Copyright
©2014 Baishideng Publishing Group Inc.
World J Hepatol. Aug 27, 2014; 6(8): 580-595
Published online Aug 27, 2014. doi: 10.4254/wjh.v6.i8.580
Published online Aug 27, 2014. doi: 10.4254/wjh.v6.i8.580
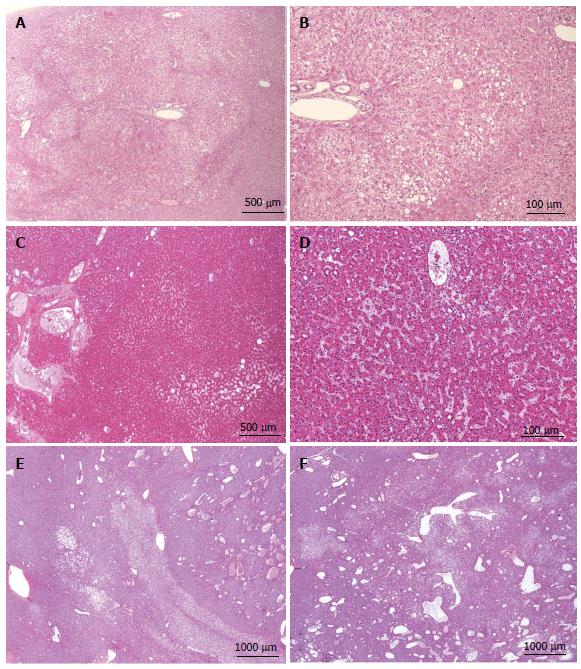
Figure 7 HNF1a inactivated hepatocellular adenoma microscopic atypical feature.
A, B: Woman born in 1952; abnormal liver function tests; oral contraceptives 13 years; BMI 25.4; magnetic resonance imaging (MRI): adenomatosis, largest nodule 6 cm. Segmentectomy IV/VI in 2001. A: ill defined nodule composed of clear hepatocytes, with mild steatosis. B: Same nodule seen at a higher magnification. The normal portal tract from the periphery of non tumoral parenchyma is entrapped in the nodule. The diagnosis of HNF1A mutated hepatocellular adenoma (H-HCA) is less evident than in Figure 6B, C. The diagnosis was confirmed by immunohistochemistry. C, D: Woman born in 1950; abnormal liver function tests; imaging: probable FNH 12 cm. Right hepatectomy 2002. HE: proliferation of benign hepatocytes, no steatosis, mild sinusoidal dilatation. This is a rare case. The diagnosis of H-HCA cannot be suspected without performing immunohistochemistry. E, F: Woman born in 1965; past history of cancer. Abdominal pain. Oral contraceptives 10 years, BMI 21 kg/m2. MRI: Adenomatosis, largest nodule 3.9 cm. Segmentectomy and tumorectomy in 2011. HE: Proliferation of benign hepatocytes, no steatosis, mild sinusoidal dilatation, numerous ectatic vessels. As above, in this rare case the diagnosis of H-HCA cannot be suspected without immunohistochemistry, and malignant transformation has to be ruled out.
- Citation: Sempoux C, Balabaud C, Bioulac-Sage P. Pictures of focal nodular hyperplasia and hepatocellular adenomas. World J Hepatol 2014; 6(8): 580-595
- URL: https://www.wjgnet.com/1948-5182/full/v6/i8/580.htm
- DOI: https://dx.doi.org/10.4254/wjh.v6.i8.580