Copyright
©The Author(s) 2018.
World J Transplantation. Sep 10, 2018; 8(5): 122-141
Published online Sep 10, 2018. doi: 10.5500/wjt.v8.i5.122
Published online Sep 10, 2018. doi: 10.5500/wjt.v8.i5.122
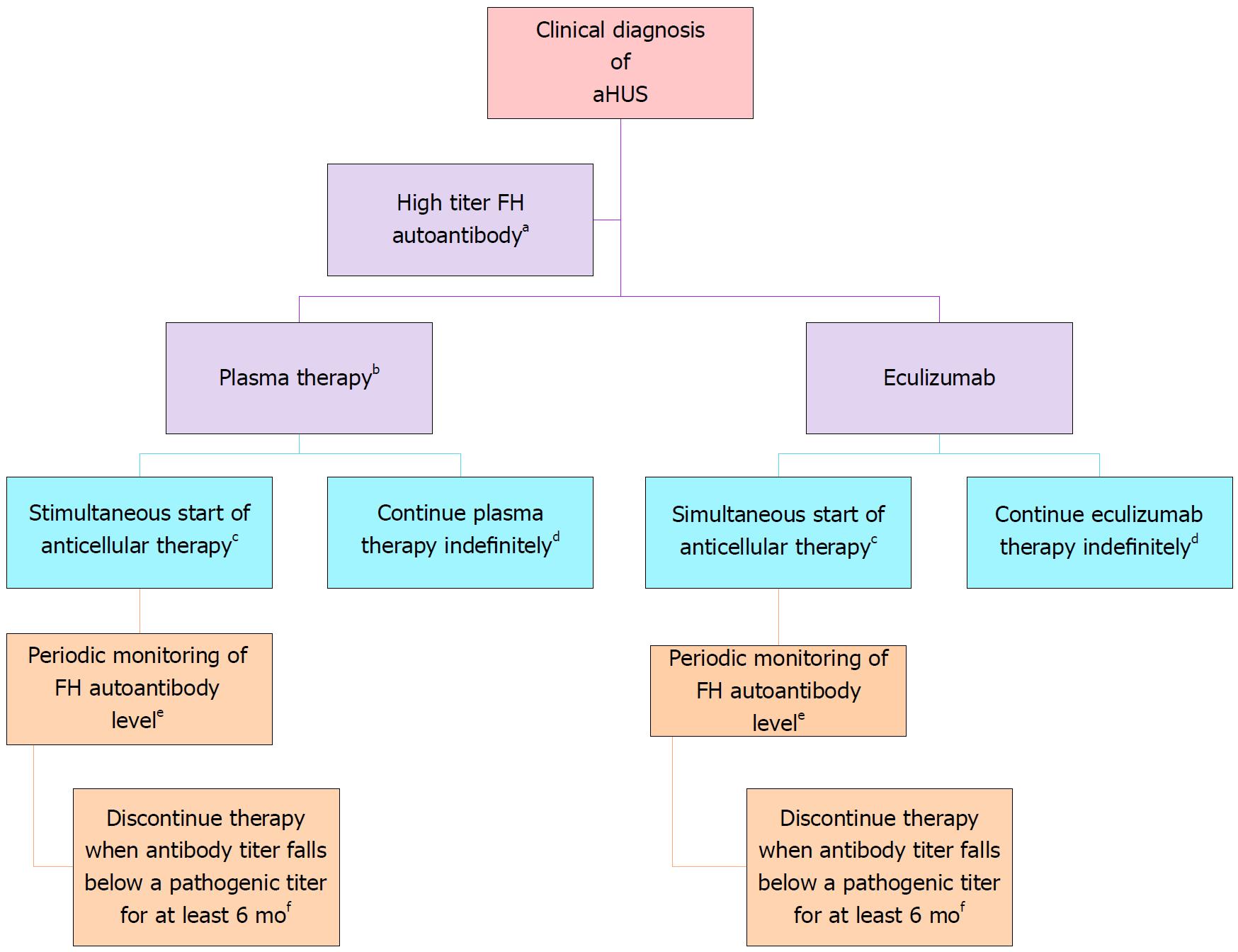
Figure 5 Treatment of complement factor H autoantibody-mediated atypical hemolytic uremic syndrome.
There are no prospective controlled studies in patients with atypical hemolytic uremic syndrome (aHUS) due to anti–factor H protein (FH) antibodies, and thus the proposed management is based on a pediatric consensus[84] (Adapted from: Goodship et al[58]). aAbnormal titer depends on the testing laboratory; bThe decision to use plasma therapy versus eculizumab will be based on patient age and local resource availability; cCyclophosphamide, rituximab, or mycophenolate mofetil; dThe decision to continue anticomplement therapy indefinitely is not informed by data; eThe interval may be monthly or quarterly and is based on local resources; fThis recommendation is based on limited retrospective case reviews[172-174].
- Citation: Abbas F, El Kossi M, Kim JJ, Sharma A, Halawa A. Thrombotic microangiopathy after renal transplantation: Current insights in de novo and recurrent disease. World J Transplantation 2018; 8(5): 122-141
- URL: https://www.wjgnet.com/2220-3230/full/v8/i5/122.htm
- DOI: https://dx.doi.org/10.5500/wjt.v8.i5.122