Copyright
©The Author(s) 2023.
World J Gastroenterol. Jan 7, 2023; 29(1): 126-143
Published online Jan 7, 2023. doi: 10.3748/wjg.v29.i1.126
Published online Jan 7, 2023. doi: 10.3748/wjg.v29.i1.126
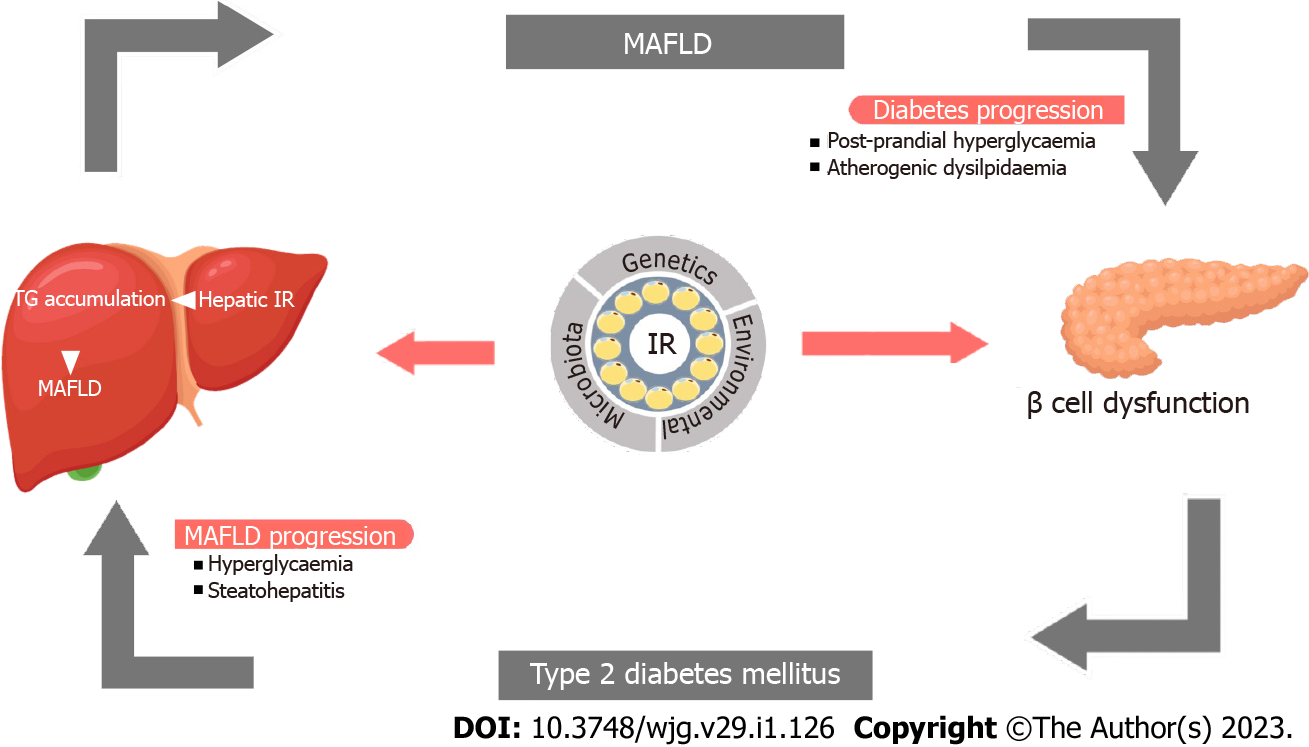
Figure 1 Pathobiological link between metabolic-associated fatty live disease and type 2 diabetes mellitus.
Metabolic-associated fatty live disease (MAFLD) may increase the risk for hyperglycemia and dyslipidemia and cause β-cell dysfunction leading to insulin resistance and type 2 diabetes which in turn may aggravate MAFLD progression to nonalcoholic steatohepatitis and fibrosis. IR: Insulin resistance; MAFLD: Metabolic-associated fatty live disease; TG: Triglycerides.
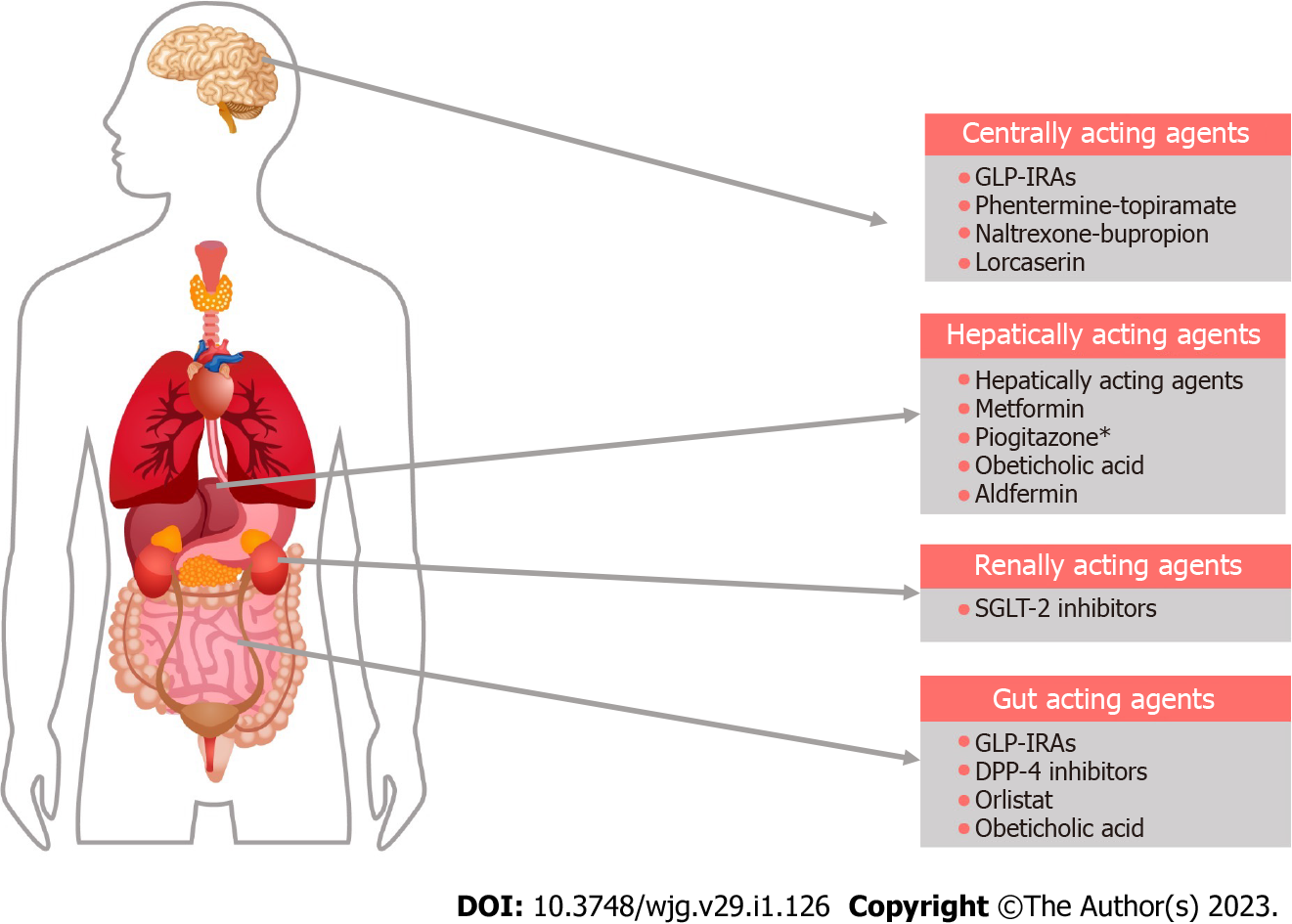
Figure 2 Major sites of action of drugs currently used in the treatment of metabolic-associated fatty live disease.
Various medications targeting comorbidities that coexist with metabolic-associated fatty live disease are used to treat symptomatic patients. The asterisk indicates adipocyte action is not shown. GLP-1RA: Glucagon-like insulinotropic peptide-1 receptor agonist; SGLT-2: Sodium glucose cotransporter-2.
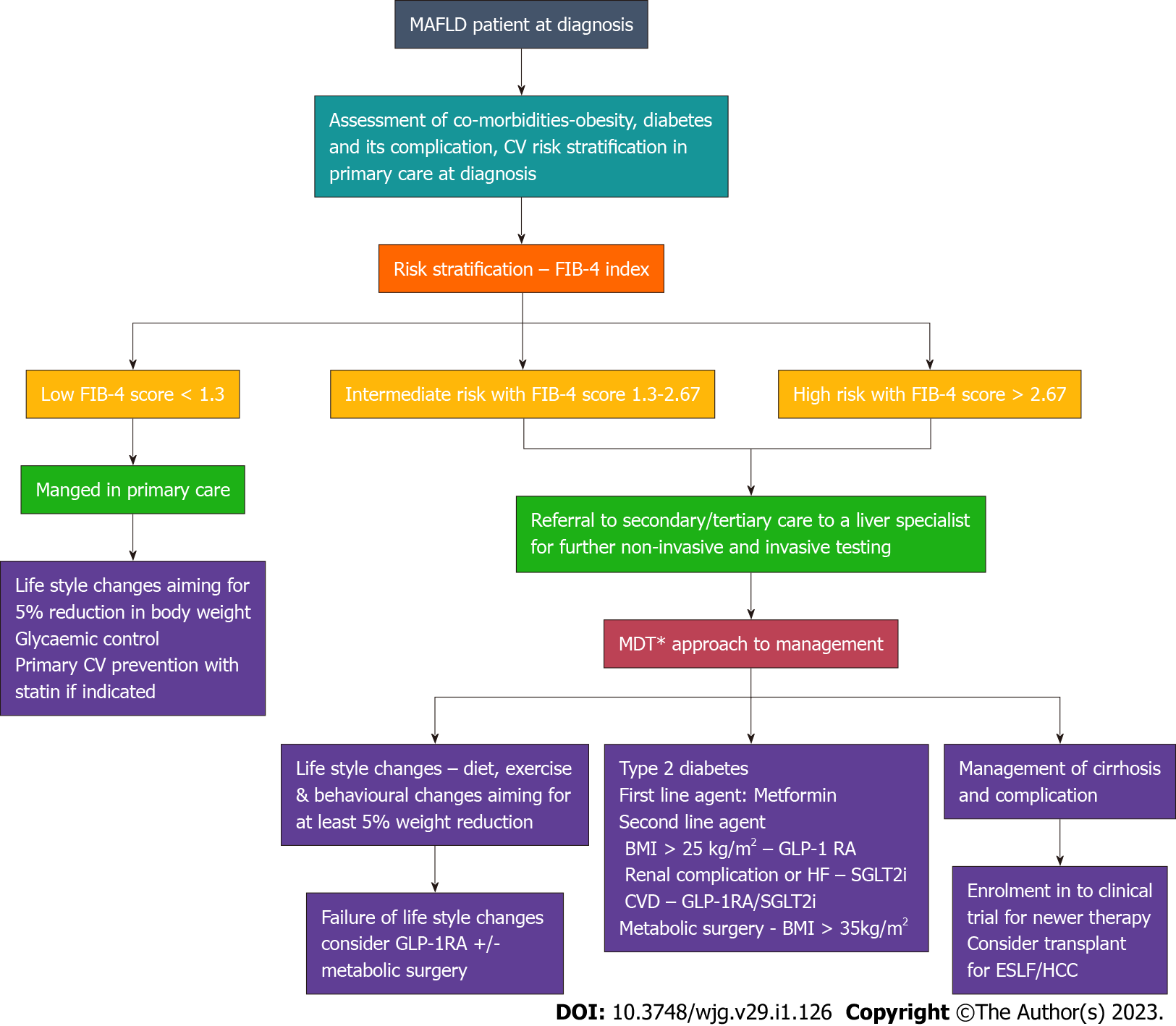
Figure 3 Management and referral system pathway for patient with metabolic associated fatty liver disease.
Multidisciplinary treatment approach involving dietician, physiotherapist, psychologist, diabetologist and hepatologist. In resource constrained setting, referral to individual specialist based on the predominant effect due to metabolic-associated fatty live disease as per the pathway. GLP-1RA: Glucagon-like insulinotropic peptide-1 receptor agonist; SGLT-2i: Sodium glucose cotransporter-2 inhibitors; CVD: Cardiovascular disease; HF: Heart failure; BMI: Body mass index.
- Citation: Jeeyavudeen MS, Khan SKA, Fouda S, Pappachan JM. Management of metabolic-associated fatty liver disease: The diabetology perspective. World J Gastroenterol 2023; 29(1): 126-143
- URL: https://www.wjgnet.com/1007-9327/full/v29/i1/126.htm
- DOI: https://dx.doi.org/10.3748/wjg.v29.i1.126