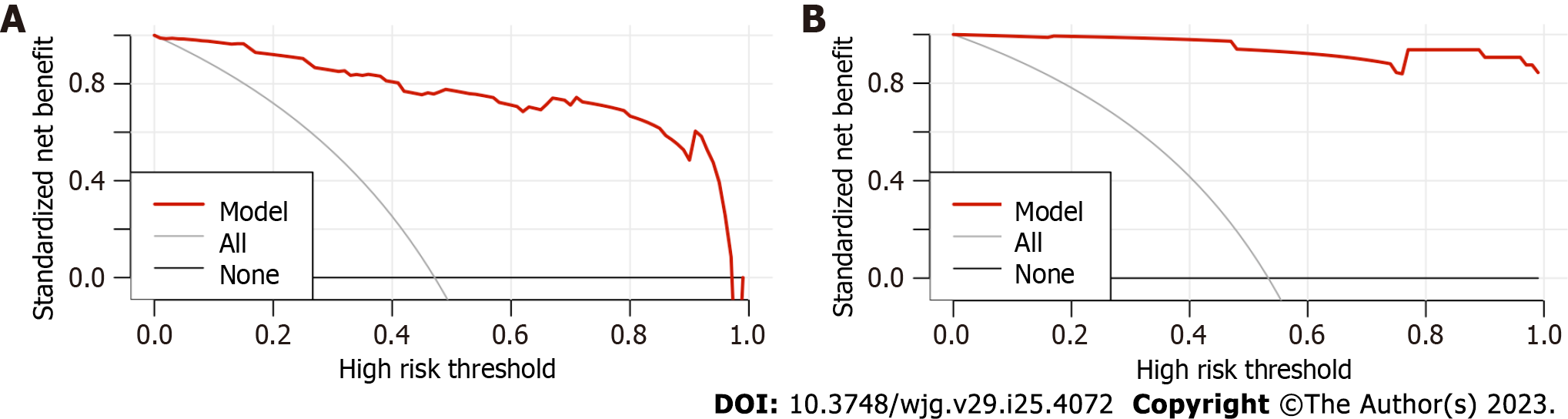
Figure 3 Adjusted decision curve analysis of data of patients.
A: Modelling group; B: External validation group. The black line indicates that in extreme cases, the new model predicted that there were no high-risk esophageal varices in all patients with viral cirrhosis, and the clinical net benefit was 0. The gray curve indicates that in extreme cases, the new model predicts there are high-risk esophageal varices in all patients with viral cirrhosis, the clinical net benefit is the negative slope. The red line indicates that the new model has a clinical net benefit. The red line is higher than the black and gray lines, indicating that patients in the modelling group can benefit from the new model.
- Citation: Yang LB, Gao X, Li H, Tantai XX, Chen FR, Dong L, Dang XS, Wei ZC, Liu CY, Wang Y. Non-invasive model for predicting high-risk esophageal varices based on liver and spleen stiffness. World J Gastroenterol 2023; 29(25): 4072-4084
- URL: https://www.wjgnet.com/1007-9327/full/v29/i25/4072.htm
- DOI: https://dx.doi.org/10.3748/wjg.v29.i25.4072