Copyright
©The Author(s) 2022.
World J Gastroenterol. Aug 14, 2022; 28(30): 4163-4173
Published online Aug 14, 2022. doi: 10.3748/wjg.v28.i30.4163
Published online Aug 14, 2022. doi: 10.3748/wjg.v28.i30.4163
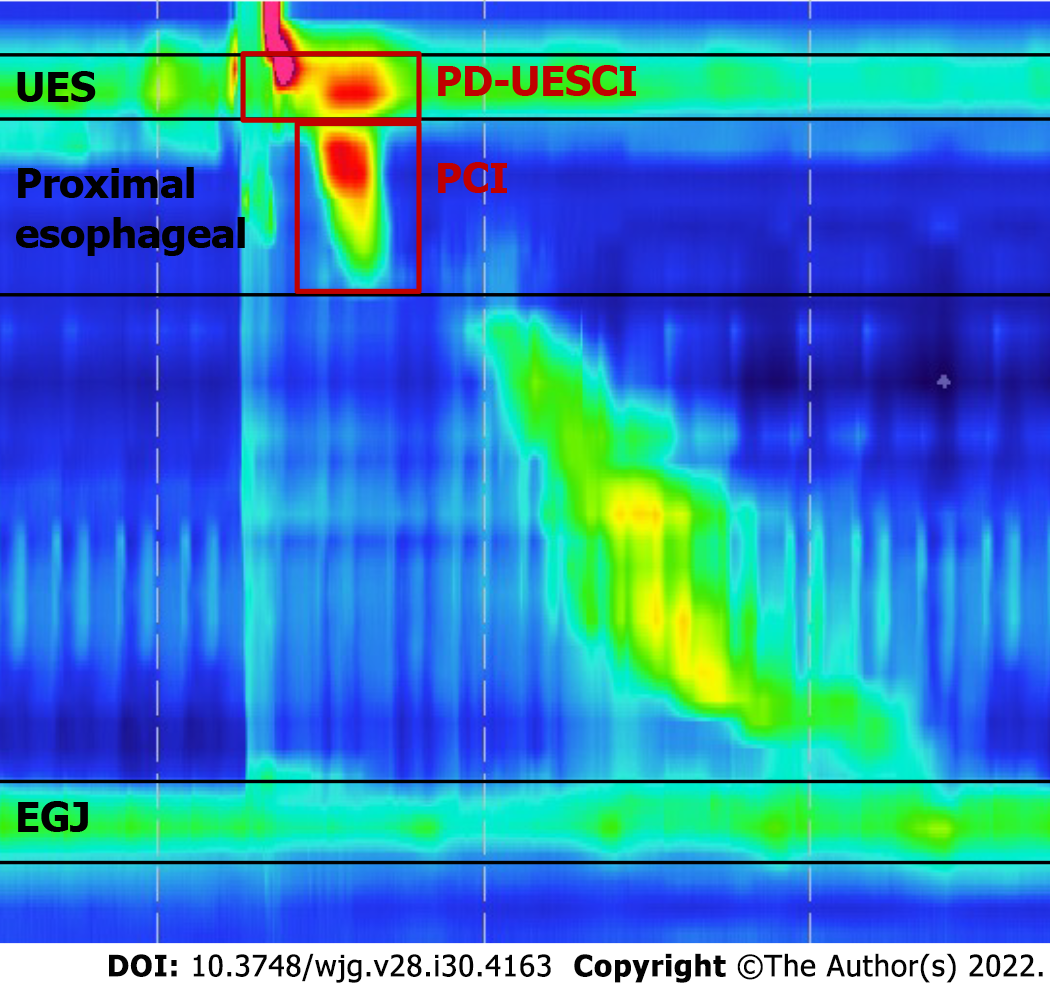
Figure 1 Key metrics of Clouse plots used in our study.
The postdeglutitive upper esophageal sphincter (UES) contractile integral was measured using a 20-mmHg pressure threshold from the beginning of the deglutitive UES relaxation to the end of the proximal esophageal contraction or the beginning of the transition zone. The proximal esophageal contractile integral was measured using a 20-mmHg pressure threshold from the lower border of the UES to either a break between the proximal and distal segment or the area with the lowest pressure between the proximal and distal segment of the contraction in patients showed no break in the 20-mmHg isobaric contour. UES: Upper esophageal sphincter; PD-UESCI: Postdeglutitive upper esophageal sphincter contractile integral; PCI: Proximal contractile integral; EGJ: Esophagogastric junction.
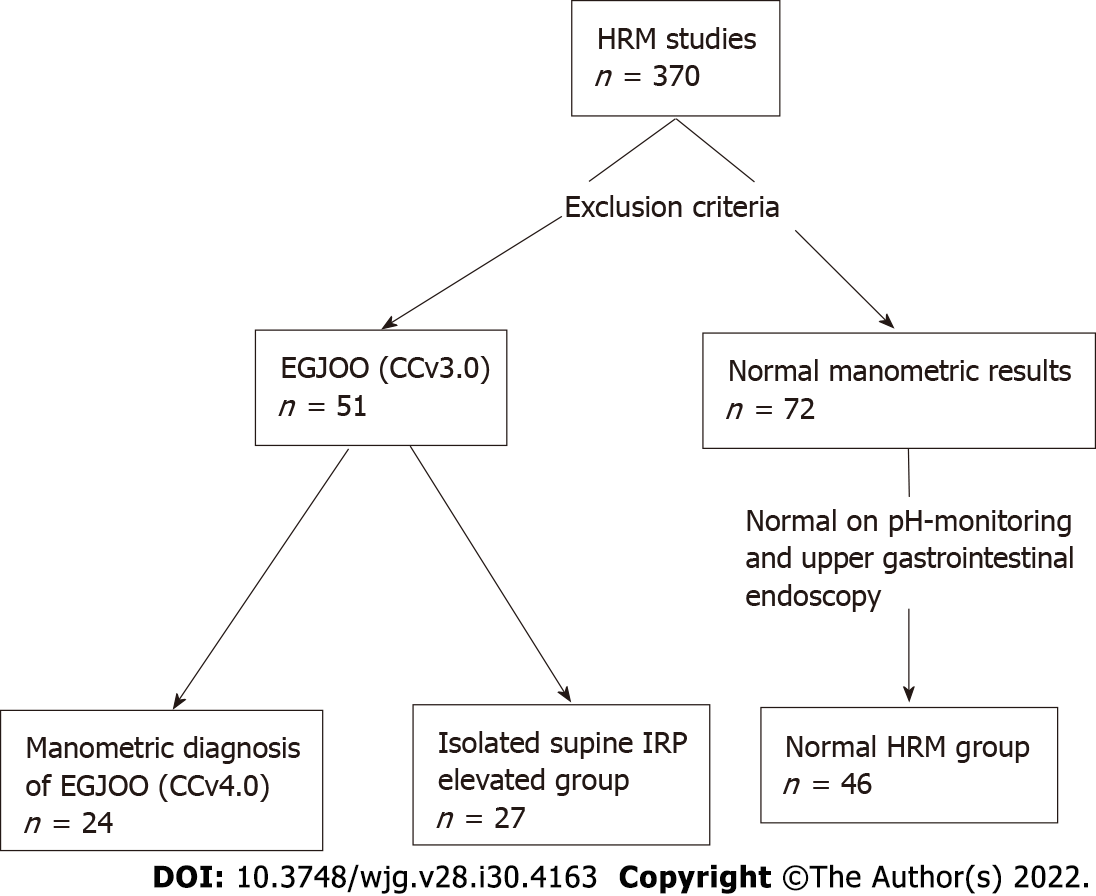
Figure 2 Patient flow.
HRM: High-resolution manometry; EGJOO: Esophagogastric junction outflow obstruction; CCv3.0: Chicago Classification version 3.0; CCv4.0: Chicago Classification version 4.0; IRP: Integrated relaxation pressure.
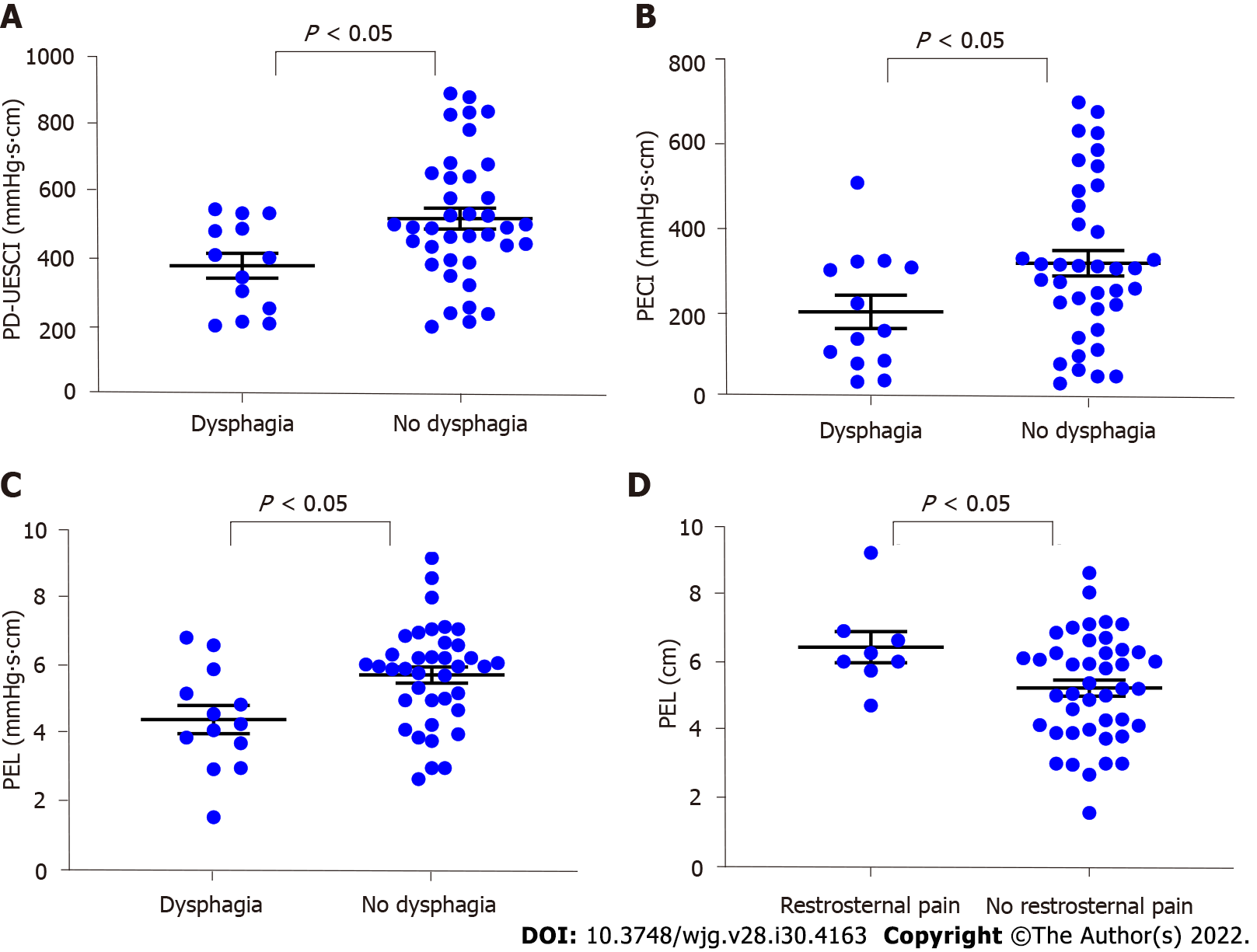
Figure 3 Comparisons of parameters according to symptoms in 51 patients with elevated integrated relaxation pressure.
A: Patients with dysphagia showed lower postdeglutitive upper esophageal sphincter contractile integral than patients without dysphagia; B: Patients with dysphagia showed lower proximal esophageal contractile integral than patients without dysphagia; C: Patients with dysphagia showed lower proximal esophageal length (PEL) than patients without dysphagia; D: Patients with retrosternal pain showed higher PEL than patients without retrosternal pain. PD-UESCI: Postdeglutitive upper esophageal sphincter contractile integral; PECI: Proximal esophageal contractile integral; PEL: Proximal esophageal length.
- Citation: Li YY, Lu WT, Liu JX, Wu LH, Chen M, Jiao HM. Changes in the esophagogastric junction outflow obstruction manometric feature based on the Chicago Classification updates. World J Gastroenterol 2022; 28(30): 4163-4173
- URL: https://www.wjgnet.com/1007-9327/full/v28/i30/4163.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i30.4163