Copyright
©The Author(s) 2016.
World J Transplant. Mar 24, 2016; 6(1): 28-41
Published online Mar 24, 2016. doi: 10.5500/wjt.v6.i1.28
Published online Mar 24, 2016. doi: 10.5500/wjt.v6.i1.28
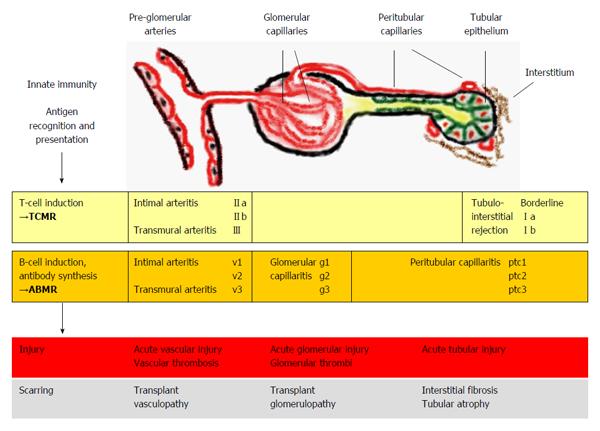
Figure 1 Kidney allograft rejection types, histological sites of injury and underlying mechanisms.
TCMR includes recognition and presentation of donor antigens by antigen-presenting cells to T cells, which become activated and undergo proliferation. Activated T-cells invade vascular, tubular and interstitial structures. Vascular rejection often presents with some degree of tubulointerstitial inflammation; however pure cases of vascular rejection (“v-only”) can be observed[8]. In ABMR, activated T cells induce B cells to undergo plasma cell proliferation resulting in the production of donor-specific antibodies. Antibody-mediated injury to pre-glomerular arteries, glomerular and peritubular capillaries is mediated by local activation of complement factors however, non-complement-fixing antibodies may also play a role in some cases[9]. Isolated findings of glomerular and peritubular capillaritis or pre-glomerular arteritis may be present or a combination of these features[7]. TCMR and ABMR can occur simultaneously (i.e., mixed rejection)[4]. The rejection processes can lead to different histological forms of injury and if not successfully treated, to scarring. The Banff classification[7] associates the elementary lesions of glomerular (g) and peritubular capillaries (ptc) and pre-glomerular vessels (v) to ABMR. TCMR includes tubulointerstitial infiltration (Borderline, I) and arteritis of pre-glomerular vessels (II-III). Banff grades (a-b, II-III, v1-3, g1-3, ptc1-3) denote different severities of the lesions. TCMR: T cell-mediated rejection; ABMR: Antibody-mediated rejection.
- Citation: Gwinner W, Metzger J, Husi H, Marx D. Proteomics for rejection diagnosis in renal transplant patients: Where are we now? World J Transplant 2016; 6(1): 28-41
- URL: https://www.wjgnet.com/2220-3230/full/v6/i1/28.htm
- DOI: https://dx.doi.org/10.5500/wjt.v6.i1.28