Copyright
©The Author(s) 2015.
World J Gastroenterol. May 21, 2015; 21(19): 5941-5949
Published online May 21, 2015. doi: 10.3748/wjg.v21.i19.5941
Published online May 21, 2015. doi: 10.3748/wjg.v21.i19.5941
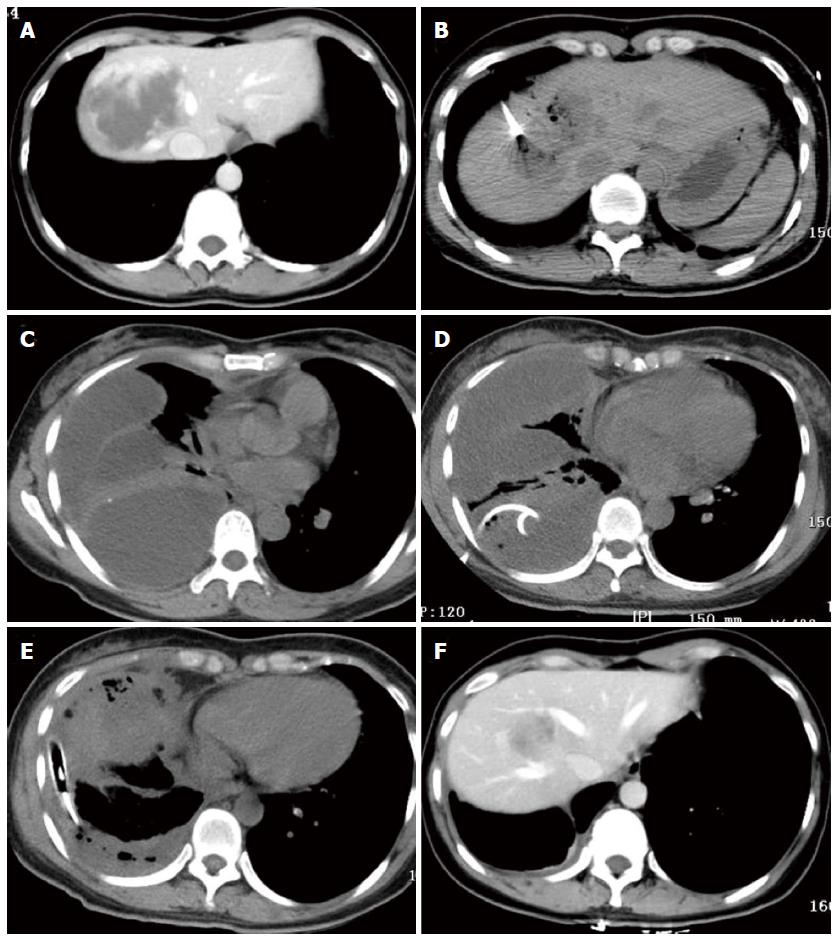
Figure 1 One patient with a 7.
5-cm hemangioma mainly in segment 8 in the computed tomography-guided ablation group developed a diaphragmatic rupture after ablation. A: A 40-year-old woman in the computed tomography (CT)-guided radiofrequency (RF) ablation group had a 7.5-cm hemangioma in segment 8, as illustrated on an abdominal CT scan; B: During CT-guided ablation, the lesion became depressed and commenced outgassing; C: Four days after ablation, CT scan of the chest showed a multiloculated pleural effusion occupying the right hemithorax with collapse of the right lung; D: Drainage via a chest tube was unsuccessful. She subsequently underwent thoracotomy; E: Two chest tubes were inserted into the pleural space; F: At 6 mo after ablation, CT scans showed that the hemangioma was completely ablated and markedly smaller without development of a diaphragmatic hernia.
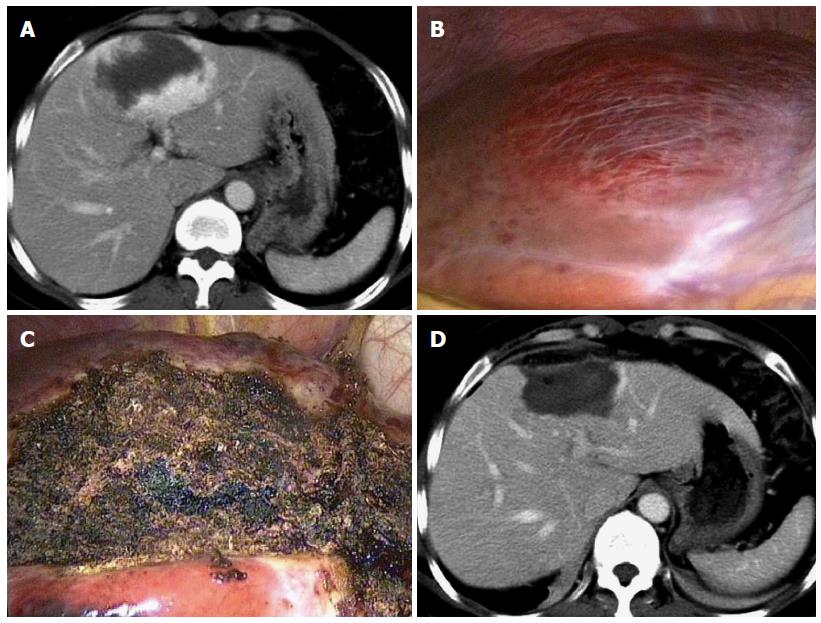
Figure 2 Complete ablation is achieved in a patient in the laparoscopic ablation group.
A: A 45-year-old woman in the laparoscopic ablation group had an 8.0-cm hemangioma in segment 5, as seen on an abdominal computerized tomography (CT) scan; B: On laparoscopic views, the tumor is evident on the superior surface; C: The lesion became a depressed mass of hard texture after RF ablation; D: The hemangioma disappeared completely 1 mo after ablation, as illustrated on an abdominal CT scan.
-
Citation: Gao J, Kong J, Ding XM, Ke S, Niu HG, Xin ZH, Ning CM, Guo SG, Li XL, Zhang L, Dong YH, Sun WB. Laparoscopic
vs computerized tomography-guided radiofrequency ablation for large hepatic hemangiomas abutting the diaphragm. World J Gastroenterol 2015; 21(19): 5941-5949 - URL: https://www.wjgnet.com/1007-9327/full/v21/i19/5941.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i19.5941