Copyright
©2014 Baishideng Publishing Group Inc.
World J Gastroenterol. Jun 28, 2014; 20(24): 7864-7877
Published online Jun 28, 2014. doi: 10.3748/wjg.v20.i24.7864
Published online Jun 28, 2014. doi: 10.3748/wjg.v20.i24.7864
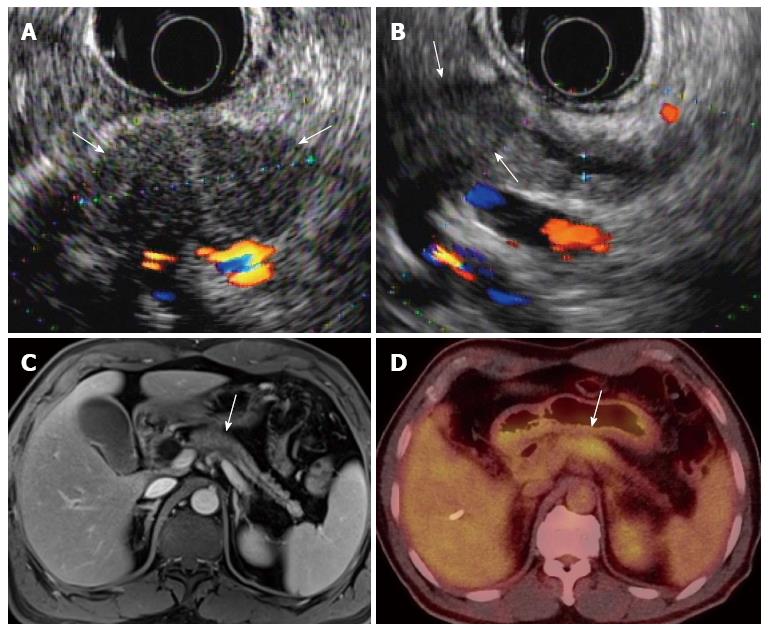
Figure 1 A 58-year-old, male patient with pancreatic body cancer with typical imaging findings.
A, B: Endoscopic ultrasonography shows an approximately 3-cm, hypoechoic mass (arrows) in the pancreatic body with distal pancreatic duct dilatation; C, D: The mass (arrow) shows hypointensity on portal-venous-phase, contrast enhanced MR and hypermetabolism on PET/CT, respectively. MR: Magnetic resonance; PET: Positron emission tomography; CT: Computed tomography.
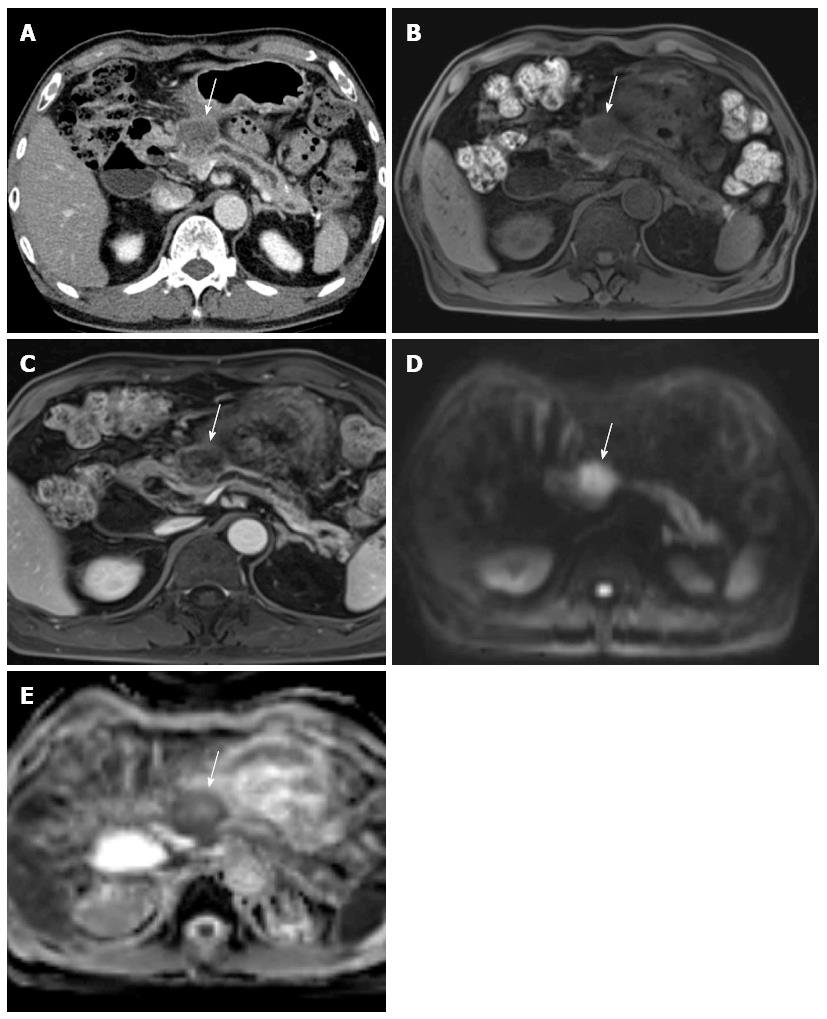
Figure 2 A 73-year-old male with pathologically-proven pancreatic head cancer.
A: Approximately 3 cm low attenuating mass (arrow) is noted at the pancreatic head on the CT scan; B: In pre-contrast T1-weighted gradient echo sequence of MR, this mass (arrow) shows lower signal intensity, compared to the normal pancreatic parenchyma; C: After contrast media administration, the pancreatic head cancer (arrow) has poor enhancement; D, E: DWI with 1000 of b-value and ADC map reveal the diffusion restriction of the pancreatic head cancer (arrow). CT: Computed tomography; MR: Magnetic resonance; DWI: Diffusion weighted imaging; ADC: Apparent diffusion coefficient.
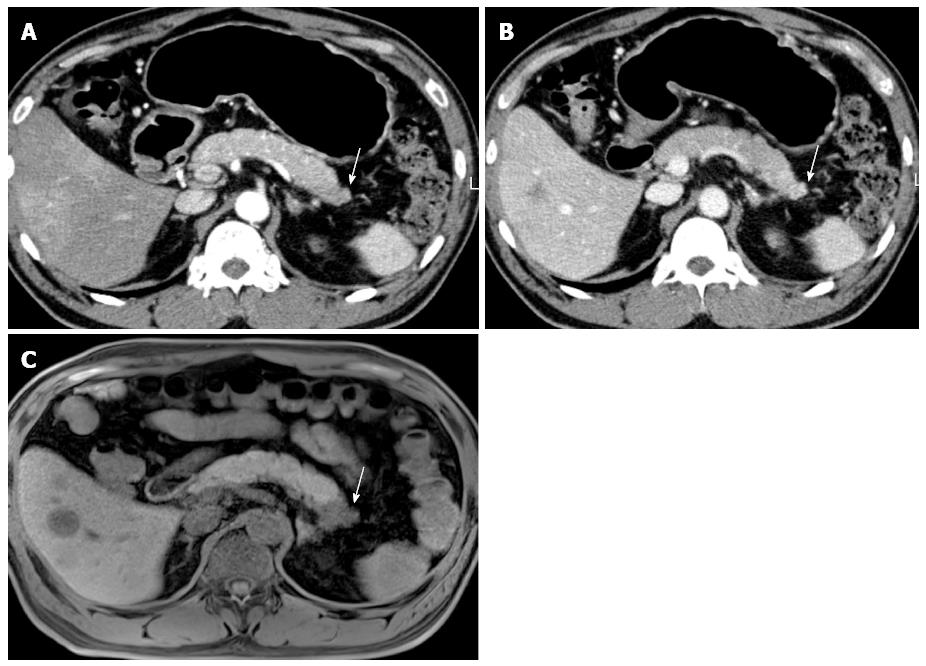
Figure 3 A 64-year-old male with biopsy-proven pancreatic adenocarcinoma with liver metastasis.
A, B: On MDCT, the pancreatic tail mass (arrow) shows isoattenuation, causing distal parenchyma atrophy; C: On pre-contrast, T1–weighted, gradient-echo sequence MRI, the pancreatic tail mass (arrow) is clearly depicted, as well as the liver metastasis, owing to the increased soft-tissue contrast of MR compared with that of CT. MRI: Magnetic resonance imaging; MDCT: Multi-detector computed tomography.
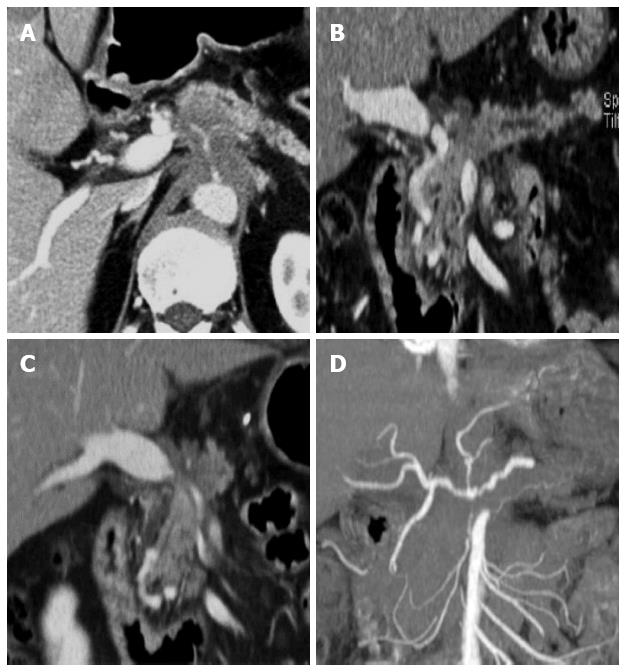
Figure 4 Post-process of multi-detector computed tomography for pancreatic cancer.
A: In the axial CT scan, an ill-defined pancreatic body cancer invading the celiac axis is identified; B: On the curved MPR along the pancreatic duct, the relationship between the pancreatic duct and the cancer can be more easily understood; C, D: The extent and degree of major vascular involvement caused by the pancreatic cancer can be comprehensively assessed using MPR and the maximum intensity projections. MDCT: Multi-detector computed tomography; MPR: Multiplanar reformations.
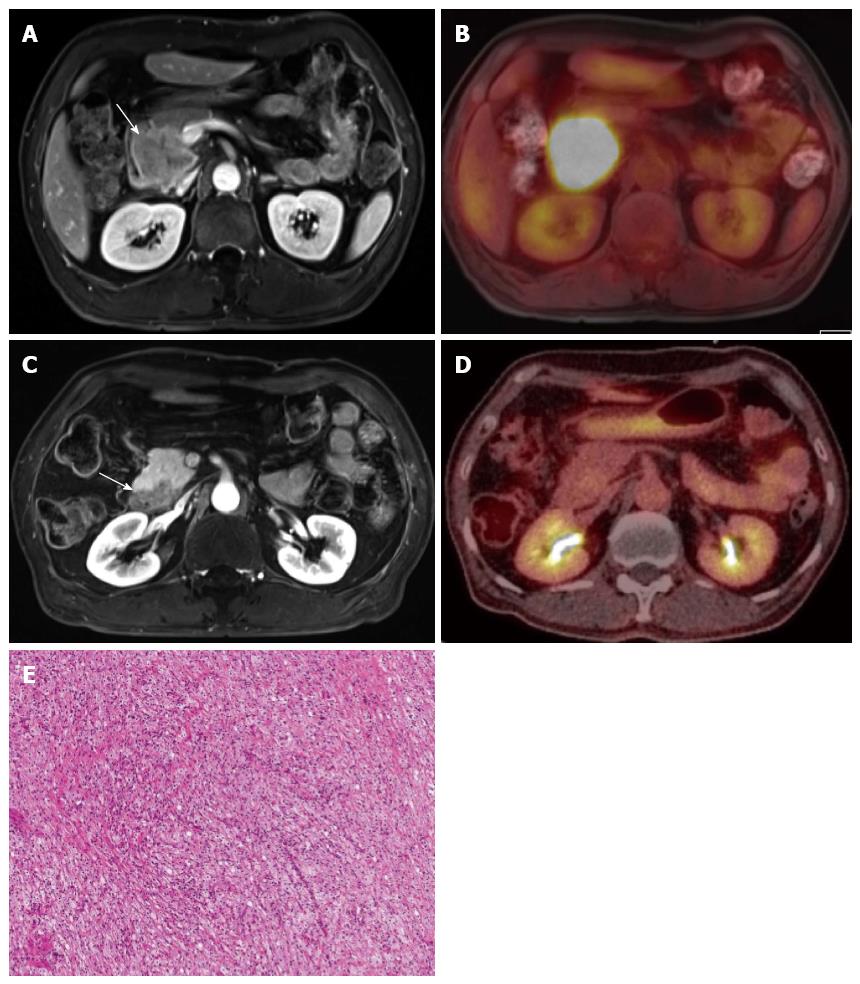
Figure 5 Treatment monitoring of pancreatic cancer using positron emission tomography/magnetic resonance.
A, B: A 5-cm mass of biopsy-proven, adenosquamous carcinoma (arrow) in the pancreatic head, as seen due to the strong FDG uptake; C, D: The mass (arrow) shows a marked decrease in size and glucose metabolism (from 22.0 to 3.8 of mSUV) after six cycles of neoadjuvant concurrent chemoradiation treatment. The specimen obtained during the following surgery revealed complete remission; E: All tumor cells are replaced by a foamy histiocytes collection of cholesterol clefts and multinucleated giant cells. PET: Positron emission tomography; MR: Magnetic resonance; FDG: Fluorodeoxyglucose; mSUV: Maximum standardized uptake value.
- Citation: Lee ES, Lee JM. Imaging diagnosis of pancreatic cancer: A state-of-the-art review. World J Gastroenterol 2014; 20(24): 7864-7877
- URL: https://www.wjgnet.com/1007-9327/full/v20/i24/7864.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i24.7864