Copyright
©The Author(s) 2015.
World J Gastroenterol. Mar 7, 2015; 21(9): 2683-2692
Published online Mar 7, 2015. doi: 10.3748/wjg.v21.i9.2683
Published online Mar 7, 2015. doi: 10.3748/wjg.v21.i9.2683
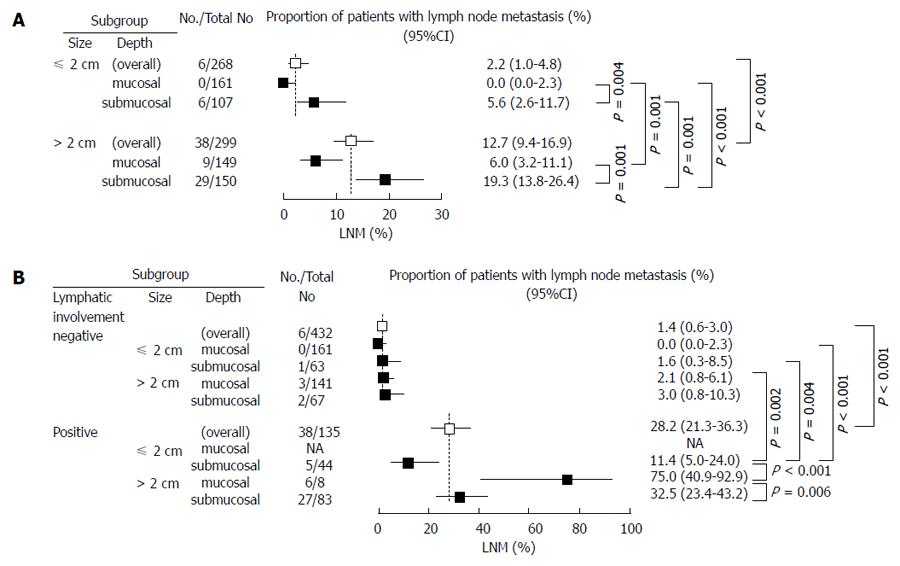
Figure 1 Lymph node metastasis.
A: In each subgroup of undifferentiated-type gastric adenocarcinoma. The figure demonstrates incidence of lymph node metastasis (LNM) with 95%CIs in subgroups classified by gastroscopic findings (size and depth) of undifferentiated-type gastric adenocarcinoma. The dashed lines represent incidence of LNM (%) in cases ≤ 2 cm and > 2 cm. A P value with a significant difference between two groups is shown. LNM was absent in the mucosal ≤ 2 cm group. The LNM rate was significantly higher in the > 2 cm group than in the > 2 cm group and higher in submucosal cancer than in mucosal cancer; B: In each subgroup with and without lymphatic involvement (LI) of undifferentiated-type gastric adenocarcinoma. The figure demonstrates incidence of LNM with its 95%CI in subgroups classified by size, depth, and LI in undifferentiated-type gastric adenocarcinoma. The dashed lines represent incidence of LNM (%) with or without LI. There was no case with LI-positive, ≤ 2 cm, and mucosal, which was referred to as not applicable (NA). A P value with a significant difference between two groups is shown. There was no significant difference in the LNM rate among LI-negative groups. The LNM rate was significantly lower in the LI-negative group than in the LI-positive group. The LNM rate (LI-positive, ≤ 2 cm, and submucosal) was relatively low at 11.4%.
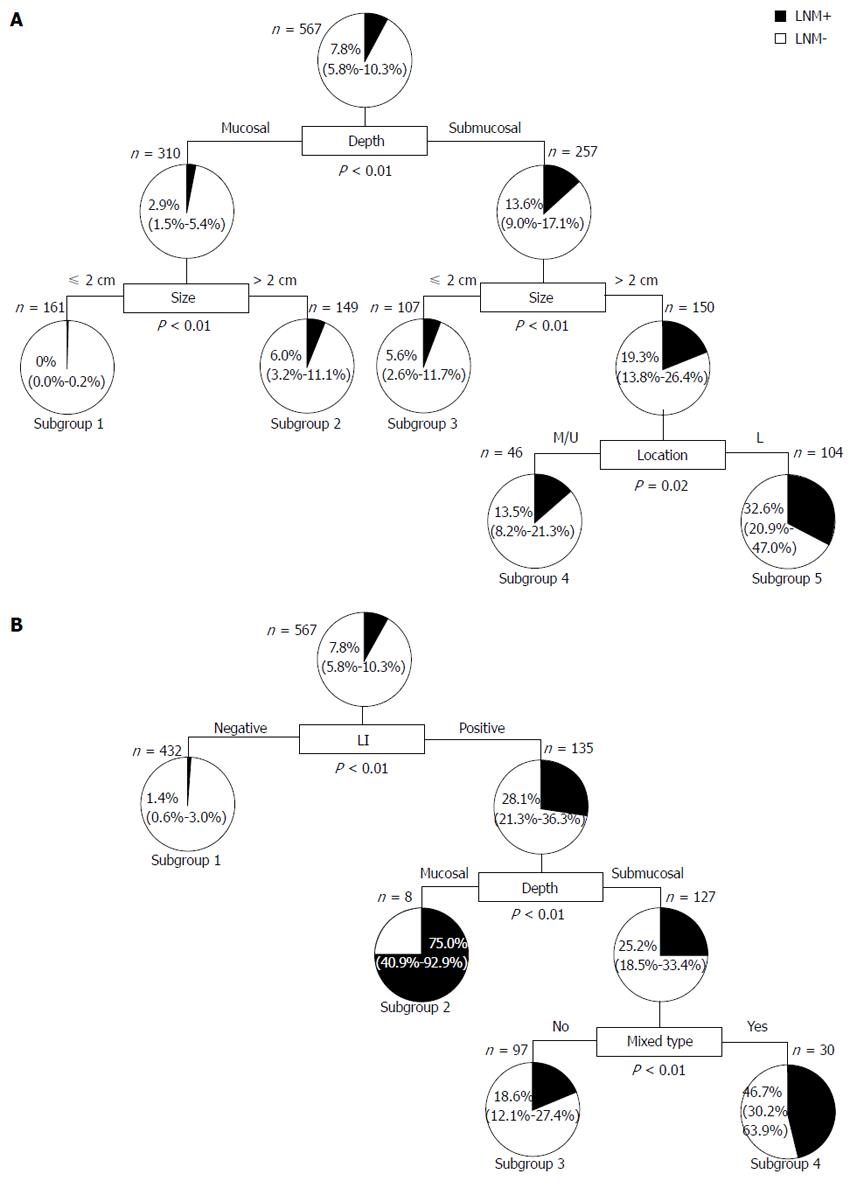
Figure 2 Decision tree analysis.
A: Preoperatively evaluable factors. Based on nine factors of age, gender, location, size, form, ulcer, depth, histology, and mixed-type, 567 cases were classified into five subgroups. Boxes indicate the factors used for splitting with cut-off points. Pie charts indicate the rate of lymph node metastasis in each group. Numbers show the rate of lymph node metastasis with 95%CI; B: Postoperatively evaluable factors. Based on 11 factors of age, gender, location, size, form, ulcer, depth, histology, mixed-type, lymphatic involvement, venous involvement, and lymph node metastasis, 567 cases were classified into four subgroups on the decision tree. Boxes indicate the factors used for splitting with cut-off points. Pie charts indicate the rate of lymph node metastasis in each group. Numbers shows the rate of lymph node metastasis with 95%CI. LNM: Lymph node metastasis; M/U: Middle/upper third of the stomach; L: Lower third of the stomach; LI: Lymphatic involvement.
- Citation: Asakawa Y, Ohtaka M, Maekawa S, Fukasawa M, Nakayama Y, Yamaguchi T, Inoue T, Uetake T, Sakamoto M, Sato T, Kawaguchi Y, Fujii H, Mochizuki K, Hada M, Oyama T, Yasumura T, Omata K, Nishiyama A, Naito K, Hata H, Haba Y, Miyata K, Saitoh H, Yamadera Y, Miura K, Kawaoi A, Abe T, Tsunoda H, Honda Y, Kurosaki M, Enomoto N. Stratifying the risk of lymph node metastasis in undifferentiated-type early gastric cancer. World J Gastroenterol 2015; 21(9): 2683-2692
- URL: https://www.wjgnet.com/1007-9327/full/v21/i9/2683.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i9.2683