Copyright
©The Author(s) 2019.
World J Gastroenterol. Jun 14, 2019; 25(22): 2706-2719
Published online Jun 14, 2019. doi: 10.3748/wjg.v25.i22.2706
Published online Jun 14, 2019. doi: 10.3748/wjg.v25.i22.2706
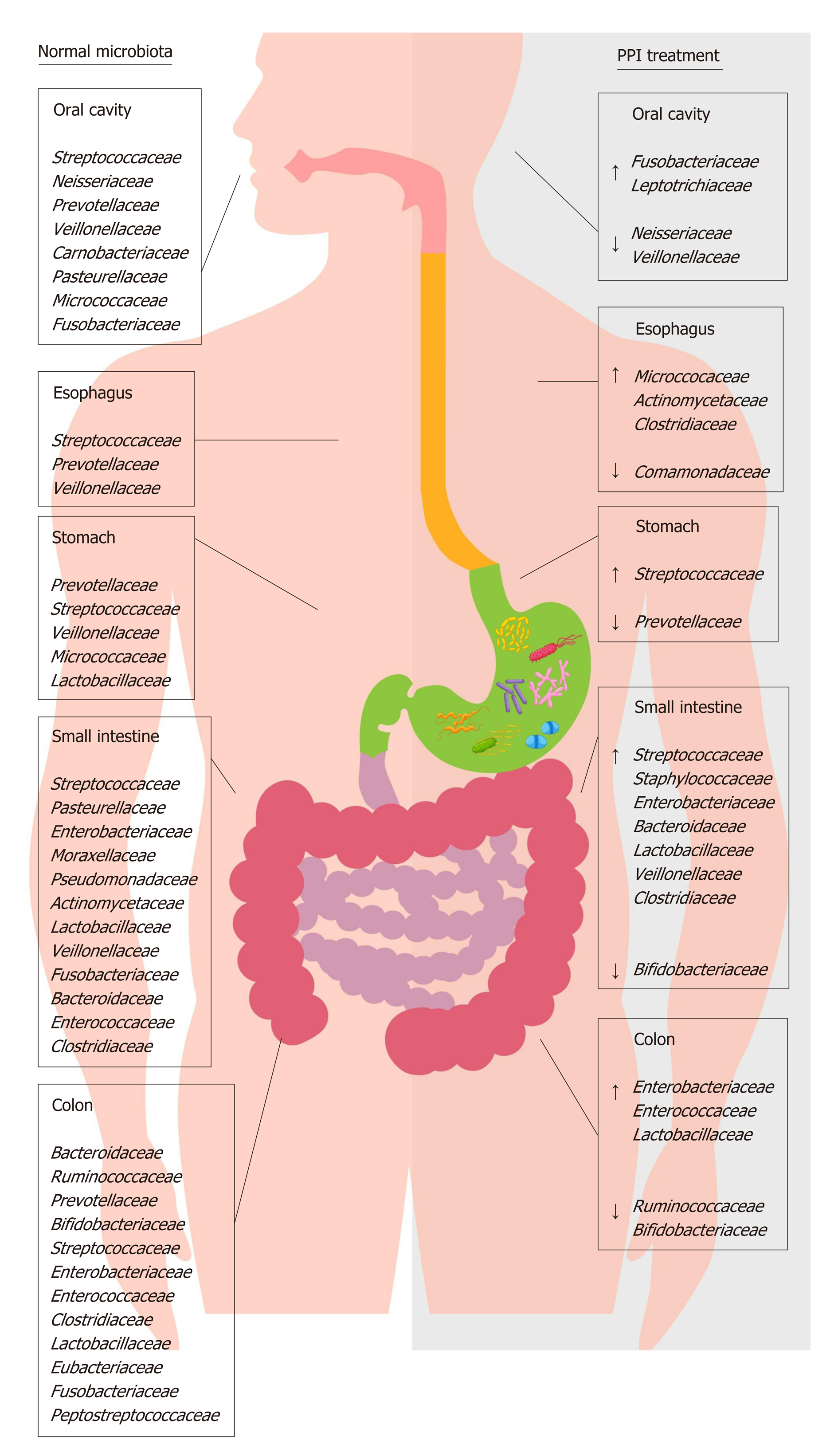
Figure 1 Distribution of main bacterial families of human microbiota in physiological condition and during proton pump inhibitor treatment.
This figure shows the effect of proton pump inhibitor (PPI) treatment on the composition of gut microbiota families. The left side of the figure shows the principal bacterial families under normal physiological conditions; the right side of the figure shows the increase (↑) and decrease (↓) in bacterial families present in the gut microbiota during PPI treatment. PPI: Proton pump inhibitor.
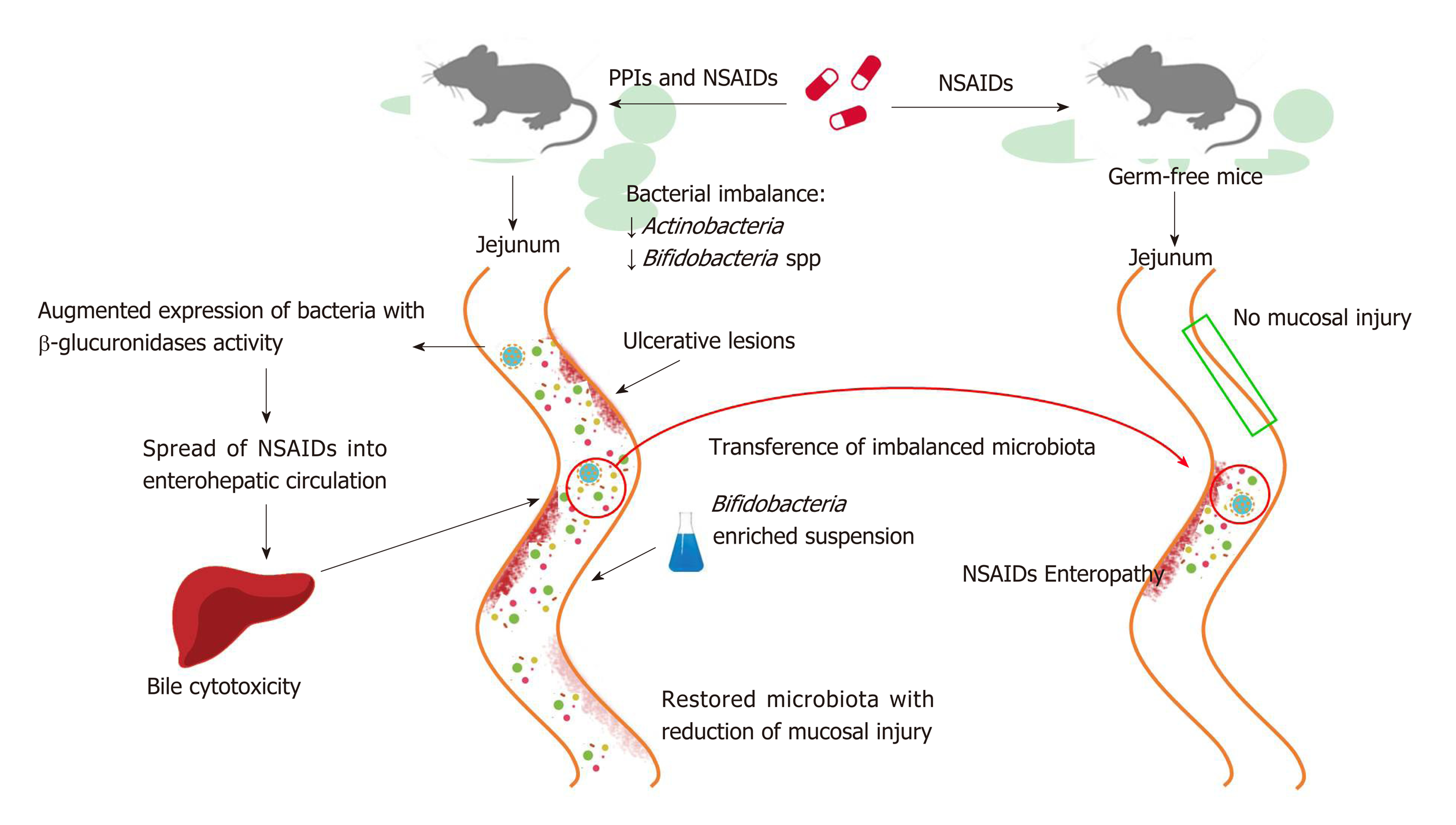
Figure 2 Proton pump inhibitors promote non-steroidal anti-inflammatory drug-induced enteropathy via microbiota.
Murine models demonstrate that proton pump inhibitor (PPI) treatment, in addition to non-steroidal anti-inflammatory drugs (NSAIDs) therapy, brings about an exacerbation of mucosal damage in the small intestine. PPIs cause a bacterial imbalance, such as the reduction (↓) of Actinobacteria and Bifidobacteria spp., which is responsible for the mucosal damage. Specifically, PPIs increase the expression of bacteria with beta-glucuronidases activity and the consequent spreading of NSAIDs into enterohepatic circulation; ultimately, bile cytotoxicity then causes ulcerative intestinal lesions. The co-administration of Bifidobacteria-enriched suspension restores the gut microbiota and reduces mucosal damage. Germ-free mice are less susceptible to NSAIDs’ harmful effects and they develop NSAID-induced enteropathy through microbiota transfer. PPI: Proton pump inhibitor; NSAID: Non-steroidal anti-inflammatory drugs.
- Citation: Bruno G, Zaccari P, Rocco G, Scalese G, Panetta C, Porowska B, Pontone S, Severi C. Proton pump inhibitors and dysbiosis: Current knowledge and aspects to be clarified. World J Gastroenterol 2019; 25(22): 2706-2719
- URL: https://www.wjgnet.com/1007-9327/full/v25/i22/2706.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i22.2706