Copyright
©The Author(s) 2015.
World J Respirol. Nov 28, 2015; 5(3): 199-206
Published online Nov 28, 2015. doi: 10.5320/wjr.v5.i3.199
Published online Nov 28, 2015. doi: 10.5320/wjr.v5.i3.199
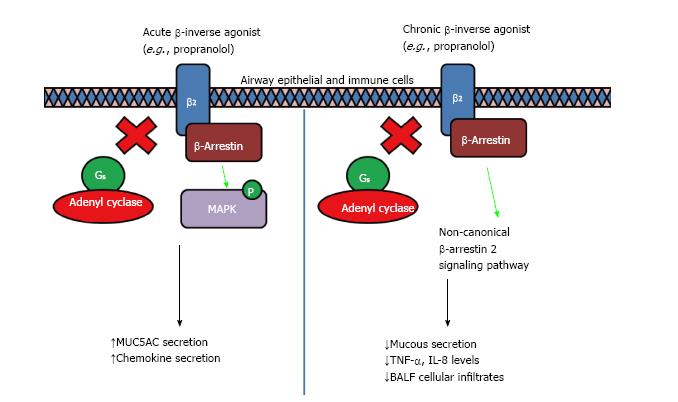
Figure 3 Acute and chronic inverse agonist treatment in obstructive airway diseases.
It was shown in cell and animal models that acute treatment of β-blockers induced a partial agonist response that led to an increase in MUC5AC production viaβ-arrestin2 which serves as a multi-protein scaffold, activating ERK1/2 and p38 mitogen-activated protein kinase (MAPK), resulting in mucus hypersecretion and increased airway resistance response to methacholine. However, chronic treatment of β-blockers led to a reduction in mucus secretion, decreased airway hyperresponsiveness and reduced inflammation, through the non-canonical β-arrestin2-mediated signaling induced by inverse agonism of β2-adrenoceptors[46]. The differential response could be due to the binding of ligand to a shallower secondary binding site exposed only when an adequate conformational state is obtained as proposed by Soriano-Ursúa et al[44], however more work need to be done to validate the mechanism.
- Citation: Tan DW, Wong JL, Tie ST, Abisheganaden JA, Lim AY, Wong WF. β2-adrenoceptor in obstructive airway diseases: Agonism, antagonism or both? World J Respirol 2015; 5(3): 199-206
- URL: https://www.wjgnet.com/2218-6255/full/v5/i3/199.htm
- DOI: https://dx.doi.org/10.5320/wjr.v5.i3.199