Copyright
©2013 Baishideng Publishing Group Co.
World J Gastroenterol. Feb 14, 2013; 19(6): 829-837
Published online Feb 14, 2013. doi: 10.3748/wjg.v19.i6.829
Published online Feb 14, 2013. doi: 10.3748/wjg.v19.i6.829
Figure 1 Computed tomography of insulinoma of the pancreas.
Typically, insulinomas (arrow) are hypervascular and, as a result, demonstrate a greater degree of enhancement than normal pancreatic parenchyma during the arterial and capillary phases of contrast bolus.
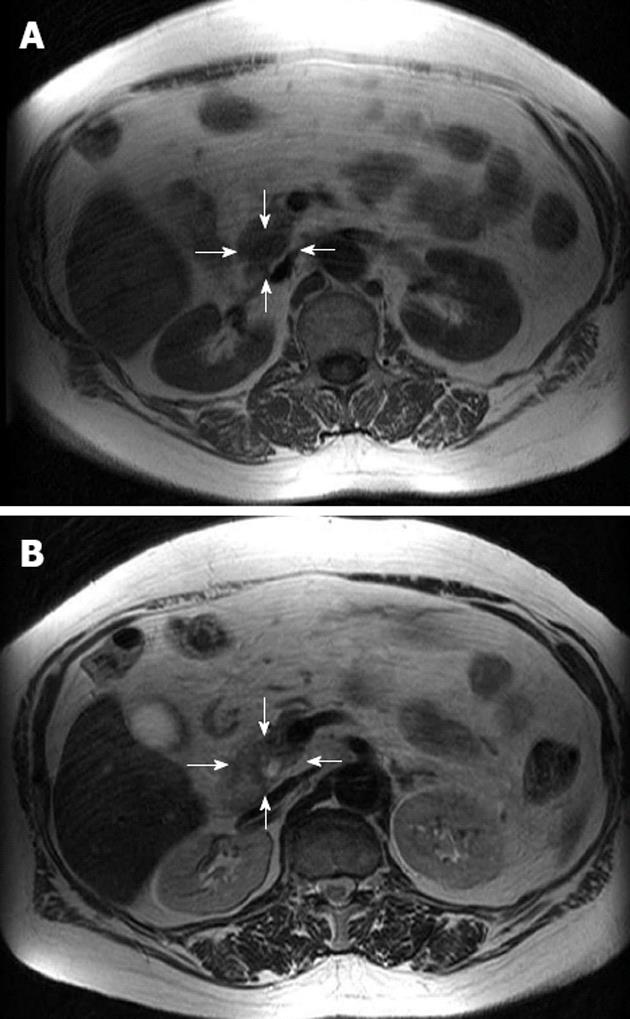
Figure 2 Magnetic resonance imaging of insulinoma of the pancreas.
Insulinomas (arrows) generally demonstrate low signal intensity on T1-weighted images (A) and high signal intensity on T2-weighted images (B).
Figure 3 Endoscopic ultrasound features of insulinoma of the pancreas.
The appearance of insulinomas (arrows) on endoscopic ultrasonography is quite characteristic, with most tumors homogeneously hypoechoic, rounded in shape, and with distinct margins.
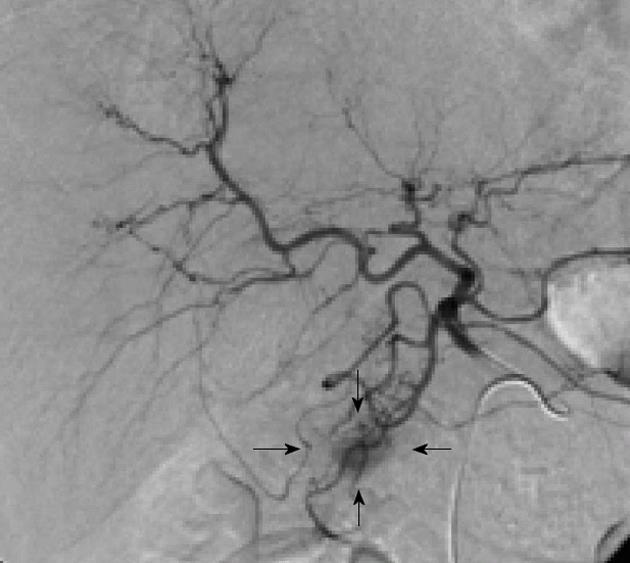
Figure 4 Angiography and arterial stimulation venous sampling.
Using arterial stimulation venous sampling, insulinomas (arrows) are seen as well-defined, round or oval vascular blushes that are of increased vascularity compared with the surrounding normal pancreatic parenchyma.
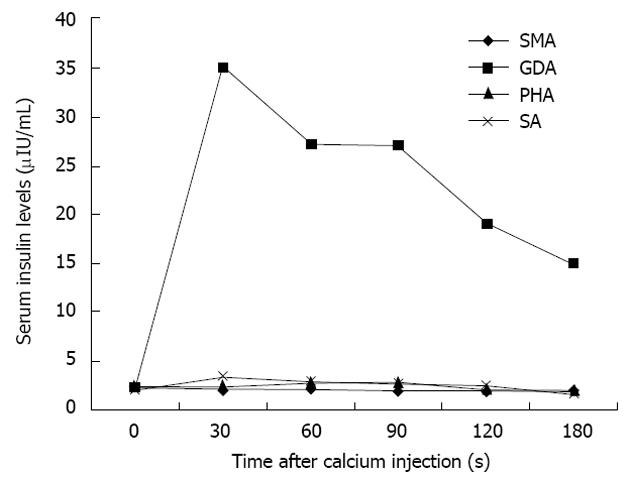
Figure 5 Changes in serum insulin levels.
Changes in serum insulin levels plotted as a function of time after calcium injection indicate that insulin concentrations are markedly elevated only in the feeding arteries of the insulinoma. SMA: Superior mesenteric artery; GDA: Gastroduodenal artery; PHA: Proper hepatic artery; SA: Splenic artery.
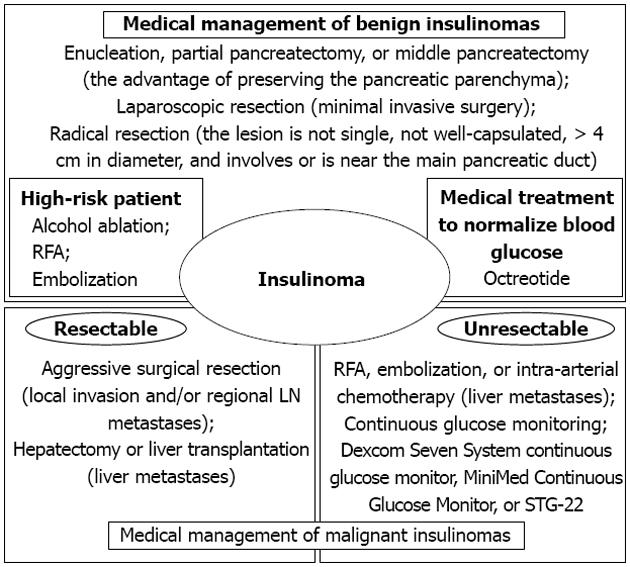
Figure 6 In patients who have unresectable or uncontrollable malignant insulinomas of the pancreas, several strategies need to be considered to both control hypoglycemic episodes and improve quality of life, including administration of ocreotide and continuous glucose monitoring.
RFA: Radiofrequency ablation; LN: Lymph node.
- Citation: Okabayashi T, Shima Y, Sumiyoshi T, Kozuki A, Ito S, Ogawa Y, Kobayashi M, Hanazaki K. Diagnosis and management of insulinoma. World J Gastroenterol 2013; 19(6): 829-837
- URL: https://www.wjgnet.com/1007-9327/full/v19/i6/829.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i6.829