Copyright
©The Author(s) 2015.
World J Gastroenterol. Jan 28, 2015; 21(4): 1334-1343
Published online Jan 28, 2015. doi: 10.3748/wjg.v21.i4.1334
Published online Jan 28, 2015. doi: 10.3748/wjg.v21.i4.1334
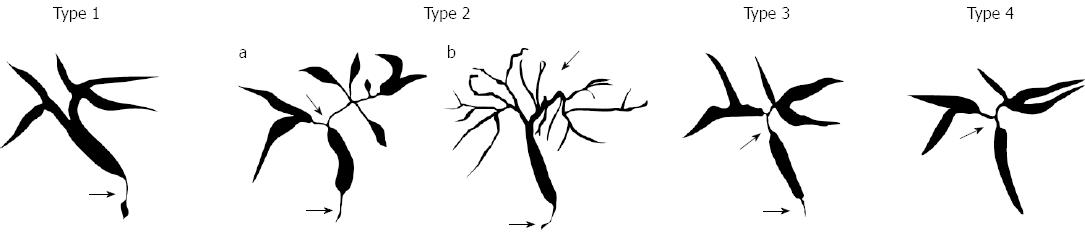
Figure 1 Cholangiographic classification of IgG4-related sclerosing cholangitis.
Stenosis is located only in the lower part of the common bile duct in Type 1; stenosis is diffusely distributed in the intra-and extra-hepatic bile ducts in Type 2. Type 2 is further subdivided into 2 types. Extended narrowing of the intrahepatic bile ducts with prestenotic dilation is widely distributed in Type 2a. Narrowing of the intrahepatic bile ducts without prestenotic dilation and reduced bile duct branches are widely distributed in Type 2b; stenosis is detected in both the hilar hepatic lesions and the lower part of the common bile ducts in Type 3; strictures of the bile duct are detected only in the hilar hepatic lesions in Type 4.
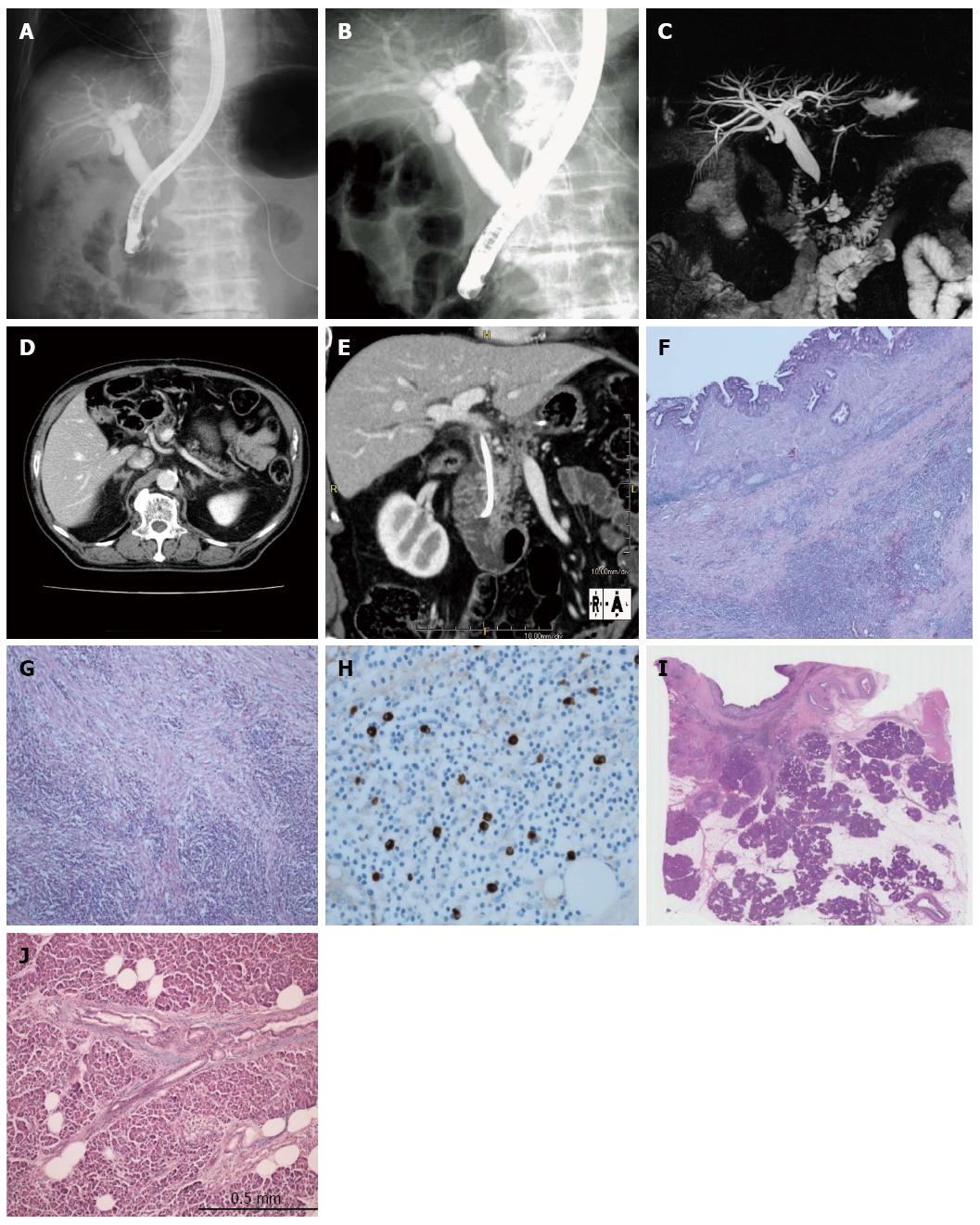
Figure 2 Imaging and pathological findings of Case 1.
A: Stenosis of the intrapancreatic bile duct on endoscopic retrograde cholangiopancreatography (ERCP); B, C: No irregular narrowing of the main pancreatic duct on ERCP and magnetic resonance cholangiopancreatography; D: No enlargement of the pancreas on computed tomography (CT); E: Thickening of the extrahepatic bile duct wall on CT (arrowhead); F: Bile duct wall thicking in surgical specimen of bile duct wall (HE × 40); G: Abundant infiltration of lymphocytes and plasma cells in the bile duct wall (HE × 200); H: Abundant infiltration of IgG4-positive plasma cells in the bile duct wall (IgG4 staining × 800); I, J: No findings mimicking AIP in surgical specimen of adjacent pancreatic tissue (I: HE × 2), (J: HE × 400).
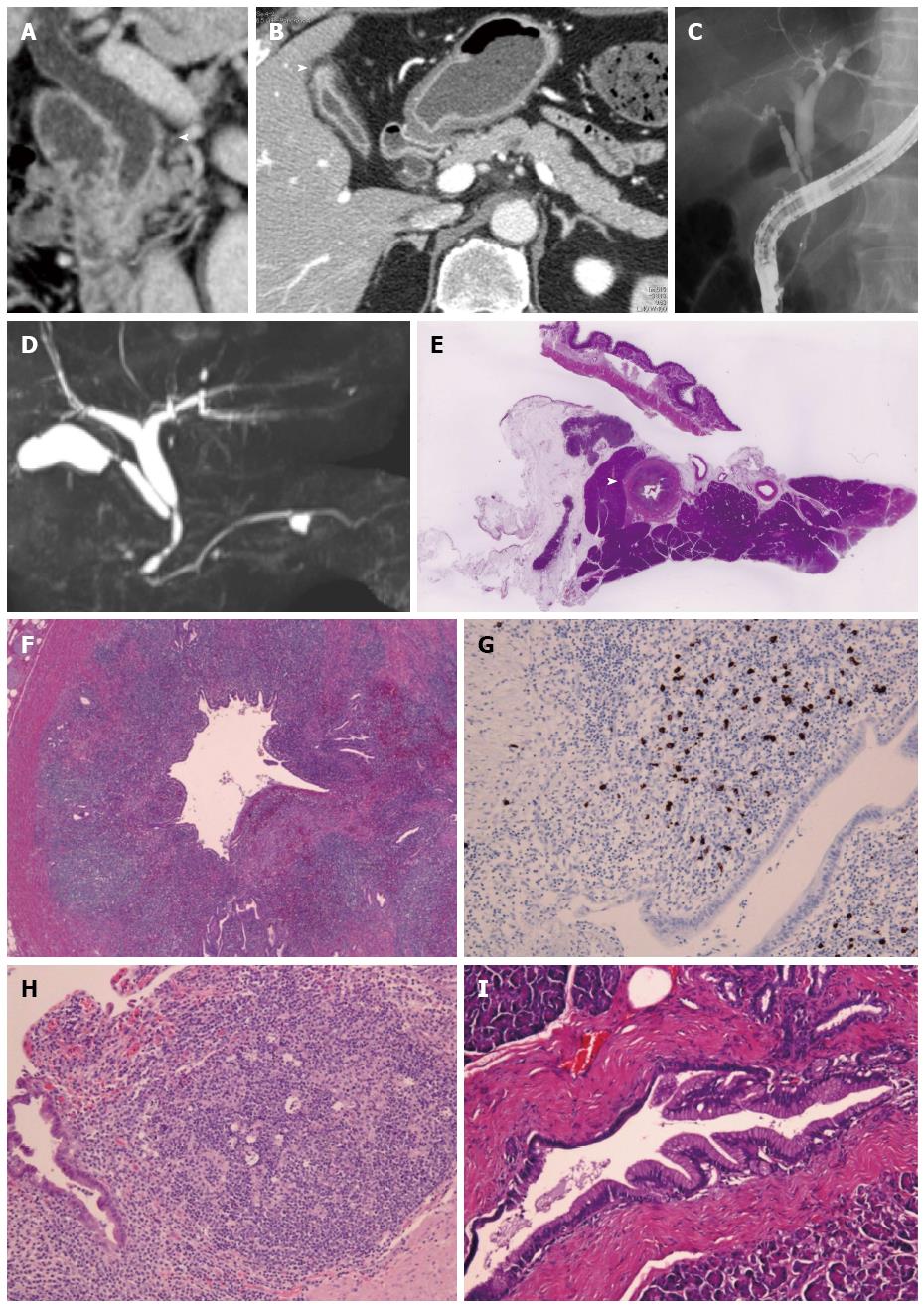
Figure 3 Imaging and pathological findings of Case 2.
A: Long segmental wall thickness in the middle and lower extrahepatic bile duct on abdominal computed tomography (arrowhead); B: Wall thickness of the fundus of gall bladder (arrowhead) and normal size of the pancreas; C: Long segmental stenosis in the middel and lower extrahepatic bile duct on endoscopic retrograde cholangiography; D: Normal main pancreatic duct except a pancreatic cyst on magnetic resonance cholangiopancreatography; E: Bile duct wall thicking (arrow head) and no inflammation of pancreas tissue in surgical specimen (HE × 1); F: Abundant infiltration of lymphocytes and plasma cells in the bile duct wall (HE × 200); G: Abundant infiltration of IgG4-positive plasma cells in the bile duct wall (IgG4 staining × 400); H: Numerous lymphocytes and plasma cells in the wall of gall bladder (HE × 400); I: Normal pancreatic tissue in adjacent pancreas (HE × 400).
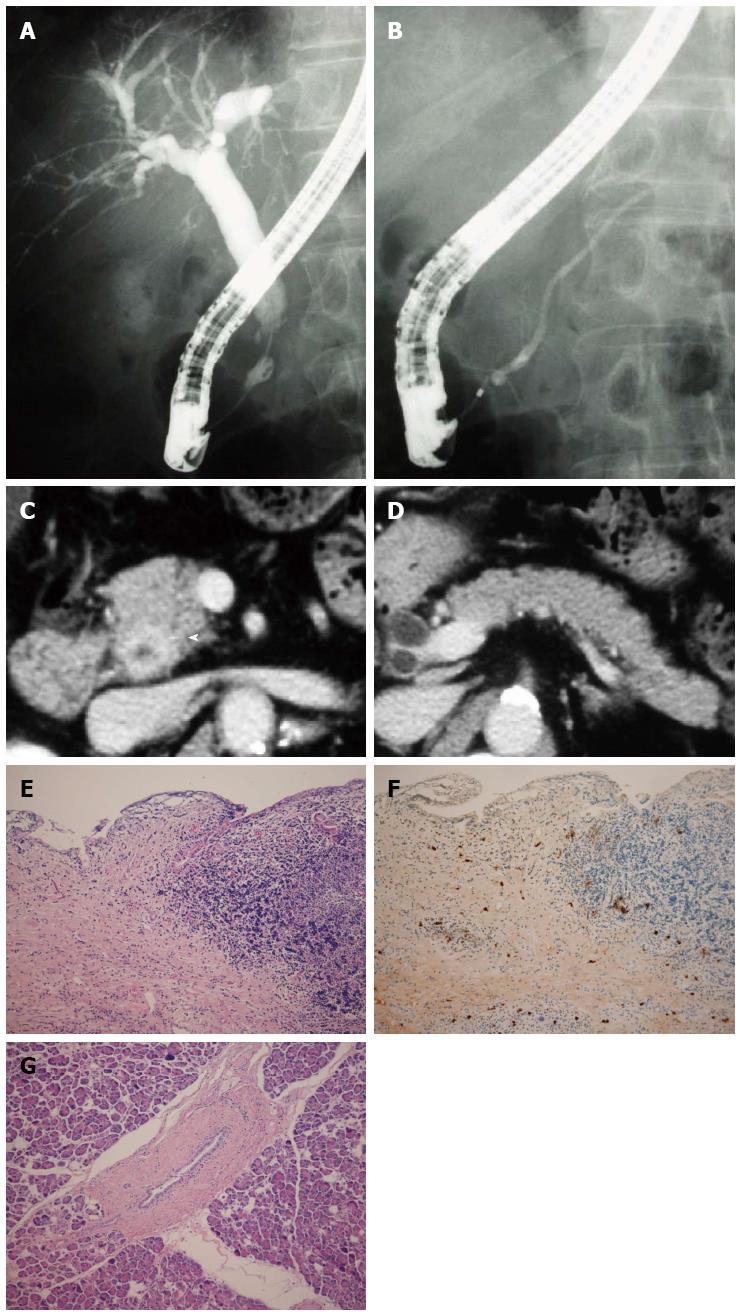
Figure 4 Imaging and pathological findings of Case 3.
A: Stricture in the intrapancreatic duct on endoscopic retrograde cholangiography; B: Normal main pancreatic duct on endoscopic retrograde pancreatography; C: Wall thickening in the middle and lower extrahepatic bile duct on abdominal computed tomography (arrowhead); D: Pancreas of normal size; E: Bile duct wall thicking (HE × 40); F: Abundant IgG4-positive plasma cells in bile duct wall (IgG4 staining × 200); G: No inflammation of pancreas tissue (HE × 400).
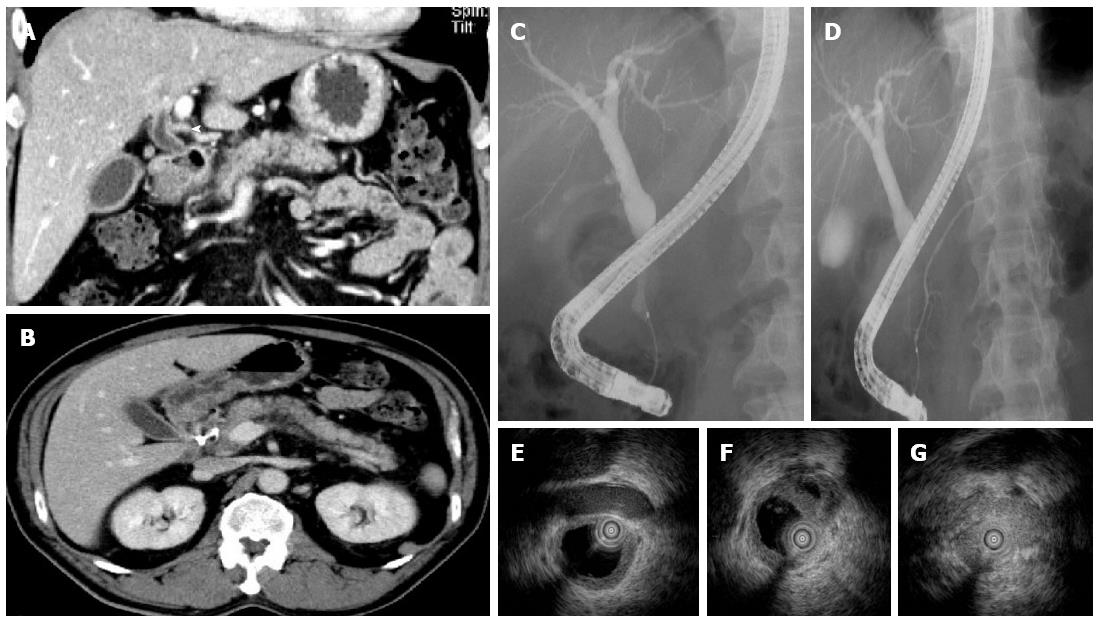
Figure 5 Imaging findings of Case 4.
A: Wall thickness of extrahepatic bile duct on abdominal computed tomography (CT); B: Normal size of the pancreas on abdominal CT; C: Stenosis in the lower extrahepatic bile duct on endoscopic retrograde cholangiography; D: Normal main pancreatic duct on endoscopic retrograde pancreatography; E (at the hilar hepatic lesion); F ( at the bifurcation of cystic duct); G (at the intrapancreatic lesion): Bile duct wall thickening with smooth inner and outer margin in areas with stenosis (G) and without (E, F) on intraductal ultrasonography.
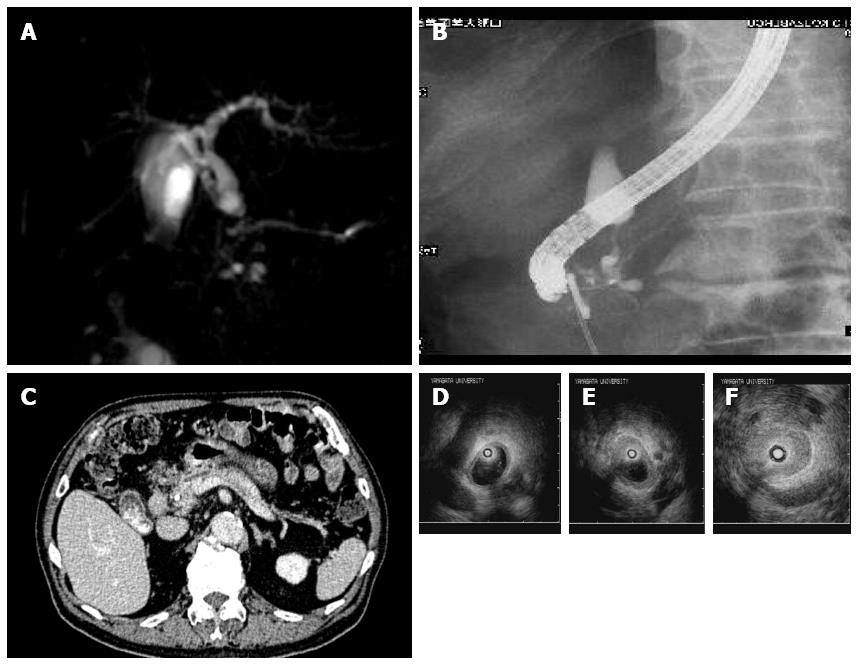
Figure 6 Imaging findings of Case 5.
A, B: Stenosis in the lower extrahepatic bile duct and a slight dilation of the main pancreatic duct on endoscopic retrograde cholangiopancreatography (A) and magnetic resonance cholangiopancreatography (B); C: Normal size of the pancreas on abdominal computed tomography; D (at the hilar hepatic lesion); E (at the bifurcation of cystic duct); F (at the intrapancreatic lesion): Bile duct wall thickening with smooth inner and outer margin in areas with stenosis (F) and without (D, E) on intraductal ultrasonography.
- Citation: Nakazawa T, Ikeda Y, Kawaguchi Y, Kitagawa H, Takada H, Takeda Y, Makino I, Makino N, Naitoh I, Tanaka A. Isolated intrapancreatic IgG4-related sclerosing cholangitis. World J Gastroenterol 2015; 21(4): 1334-1343
- URL: https://www.wjgnet.com/1007-9327/full/v21/i4/1334.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i4.1334