Published online Nov 6, 2019. doi: 10.12998/wjcc.v7.i21.3436
Peer-review started: July 16, 2019
First decision: September 9, 2019
Revised: September 27, 2019
Accepted: October 5, 2019
Article in press: October 5, 2019
Published online: November 6, 2019
The major reason for filtering bleb failure or scarring of the bleb site is due to excessive scarring after glaucoma filtration surgery in the clinic. Traditional Chinese medicine has preeminence in the prevention of fibrosis formation through the regulation of systemic circulation and improvement of the properties of the inflammatory cells in the blood.
To examine the clinical efficacy of using the Modified Cortex Mori Capsules (MCMC; Chinese name: Jiawei Sangbaipi Capsules) in the success rate of functional filtering blebs after glaucoma filtering surgery in clinical patients.
Sixty resurgery glaucoma patients were randomly divided into two groups: 30 patients in surgery with the placebo group and 30 patients in surgery with the MCMC group. Patients took either the placebo or the MCMC 2 wk before and after surgery. Postoperative morphology and function filtering bleb, visual acuity, intraocular pressure, postoperative complications, the success rate of filtration surgery and clinical efficacy were observed.
Fifty patients completed the study. The percentage of functional filtering blebs in the surgery plus MCMC group was 84% at 6 mo after surgery, which was higher than surgery plus placebo group (64%, P < 0.05). The surgical success rate in the MCMC and placebo groups were 79% ± 8.3% and 57% ± 10.6% respectively (P < 0.05). The visual acuity, intraocular pressure and the postoperative complications in the two groups had no significant differences.
Glaucoma filtering surgery while taking MCMC not only reduced excessive scar formation and increased the success rate of functional filtering blebs but also improved the success of glaucoma filtration operations.
Core tip: Glaucoma is one of the leading causes of irreversible blindness. Trabeculectomy is one of the effective surgical techniques, which creates a new drainage channel, resulting in the formation of a subconjunctival bleb. The major reason for filtering bleb failure or scarring of the bleb site is due to excessive scarring after surgery. In this study, we established that the Modified Cortex Mori Capsules have a propensity to increase functional filtering bleb formation and enhance surgical success rate after glaucoma filtering surgery. Intervening with traditional Chinese medicine could be an effective way for improving surgical success.
- Citation: Yu J, Qiu LX, Qing GP, Zhao BW, Wang H. Modified Cortex Mori Capsules improving the successful rate of functional filtering blebs after reclinical glaucoma filtering surgery. World J Clin Cases 2019; 7(21): 3436-3445
- URL: https://www.wjgnet.com/2307-8960/full/v7/i21/3436.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i21.3436
Glaucoma is one of the leading causes of irreversible blindness worldwide, and it affects more than 70 million people with approximately 10% being bilaterally blind[1]. Glaucoma is an optic neuropathy characterized by the progressive degeneration of retinal ganglion cells[2-4]. Degeneration of these nerves results in visual field defects, optic disc cupping and visual loss[5]. The biological basis and pathological mechanisms of glaucoma remain poorly understood, and the factors contributing to its progression have not been fully described[6]. Slowing disease progression and preservation of quality of life are the main goals for glaucoma treatment.
Currently, reduction of intraocular pressure (IOP) is the only proven method to treat glaucoma[7]. Glaucoma filtering surgery is the most common treatment used to control IOP[8]. Trabeculectomy is an effective surgical option that creates a new drainage channel to filter aqueous humor from the anterior chamber to the outer surface of the sclera, resulting in the formation of a subconjunctival bleb and a decrease in IOP[9,10]. However, the filter can fail if scar tissue forms between the conjunctiva/Tenon’s capsule and the sclera at the surgical site[11]. Scar formation is most commonly due to the proliferation of fibroblasts and the synthesis of the extracellular matrix (mainly collagen synthesis and glucose glycan ammonia)[12]. In current clinical practice, first-line perioperative antiproliferative drugs are 5-fluorouracil and mitomycin-C (MMC). MMC is an antitumor drug that inhibits fibroblast proliferation and alters conjunctival vascular epithelium[8]. It has improved the success rate of filtration surgery. MMC is nonspecific and can increase the risk of severe side effects such as cornea toxicity reaction, conjunctival wound leak, low IOP, etc[13,14]. Therefore, therapeutic agents that can either alone or with MMC improve the reduction of bleb scarring and inhibit complications need to be investigated.
In traditional Chinese medicine (TCM), the scar formation after glaucoma filtering surgery mostly belongs to Phlegm-heat. The Modified Cortex Mori Capsules (MCMC, Jiawei Sangbaipi Capsules) has been used to treat Phlegm-heat syndrome. The pharmaceutical composition of MCMC is based on the concept of TCM and can treat both the symptoms and the causes of glaucoma. It contains a combination of raw materials from herbs that can nourish vital energy, promote blood stasis and prevent bleeding, clear and/or soften phlegm, promote the absorption exudate, edema, and hemorrhage and reduce angiogenesis lesion, thereby improving functional filtering bleb formation. From a contemporary biological point of view, the compounds in the pharmaceutical composition could also target oxidative stress and inflammation. In this study, we evaluate the clinical effects of MCMC on prevention scarring of the filtering bleb after trabeculectomy.
The study protocol was approved by the institutional review board of Beijing Tongren Hospital in China and took place from Jan 2016 to Dec 2018. The inclusion criteria were as follows: (1) Subjects were 20–60 years old; (2) Subjects were diagnosed with primary angle-closure glaucoma and primary open-angle glaucoma; (3) Subjects underwent at least once trabeculectomy and needed resurgery; (4) Subjects diagnosed with Phlegm-heat in TCM dialectical syndrome: TCM syndrome diagnosis standards were according to Disease Diagnosis Curative of TCM ‘Jin Gan’ (phlyctenular conjunctivitis). Phlegm-heat dialectical syndrome was defined as phlyctenular conjunctivitis, conjunctival congestion, more secretions, dry eye, red tongue, yellow coating and rapid pulse; and (5) Subjects signed written informed consent.
Exclusion criteria were as follows: (1) Subjects had neovascular glaucoma and diagnosed as secondary glaucoma; (2) Subjects had scar diathesis; (3) Subjects had other eye diseases, including non-glaucomatous optic neuropathy or severe cataract; (4) Subjects had received cataract surgery within the previous 3 mo; (5) Subjects had a serious systemic disease or mental illness; (6) Subjects had uveitis, retinal detachment, optic nerve diseases or highly myopic eyes; (7) Subjects had significant cardiovascular, liver, kidney, or hematopoietic systems diseases, mental illness and other serious medical conditions; (8) Subjects were pregnant, planning to become pregnant or lactating; (9) Subjects were allergic to Chinese herbal medicines; and (10) Subjects had participated in any other clinical trials in the previous month.
MCMC (Jiawei Sangbaipi Capsules) contains Cortex Mori (Sangbaipi), Bark of Chinese Wolfberry (Digupi), Root of Baikal Skullcap (Huangqin), Root of Dwarf Lilyturf (Maidong), Platycodon Root (Jiegeng), Fruit of Seville Orange (Zhiqiao), Chrysanthemum Flower (Juhua) and Inula Flower (Xuanfuhua). The herbs’ quality was tested by our hospital TCM pharmacy. The capsule was made with an equal weight of all herbs (15 g) in our hospital TCM pharmacy. Each capsule contains 15 mg total herb medicine. The placebo was made with an equal weight of starch. Four capsules of MCMC or placebo were taken orally two times a day, 30 min after breakfast and dinner.
From initial screening visits, 60 glaucoma patients with trabeculectomy resurgery were recruited from the eye department of Beijing Tongren Hospital in China. All subjects received standard treatment without any dietary intervention. A biostatistician conducted a stratified sample, the block randomization method. Patients were assigned into two groups: 30 patients receiving placebo and 30 patients receiving MCMC. After 6 mo, 50 patients completed the study.
Subjects were orally administered with MCMC capsules and placebo two times daily, 30 min after breakfast and dinner. Each capsule pill contained 15 mg of herbal medicine. The Pharmacy of Tongren Hospital provided all study medications. The treatment for each group started 2 wk before surgery and lasted 2 wk after surgery (four consecutive weeks).
All patients underwent standard trabeculectomy by two specified ophthalmologists according to the modification of Cairns using a fornix-based conjunctival flap[15]. Briefly, the IOP must be controlled under 21 mmHg before surgery, and 20% mannitol intravenous may be used when necessary. After raising a fornix-based conjunctival flap, a rectangular 4 mm x 4 mm x 0.3 mm scleral flap was dissected at the 12-o’clock position. Surgical absorbent sponge pieces soaked in a 0.04% MMC solution prepared just before use were placed between the episclera and conjunctival flap for 5 min. After removal of the sponge pieces, the site was rinsed with 100 mL of balanced salt solution. Then, a 2 mm x 3 mm sclerotomy was created, after which a peripheral iridectomy was performed. The sclera flap was closed using two relatively lose 10-0 nylon sutures. Finally, the conjunctiva was closed and topical tobramycin 0.3% and dexamethasone 0.1% (Tobradex, Alcon Pharmaceuticals, Fort Worth, TX, United States) were given every day until the 6th week postoperatively.
Follow-up visits were scheduled at day 1, day 3, day 7, day 14, 1 mo, 3 mo and 6 mo after the operation. After 14 d, each examination included best-corrected visual acuity, the IOP (average of three separate readings), slit-lamp microscopy (including bleb appearance and anterior chamber inflammation), fundoscopic examination and visual field.
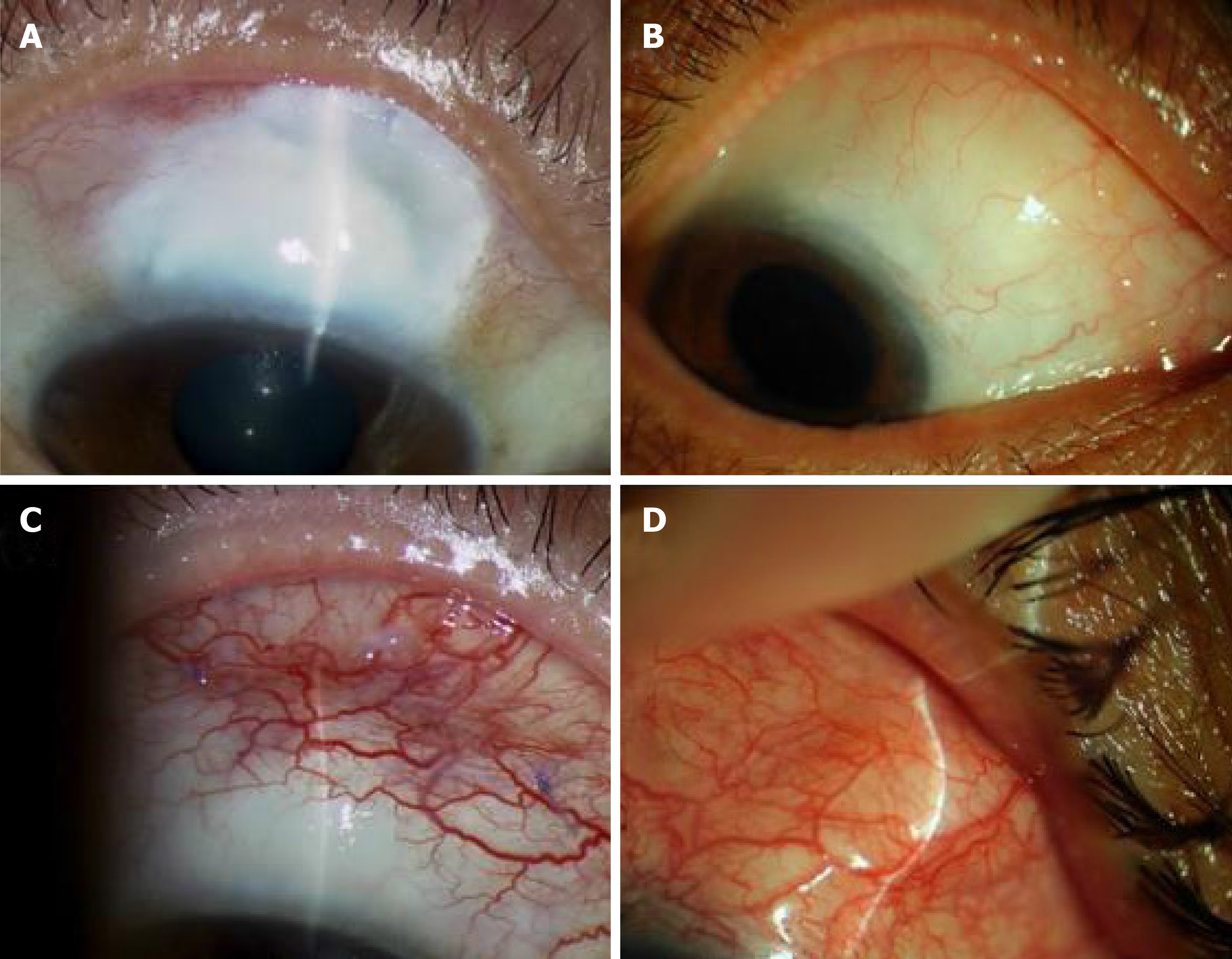
Four types of filtering bleb were diagnosed as follow: Type I (small cystic type): thin capsule wall, no vessels with tiny cystic; Type II (flat diffuse type): thicker capsule wall, flat, diffuse and pale filtering bleb; Type III (scar type): no filtering bleb or conjunctiva congestion, rich vessels and scarring on the filtering bleb; and Type IV (package type): cystic hyperplasia, limitations of uplift filtering bleb (Figure 1). Type I and Type II are functional filtering bleb, while Type III and Type IV are dysfunctional filtering bleb[16].
The following indicators determined a successful surgery: (1) The IOP maintained under 15 mmHg after surgery; (2) No visual acuity progressive decrease; (3) No visual field continued damage; and (4) No cup-to-disc ratio increase.
The postoperative complication examination included corneal epithelium damage, conjunctiva wound leakage, shallow anterior chamber, uveitis, low IOP, choroid detachment, retinal detachment, hemorrhage, aggravate lens opacity, endophthalmitis and filtering bleb rupture.
Categorical variables were analyzed using the chi-square test, and continuous variables were analyzed using the unpaired Student’s t-test. The data were analyzed using SPSS software (version 19.0, SPSS Inc., Chicago, IL, United States). Correlation was considered significant as P value < 0.05.
Sixty subjects who met the inclusion criteria in the clinic in the eye department of Beijing Tongren Hospital were enrolled in this study and were placed randomly into either the placebo or MCMC group. The mean age of the subjects was 40.5 years old, and among them 37 were female. The variance test of the IOP value, medicine intake and number of glaucoma surgeries had no significant difference between the two groups (Table 1). At the 6-mo follow up, 50 subjects had completed the study.
| Placebo | MCMC | P value | |
| Gender | 1.20 ± 0.23 | 1.19 ± 0.281 | > 0.05 |
| Age | 40.30 ± 8.82 | 39.79 ± 6.15 | > 0.05 |
| IOP | 38.20 ± 2.47 | 37.88 ± 3.16 | > 0.05 |
| C/D | 0.70 ± 0.32 | 0.70 ± 0.17 | > 0.05 |
| Surgery times | 1.35 ± 0.56 | 1.33 ± 0.53 | > 0.05 |
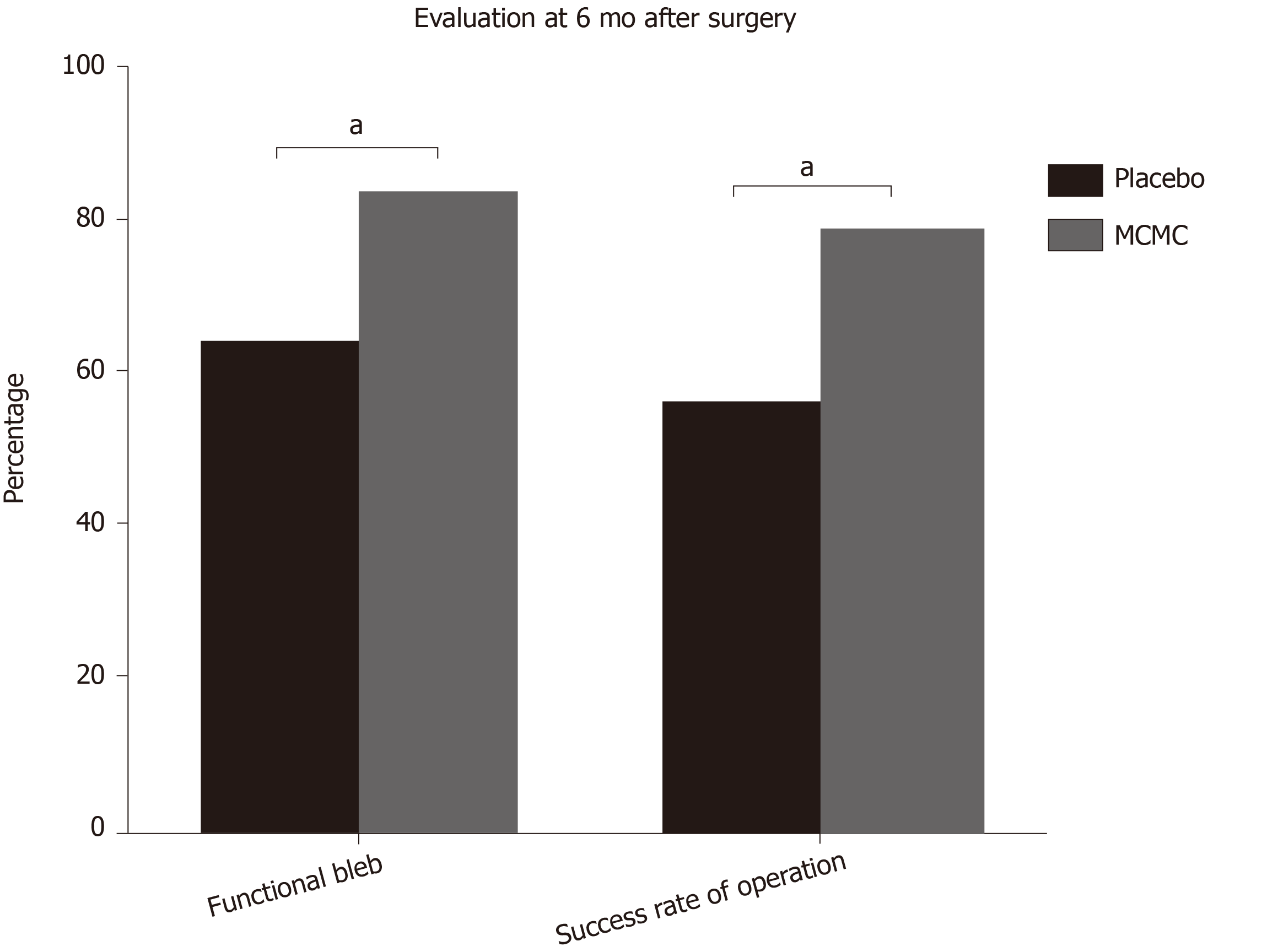
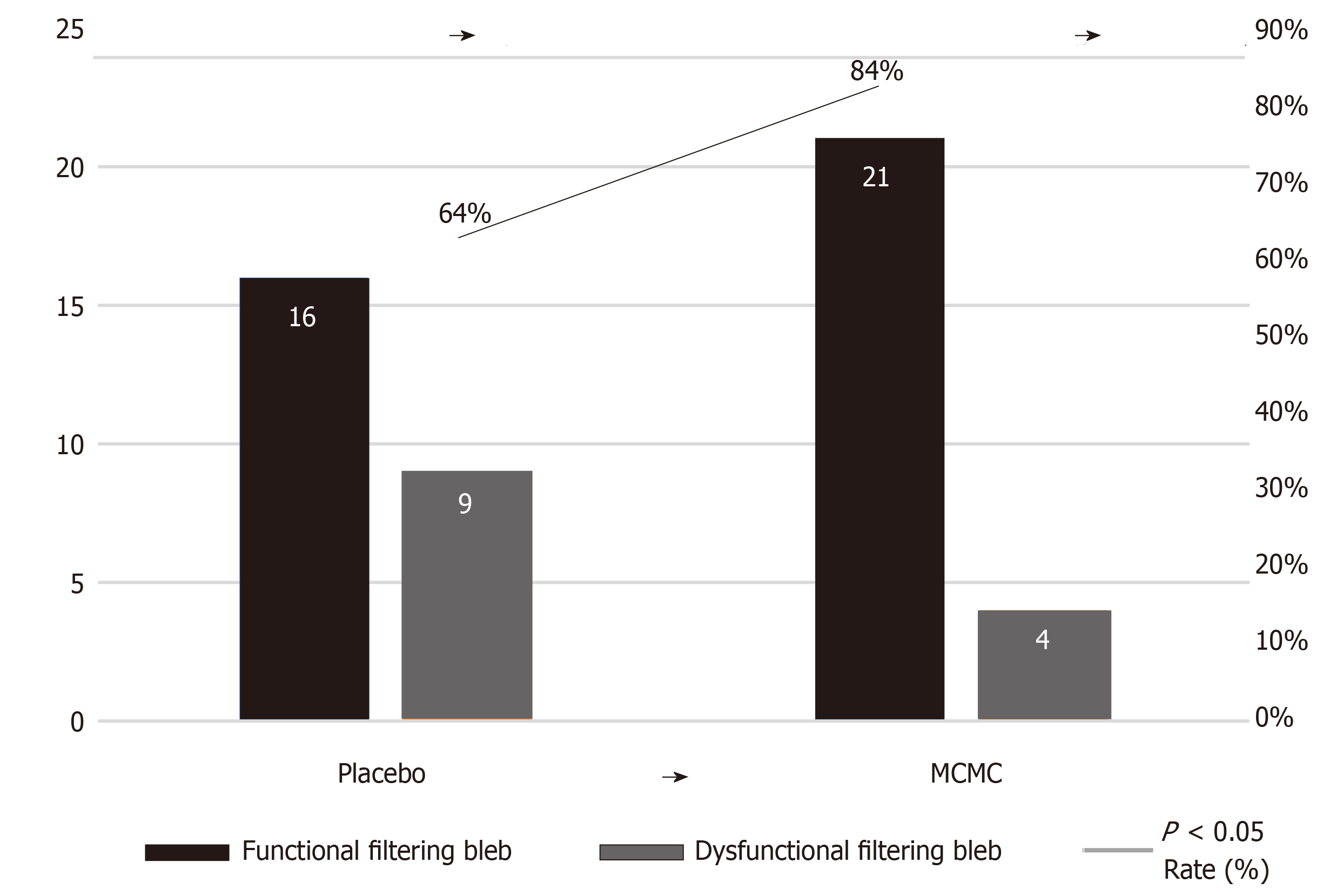
Six months after the operation, there were 84% functional filtering bleb in the combination surgery and MCMC group, while there were 64% functional filtering bleb in the surgery and placebo group. Comparison between the two groups had a significant difference (P < 0.05, Table 2 and Figure 2). The successful surgery was determined with the IOP controlled under 15 mmHg, no progressive visual acuity, visual field and optic disc damage. The rate of success 6 mon after surgery in the MCMC group was 79% ± 8.3 %, which was significantly higher than the placebo group (57% ± 10.6%, P < 0.05, Table 2 and Figures 2 and 3).
| Placebo | MCMC | P value | |
| Functional filtering bleb | 16 | 21 | |
| Dysfunctional filtering bleb | 9 | 4 | |
| Rate, % | 64 | 84 | < 0.05 |
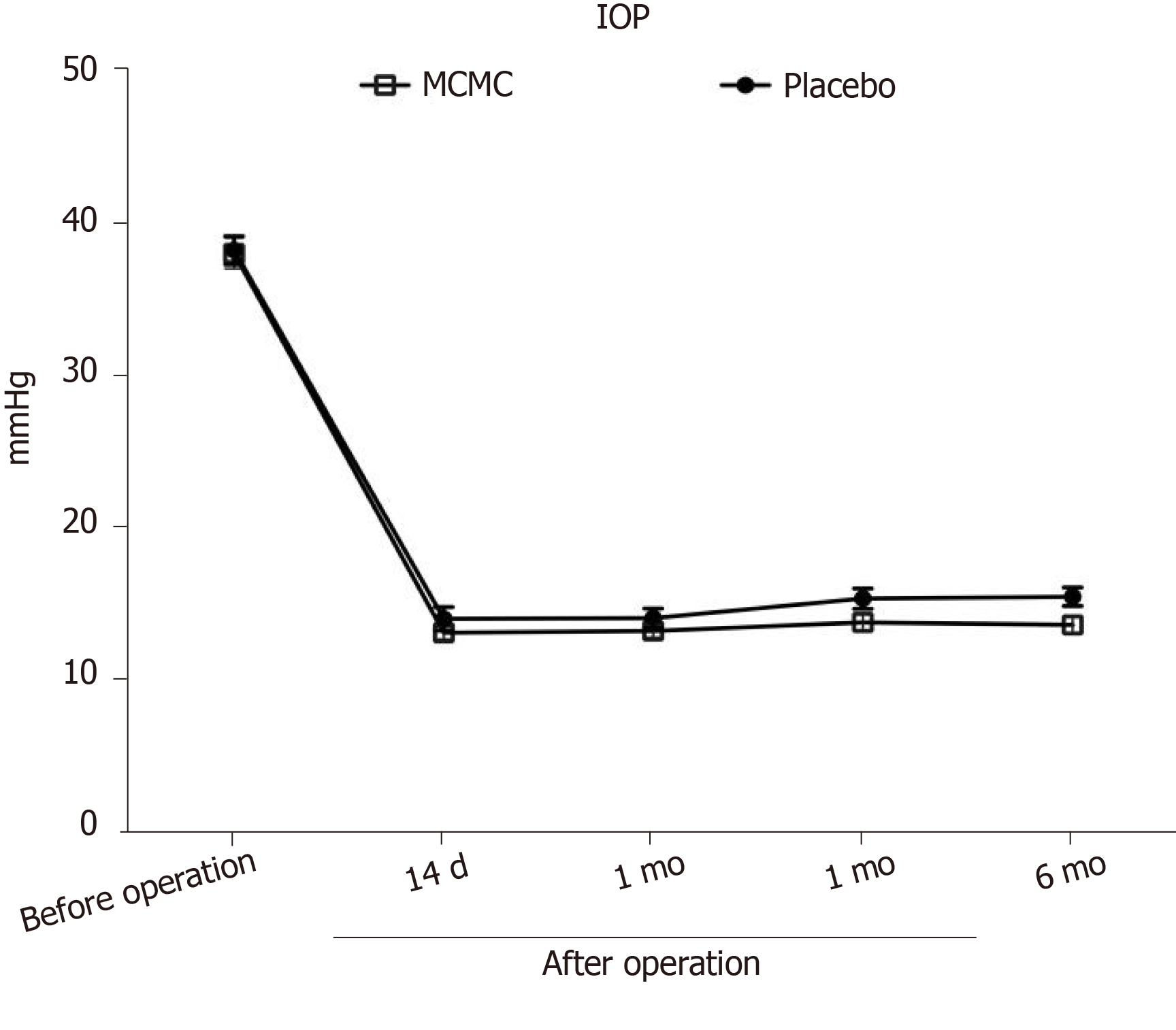
During the 6 mo follow up after trabeculectomy surgery, the complications including corneal epithelium damage, shallow anterior chamber and aggravated lens opacity, but there were no significant differences between the two groups (P > 0.05, Table 3). However, the MCMC group showed less local postoperative inflammation such as local blood congestions and swellings in the conjunctiva. The IOP measurement at different times showed a significant decrease in IOP value post operation and maintained around 15 mmHg in both the MCMC and placebo group (Figure 4). However, we observed the trend of the IOP level becoming more stable in the MCMC group compared to the placebo group.
| Placebo | MCMC | P value | |
| Corneal epithelium damage | 7 | 5 | > 0.05 |
| Conjunctiva wound leakage | 0 | 0 | > 0.05 |
| Shallow anterior chamber | 2 | 1 | > 0.05 |
| Uveitis | 0 | 0 | > 0.05 |
| Low IOP | 0 | 0 | > 0.05 |
| Choroid detachment | 0 | 0 | > 0.05 |
| Progressive lens opacity | 2 | 2 | > 0.05 |
| Endophthalmitis | 0 | 0 | > 0.05 |
| Filtering bleb rupture | 0 | 0 | > 0.05 |
No adverse effects with clinical signs were observed in the two groups during the study using the chi-square test. The number of reported minor adverse effects in the placebo was observed, but there was no statistically significant difference in the frequency of adverse effects between the groups (P = 0.622, Table 3).
Glaucoma is one of the progressive eye diseases that cause irreversible blindness, and there are no cures so far. Currently, IOP is the primary and most effective proven therapeutic method[7,8]. Trabeculectomy is considered the gold standard in surgical management of glaucoma[17]. However, surgery failures often happen in some patients[18,19].
The most prevalent reason for failure in filtration surgery is post operation scarring in the filtration path, and the failure rate reaches 15%-25% within two years post operation[20]. Due to the overhealing of subconjunctiva at the bleb and sclerotomy site, the successful rate of reoperation is only 36%-51%[21]; therefore scarring of the filtration path is the most intractable problem for filtration surgery. Currently, the first line of perioperative antiproliferative treatment is MMC. MMC is an antitumor antibiotic isolated from Streptomyces, inhibits the synthesis of DNA and protein, prevents fibroblasts, produces collagen material and improves the success rate of the filtration surgery. But still, some patients need surgery even with MMC because the time of MMC immersion is deficient. The efficacy of the antimetabolism treatment is transient or is due to the systemic conditions of the patient. Therefore, to find an effective, long-lasting alternative that can assist MMC with antiscarring is an important area for further investigation for glaucoma.
TCM is used in treating cancer, preventing carcinogenesis, inhibiting cell proliferation, arresting the cell cycle, inducing apoptosis, inhibiting angiogenesis and regulating immune function[22-24]. TCM is also used to inhibit myocardial fibrosis by inhibiting expression of inflammatory mediators associated with NF-kB signaling thereby blocking the upregulation of pro-inflammatory cytokines (IL-1β, TNFα) and chemokine (MCP-1), macrophage infiltration and inactivating TGF-β/Smad3 signaling. These actions suppress fibrosis including expression of fibronectin, collagen I and collagen IV[25,26]. TCM’s mechanisms of action differ greatly from that of Western medicine. Whereas Western medicine employs purified molecules that exert a concentrated, single target effect, the effects of TCM are generally regarded as multifunctional and through a systemic regulation to affect the target. These effects are due to the complex formulation of herbal medicine that exerts global effects on multiple organ systems or targets. As we know, herbs contain many active components[27-29]. Thus, in many cases, using a general or crude extract that contains multiple active components is more biologically powerful than a purified extraction containing only one or a few active components[30]. The modern approach of using standardized extracts and herbal formulas can offer a high degree of quality control and standardization for a crude extract of TCM when they are used in the research of herbal bio effects, thus preserving the multisystem targets for neuroprotection that is possible from TCM tonics[31].
Glaucoma belongs to “Lü Feng Nei Zhang” and/or “Qing Feng Nei Zhang” in the theory of TCM. According to TCM classical literature of “Shen Shi Yao Han” (written by Ren-Yu Fu et al, 1671) and “Mu Jing Da Cheng” (Written by Ting-Jing Huang, 1741), the guidance of clinical practice in TCM ophthalmology is the theory of “Five Wheels of the Eye.” The bulbar conjunctiva and sclera in this theory are called “Bai Jing” and named “Qi Wheel.” These tissues’ corresponding organ is the “Lung,” and in the clinic of TCM ophthalmology, the conjunctiva and sclera diseases are treated often from “Lung” dysfunction. This perspective of TCM, the dysfunction of “lung heat” causes bulbar conjunctiva and sclera disorder or inflammation, which cause scarring. “Sang Bai Pi Tang” is a typical method that treats “lung heat” in clinics of TCM, such as chronic conjunctivitis, dry eye disease and shallow scleritis.
MCMC is the crude herb formula compound produced from the formula of “Sang Bai Pi Tang” and clinical experiences. In this study, MCMC can significantly improve functional filtering bleb formation, increase success rate of the surgery and decrease local inflammation. The MCMC formula contains Sangbaipi, Digupi, Huangqin, Maidong, Jiegeng, Zhiqiao, Juhua and Xuanfuhua that are strong and effective in clearing heat and moistening the lung, which could systemically regulate blood circulation and immune cell properties that were important for the local inflammation formation. Nevertheless, approving the efficacy of MCMC requires not only requires a large number of clinical trials and long-term observations but also requires in vitro experiments. Further animal experiments or cell culture may further identify the mechanism of MCMC in the improvement of the functional filtering blebs after reclinical glaucoma filtering surgery.
In conclusion, in this study, we established that MCMC has a propensity to increase functional filtering bleb formation and enhance surgical success rate after glaucoma filtering surgery. There is no significant difference in the postoperative complications between the MCMC and placebo groups. Intervening with TCM could be an effective way for improving surgical success, and it may open an avenue to treat glaucoma by combining TCM and western medicine.
Trabeculectomy is one of the effective surgical techniques for glaucoma, which creates a new drainage channel, resulting in the formation of a subconjunctival bleb. Scarring of the bleb site is the main cause of the failure of the filter. Use of antiproliferative drugs has improved the success rate of the filtration surgery, but they also increase the risk of severe side effects. In our study, we established that the Modified Cortex Mori Capsules (MCMC) have a propensity to increase functional filtering bleb formation and enhance surgical success rate after glaucoma filtering surgery.
To find an effective method to inhibit scar tissue formation at the filtering surgery surgical site. According to the theory of traditional Chinese medicine (TCM), the scar formation after glaucoma filtering surgery mostly belongs to Phlegm-heat. The pharmaceutical composition of MCMC is based on the concept of TCM and can treat both the symptoms and the causes of the glaucoma. In this study, we evaluated the clinical effects of MCMC in prevention of scarring of the filtering bleb after trabeculectomy.
Our aim was to examine the clinical effects by using MCMC (Chinese name: Jiawei Sangbaipi Capsules) in the success rate of functional filtering blebs after filtering surgery.
This study was a prospective clinical randomized controlled study. The enrollment of patients was in strict accordance with inclusion and exclusion criteria. Sixty postoperative patients were randomly divided into two groups: 30 patients in the surgery and placebo group and 30 patients in the surgery and MCMC group. Patients took the placebo or the MCMC 2 wk before and after surgery. Categorical variables and continuous variables were analyzed.
The percentage of functional filtering blebs in MCMC group was 84% at 6 mo after surgery, which was significantly higher than placebo group. The surgical success rate in the MCMC group and the placebo group were 79% ± 8.3% and 57% ± 10.6%, respectively (P < 0.05); Other indicators of the two groups had no significant differences. MCMC not only reduced excessive scar formation and increased success rate of functional filtering blebs but also improved the success of glaucoma filtration operations.
In this study, we observed that MCMC can significantly improve functional filtering bleb formation, increase success rate of the surgery and decrease local inflammation. The mechanisms of MCMC in improving the functional filtering blebs after reclinical glaucoma filtering surgery require further investigation.
Surgery is one of the most effective methods to treat glaucoma. The reasons that cause the failure of the surgery are very complicated. The theory of TCM recognizes glaucomatous postoperative signs differently than western medicine. TCM provides a new choice to improve the success rate of glaucoma filtering surgery. The efficacy of MCMC still needs large clinical trials and long-term observations as well as in vitro experiments.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Georgescu EF, Siddiqui I S-Editor: Wang JL L-Editor: Filipodia E-Editor: Liu MY
| 1. | Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90:262-267. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4855] [Cited by in F6Publishing: 4648] [Article Influence: 258.2] [Reference Citation Analysis (0)] |
| 2. | Kwon YH, Fingert JH, Kuehn MH, Alward WL. Primary open-angle glaucoma. N Engl J Med. 2009;360:1113-1124. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 527] [Cited by in F6Publishing: 609] [Article Influence: 40.6] [Reference Citation Analysis (0)] |
| 3. | Quigley HA, Dunkelberger GR, Green WR. Retinal ganglion cell atrophy correlated with automated perimetry in human eyes with glaucoma. Am J Ophthalmol. 1989;107:453-464. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 658] [Cited by in F6Publishing: 706] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 4. | Kerrigan-Baumrind LA, Quigley HA, Pease ME, Kerrigan DF, Mitchell RS. Number of ganglion cells in glaucoma eyes compared with threshold visual field tests in the same persons. Invest Ophthalmol Vis Sci. 2000;41:741-748. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Weinreb RN, Khaw PT. Primary open-angle glaucoma. Lancet. 2004;363:1711-1720. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1247] [Cited by in F6Publishing: 1327] [Article Influence: 66.4] [Reference Citation Analysis (0)] |
| 6. | Nickells RW, Howell GR, Soto I, John SW. Under pressure: cellular and molecular responses during glaucoma, a common neurodegeneration with axonopathy. Annu Rev Neurosci. 2012;35:153-179. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 198] [Cited by in F6Publishing: 224] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 7. | Heijl A, Leske MC, Bengtsson B, Hyman L, Bengtsson B, Hussein M; Early Manifest Glaucoma Trial Group. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2002;120:1268-1279. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2103] [Cited by in F6Publishing: 2263] [Article Influence: 102.9] [Reference Citation Analysis (0)] |
| 8. | Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: a review. JAMA. 2014;311:1901-1911. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1848] [Cited by in F6Publishing: 2195] [Article Influence: 219.5] [Reference Citation Analysis (0)] |
| 9. | Cairns JE. Trabeculectomy. Preliminary report of a new method. Am J Ophthalmol. 1968;66:673-679. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 692] [Cited by in F6Publishing: 638] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 10. | Razeghinejad MR, Fudemberg SJ, Spaeth GL. The changing conceptual basis of trabeculectomy: a review of past and current surgical techniques. Surv Ophthalmol. 2012;57:1-25 [PMID: 22137574 DOI: 10.1016/j.survophthal.2011.07.005. [Cited in This Article: ] |
| 11. | Skuta GL. Parrish RK 2nd. Wound healing in glaucoma filtering surgery. Surv Ophthalmol. 1987;32:149-170. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 426] [Cited by in F6Publishing: 433] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 12. | Chang L, Crowston JG, Cordeiro MF, Akbar AN, Khaw PT. The role of the immune system in conjunctival wound healing after glaucoma surgery. Surv Ophthalmol. 2000;45:49-68. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 85] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 13. | Bindlish R, Condon GP, Schlosser JD, D'Antonio J, Lauer KB, Lehrer R. Efficacy and safety of mitomycin-C in primary trabeculectomy: five-year follow-up. Ophthalmology. 2002;109:1336-41; discussion 1341-2. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 234] [Cited by in F6Publishing: 232] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 14. | Beckers HJ, Kinders KC, Webers CA. Five-year results of trabeculectomy with mitomycin C. Graefes Arch Clin Exp Ophthalmol. 2003;241:106-110. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 104] [Cited by in F6Publishing: 117] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 15. | Cairns JE. Surgical treatment of primary open-angle glaucoma. Trans Ophthalmol Soc U K. 1972;92:745-756. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Addicks EM, Quigley HA, Green WR, Robin AL. Histologic characteristics of filtering blebs in glaucomatous eyes. Arch Ophthalmol. 1983;101:795-798. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 336] [Cited by in F6Publishing: 345] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 17. | Agrawal P, Bradshaw SE. Systematic Literature Review of Clinical and Economic Outcomes of Micro-Invasive Glaucoma Surgery (MIGS) in Primary Open-Angle Glaucoma. Ophthalmol Ther. 2018;7:49-73. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 87] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 18. | Feiner L, Piltz-Seymour JR; Collaborative Initial Glaucoma Treatment Study. Collaborative Initial Glaucoma Treatment Study: a summary of results to date. Curr Opin Ophthalmol. 2003;14:106-111. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 103] [Cited by in F6Publishing: 116] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 19. | Edmunds B, Thompson JR, Salmon JF, Wormald RP. The National Survey of Trabeculectomy. III. Early and late complications. Eye (Lond). 2002;16:297-303. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 195] [Cited by in F6Publishing: 188] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 20. | Fourman S. Effects of aminoproprionitrile on glaucoma filter blebs in rabbits. Ophthalmic Surg. 1988;19:649-652. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Law SK, Shih K, Tran DH, Coleman AL, Caprioli J. Long-term outcomes of repeat vs initial trabeculectomy in open-angle glaucoma. Am J Ophthalmol. 2009;148:685-695.e1. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 86] [Cited by in F6Publishing: 92] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 22. | Hu B, An HM, Wang SS, Chen JJ, Xu L. Preventive and Therapeutic Effects of Chinese Herbal Compounds against Hepatocellular Carcinoma. Molecules. 2016;21:142. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 23. | Lu XL, He SX, Ren MD, Wang YL, Zhang YX, Liu EQ. Chemopreventive effect of saikosaponin-d on diethylinitrosamine-induced hepatocarcinogenesis: involvement of CCAAT/enhancer binding protein β and cyclooxygenase-2. Mol Med Rep. 2012;5:637-644. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 24. | Rui W, Xie L, Liu X, He S, Wu C, Zhang X, Zhang L, Yang Y. Compound Astragalus and Salvia miltiorrhiza extract suppresses hepatocellular carcinoma progression by inhibiting fibrosis and PAI-1 mRNA transcription. J Ethnopharmacol. 2014;151:198-209. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 25. | Zhao T, Sun S, Zhang H, Huang X, Yan M, Dong X, Wen Y, Wang H, Lan HY, Li P. Therapeutic Effects of Tangshen Formula on Diabetic Nephropathy in Rats. PLoS One. 2016;11:e0147693. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 26. | Ding YF, Peng YR, Shen H, Shu L, Wei YJ. Gualou Xiebai decoction inhibits cardiac dysfunction and inflammation in cardiac fibrosis rats. BMC Complement Altern Med. 2016;16:49. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 27. | Chang RC, So KF. Use of anti-aging herbal medicine, Lycium barbarum, against aging-associated diseases. What do we know so far? Cell Mol Neurobiol. 2008;28:643-652. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 226] [Cited by in F6Publishing: 211] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 28. | Li HL, Ashpole NE, Navarro ID, Lam TC, Chan HL, To CH, Stamer WD, Do CW. Baicalein lowers intraocular pressure and increases outflow facility in mouse eye. Denver: Association for Research in Vision and Ophthalmology 2015; 4853-A0006. [Cited in This Article: ] |
| 29. | Man D, Huang Y, Zhang H. Effects observation of treating glaucoma by trabeculectomy plus TCM. Zhongyi Linchuang Yanjiu. 2011;14:1674-1680. [Cited in This Article: ] |
| 30. | Luo Q, Cai Y, Yan J, Sun M, Corke H. Hypoglycemic and hypolipidemic effects and antioxidant activity of fruit extracts from Lycium barbarum. Life Sci. 2004;76:137-149. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 312] [Cited by in F6Publishing: 288] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 31. | Sun ZK, Yang HQ, Chen SD. Traditional Chinese medicine: a promising candidate for the treatment of Alzheimer's disease. Transl Neurodegener. 2013;2:6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 63] [Article Influence: 5.7] [Reference Citation Analysis (0)] |